
Medical Indemnity Act 2002
No. 132, 2002
An Act to make provision in relation to indemnities in relation to the practice of medical professions and vocations, and for related purposes

Medical Indemnity Act 2002
No. 132, 2002
An Act to make provision in relation to indemnities in relation to the practice of medical professions and vocations, and for related purposes
Contents
Part 1—Preliminary
1 Short title...................................
2 Commencement...............................
3 Objects of this Act and the medical indemnity contribution legislation
4 Definitions..................................
5 Medical defence organisation (MDO)..................
6 Member of an MDO.............................
7 Incident‑occurring based cover.................
8 IBNR exposure of an MDO........................
9 External Territories.............................
Part 2—Commonwealth payments
Division 1—IBNR (incurred but not reported) indemnity scheme
Subdivision A—Introduction
10 Guide to the IBNR indemnity provisions.................
Subdivision B—Participating MDOs
11 Participating MDO.............................
12 Minister may determine that MDO not a participating MDO.....
13 Process for determining whether a determination should be made under section 12
Subdivision C—Incidents covered by the IBNR indemnity scheme
14 Incidents covered by the IBNR indemnity scheme...........
Subdivision D—IBNR indemnity
15 IBNR indemnity may be payable under either section 16 or 17....
16 IBNR indemnity for payment made by MDO or insurer........
17 IBNR indemnity for MDO or insurer in external administration...
18 Clarification of circumstances in which IBNR indemnity payable..
19 Exceptions..................................
20 Payment partly related to treatment of public patient in public hospital
21 Amount of the IBNR indemnity......................
22 Minister to determine unfunded IBNR factor for a participating MDO
23 Process for determining unfunded IBNR factor under section 22...
Subdivision E—Recovery of amount paid to MDO or insurer after IBNR indemnity paid
24 Recovery if certain amounts paid to MDO or insurer after IBNR indemnity paid
25 MDO or insurer to inform HIC of certain amounts...........
26 HIC to notify MDO or insurer of repayable amount..........
27 Penalty imposed if an amount is repaid late...............
Division 2—High cost claim indemnity scheme
Subdivision A—Introduction
28 Guide to the high cost claim indemnity provisions...........
29 High cost claim threshold..........................
Subdivision B—High cost claim indemnity
30 Circumstances in which high cost claim indemnity payable......
31 Aggregating amounts paid or payable by an MDO and insurer....
32 Exceptions..................................
33 Payment partly related to treatment of public patient in public hospital
34 Amount of high cost claim indemnity..................
Division 3—Administration of the indemnity schemes
Subdivision A—Introduction
35 Guide to this Division............................
Subdivision B—Applications for, and payment of, indemnity scheme payments
36 Application for indemnity scheme payment...............
37 Payment date for indemnity scheme payment..............
Subdivision C—Information gathering and record keeping
38 HIC may request information.......................
39 MDOs and insurers to keep relevant records...............
40 Participating MDOs to keep additional records.............
Subdivision D—Overpayments of the indemnities
41 Recovery of overpayments.........................
Subdivision E—Recovery of repayment or overpayment debt
42 HIC may collect money from a person who owes money to a person
Division 4—Medical indemnity premium subsidy scheme
43 Minister may formulate subsidy scheme.................
44 HIC may request information.......................
Division 5—Offences
45 Failing to give information.........................
46 Failing to notify...............................
47 Failing to keep and retain records.....................
Division 6—Finance
48 Appropriation................................
Division 7—Reinsurance contracts
49 Indemnity scheme payments disregarded for purposes of reinsurance contracts
Part 3—Contributions towards the cost of providing indemnities
Division 1—IBNR (incurred but not reported) indemnity contribution
Subdivision A—Introduction
50 Guide to the IBNR indemnity contribution provisions.........
Subdivision B—Who pays IBNR indemnity contribution
51 Who is liable to pay the IBNR indemnity contribution.........
52 Exemptions..................................
53 Comprehensive insurance cover determination.............
Subdivision C—Determining amount of IBNR indemnity contribution
54 Annual subscription for base year.....................
Subdivision D—Annual reassessment of participating MDO’s IBNR exposure
55 Object of this Subdivision.........................
56 Process for annually reassessing IBNR exposure............
Division 2—Enhanced UMP indemnity contribution
Subdivision A—Introduction
57 Guide to the enhanced UMP indemnity contribution provisions...
Subdivision B—Who pays enhanced UMP indemnity contribution
58 Who is liable to pay the enhanced UMP indemnity contribution...
59 Exemptions..................................
Division 3—Administration of the medical indemnity contributions
Subdivision A—Introduction
60 Guide to this Division............................
Subdivision B—Payment and collection of medical indemnity contributions
61 When medical indemnity contribution must be paid..........
62 Deferral of payment day for medical indemnity contribution.....
63 Medical indemnity contribution may be paid by instalments.....
64 Discount for lump sum payment of medical indemnity contribution.
65 Late payment penalty............................
66 Method of paying certain amounts....................
Subdivision C—Refunds
67 Refund of overpaid amounts........................
Subdivision D—Recovery of contribution debt
68 Recovery of contribution debt.......................
69 HIC may collect money from a person who owes money to a person
70 Evidentiary certificates...........................
Subdivision E—Information gathering processes
71 HIC may request information.......................
72 HIC must be notified of a change in circumstances etc.........
Division 4—Offences
73 Failing to give information.........................
74 Failing to notify...............................
Part 4—Miscellaneous
75 General administration of this Act and medical indemnity contribution legislation
76 Additional functions of the HIC......................
77 Officers to observe secrecy.........................
78 Act not to apply in relation to State insurance within a State.....
79 Regulations..................................

Medical Indemnity Act 2002
No. 132, 2002
An Act to make provision in relation to indemnities in relation to the practice of medical professions and vocations, and for related purposes
[Assented to 19 December 2002]
The Parliament of Australia enacts:
This Act may be cited as the Medical Indemnity Act 2002.
This Act commences, or is taken to have commenced, on 1 January 2003.
3 Objects of this Act and the medical indemnity contribution legislation
(1) An object of this Act is to contribute towards the availability of medical services in Australia by providing Commonwealth assistance to support access by medical practitioners to arrangements that indemnify them for claims arising in relation to their practice of their medical professions.
(2) The Commonwealth provides that assistance under this Act by:
(a) meeting part of the costs of large settlements or awards paid by organisations that indemnify medical practitioners (but only for claims notified on or after 1 January 2003); and
(b) providing for a subsidy scheme to help certain medical practitioners meet the cost of their indemnity arrangements; and
(c) meeting the cost associated with certain IBNR liabilities of organisations that indemnify medical practitioners to the extent to which those organisations had not made adequate provision for those liabilities as at 30 June 2002.
Note: The acronym “IBNR” is used in this Act for “incurred but not reported”.
(3) The Commonwealth provides further assistance in relation to members and former members of UMP under a Medical Indemnity Agreement referred to in the Medical Indemnity Agreement (Financial Assistance—Binding Commonwealth Obligations) Act 2002.
(4) Another object of this Act (together with the medical indemnity contribution legislation) is to allow the Commonwealth:
(a) to recover the costs of providing the assistance referred to in paragraph (2)(c) by requiring contributions from persons who were members of relevant organisations on 30 June 2000; and
(b) to recover the cost of providing some of the assistance referred to in subsection (3) by requiring contributions from persons who were members of UMP on 1 July 2002.
General
(1) In this Act, unless the contrary intention appears:
Actuary means the Australian Government Actuary.
claim:
(a) means a claim or demand of any kind (whether or not involving legal proceedings); and
(b) includes proceedings of any kind including:
(i) proceedings before an administrative tribunal or of an administrative nature; and
(ii) disciplinary proceedings (including disciplinary proceedings conducted by or on behalf of a professional body); and
(iii) an inquiry or investigation;
and claim against a person includes an inquiry into, or an investigation of, the person’s conduct.
contribution year:
(a) for an IBNR indemnity contribution payable by a participating member of a participating MDO—has the same meaning as in the Medical Indemnity (IBNR Indemnity) Contribution Act 2002; and
(b) for an enhanced UMP indemnity contribution—has the same meaning as in the Medical Indemnity (Enhanced UMP Indemnity) Contribution Act 2002.
externally‑administered body corporate means:
(a) a body corporate that is an externally‑administered body corporate within the meaning of the Corporations Act 2001; or
(b) a body corporate to which a provisional liquidator has been appointed.
health care related vocation means a health care related vocation that a person must be registered under a State or Territory law to practise.
health professional means a person who practises a health care related vocation.
HIC means the Health Insurance Commission.
high cost claim threshold has the meaning given by section 29.
IBNR exposure has the meaning given by section 8.
imposition day:
(a) for an IBNR indemnity contribution payable by a participating member of a participating MDO—has the same meaning as in the Medical Indemnity (IBNR Indemnity) Contribution Act 2002; and
(b) for an enhanced UMP indemnity contribution—has the same meaning as in the Medical Indemnity (Enhanced UMP Indemnity) Contribution Act 2002.
incident includes:
(a) any act, omission or circumstance; and
(b) an incident that is claimed to have occurred.
incident‑occurring based cover has the meaning given by section 7.
indemnify has a meaning affected by subsection (2).
indemnity scheme payment means:
(a) an IBNR indemnity paid or payable under Division 1 of Part 2; or
(b) a high cost claim indemnity paid or payable under Division 2 of Part 2.
insurance business has the same meaning as in the Insurance Act 1973.
insurer means a person who carries on insurance business.
insurer‑to‑insurer payment means a payment that:
(a) is made by an MDO or insurer to an MDO or an insurer; and
(b) is not made by the MDO or insurer on behalf of another person.
late payment penalty:
(a) in relation to an amount repayable under section 24—means a penalty payable under section 27; and
(b) in relation to a medical indemnity contribution or a lump sum payable under section 64—means a penalty payable under section 65.
Managing Director means the Managing Director of the HIC.
MDO has the meaning given by section 5.
medical indemnity contribution means:
(a) an IBNR indemnity contribution payable under Division 1 of Part 3; or
(b) an enhanced UMP indemnity contribution payable under Division 2 of Part 3.
medical indemnity contribution legislation means:
(a) the Medical Indemnity (IBNR Indemnity) Contribution Act 2002; or
(b) the Medical Indemnity (Enhanced UMP Indemnity) Contribution Act 2002.
medical practitioner means a person registered or licensed as a medical practitioner under a State or Territory law that provides for the registration or licensing of medical practitioners.
medical profession includes a health care related vocation.
medicare benefit means a medicare benefit payable under Part II of the Health Insurance Act 1973.
member of an MDO has the meaning given by section 6.
participating MDO has the meaning given by section 11.
participating member of a participating MDO means a person who was a member of the MDO on 30 June 2000 (whether or not the person ceased to be a member of the MDO after that date).
payment made in relation to a claim has the meaning given by subsections (3) and (4).
provable: an amount that an MDO or insurer is liable to pay is provable if:
(a) it is provable in the winding up of the MDO or insurer if the winding up of the MDO or insurer has commenced; or
(b) it would be provable in the winding up of the MDO or insurer if the MDO or insurer were to be wound up.
public hospital means a recognised hospital within the meaning of the Health Insurance Act 1973.
public patient has the same meaning as in the Health Insurance Act 1973.
related body corporate has the same meaning as in the Corporations Act 2001.
Secretary means the Secretary of the Department.
UMP means United Medical Protection Limited.
unfunded IBNR exposure: an MDO has an unfunded IBNR exposure on 30 June 2002 if the MDO had, on that day, insufficient readily available assets to cover both its IBNR exposure and all its other liabilities.
unfunded IBNR factor for a participating MDO means the factor for the MDO worked out under section 22.
Indemnifying
(2) To avoid doubt, a person may, for the purposes of this Act, indemnify someone else by either:
(a) making a payment; or
(b) agreeing to make a payment.
Note: A person may indemnify someone else by making a payment even if the payment was not preceded by an agreement to pay.
Payments in relation to claims
(3) For the purposes of this Act:
(a) a payment is made in relation to a claim against a person if and only if the payment is made to:
(i) satisfy or settle the claim; or
(ii) meet legal and other expenses that are directly attributable to any negotiations, arbitration or proceedings in relation to the claim; and
(b) a payment is made in relation to a claim by a person if and only if the payment is made to meet legal and other expenses that are directly attributable to any negotiations, arbitration or proceedings in relation to the claim.
(4) A reference in this Act to a payment being made to satisfy or settle a claim against a person includes a reference to a payment that:
(a) is made to reimburse the person for a payment the person has made to satisfy or settle the claim; or
(b) is made to the person so that the person can make a payment to satisfy or settle the claim.
Changes in body corporate names
(5) A reference in this Act to a body corporate by a particular name is a reference to the body corporate that had that name on 30 June 2002.
5 Medical defence organisation (MDO)
(1) An MDO is a body corporate that is an MDO under subsection (2) or (3) or regulations made for the purposes of subsection (4).
(2) Subject to regulations made for the purposes of subsection (5), a body corporate is an MDO if:
(a) the body corporate is incorporated by or under a law of the Commonwealth, a State or a Territory; and
(b) the body corporate was in existence on 30 June 2002; and
(c) the body corporate, in the ordinary course of its business as at 30 June 2002, indemnified persons in relation to claims in relation to incidents that occurred in the course of, or in connection with, the practice of a medical profession by the persons; and
(d) did so only if the persons were one of the following:
(i) members or former members of the body corporate;
(ii) the legal personal representatives of members or former members of the body corporate.
This is so even if the indemnity is one that is provided at the body corporate’s discretion.
(3) Subject to regulations made for the purposes of subsection (5), each of the bodies corporate listed in the following table is an MDO:
MDOs |
Medical Defence Association of South Australia Limited |
Medical Defence Association of Victoria Limited |
Medical Defence Association of Western Australia (Incorporated) |
Medical Indemnity Protection Society Limited |
Medical Protection Society of Tasmania Inc. |
Queensland Doctors Mutual Limited |
United Medical Protection Limited |
(4) The regulations may provide that a body corporate specified in the regulations is an MDO.
(5) The regulations may provide that a body corporate specified in the regulations is not an MDO for the purposes of this Act.
(1) A person is a member of an MDO:
(a) at all times when the person is a member of the MDO according to the MDO’s constitution; and
(b) no matter how the person’s membership is described.
(2) Without limiting paragraph (1)(a), a person does not cease to be a member of an MDO merely because some or all of the person’s rights and privileges as a member are suspended, have lapsed or have ceased.
(3) Without limiting paragraph (1)(b), a person is a member of an MDO even if the person is described by the MDO’s constitution as:
(a) an associate member; or
(b) an honorary member; or
(c) a non‑financial member; or
(d) a retired member; or
(e) a student member.
7 Incident‑occurring based cover
(1) A person had incident‑occurring based cover for an incident with an MDO on 30 June 2002 if:
(a) an arrangement between the MDO and the person, or between the MDO and someone else, existed on 30 June 2002; and
(b) under the arrangement, the MDO:
(i) would have been able to indemnify the person in relation to the incident if the person were to make a proper claim after 30 June 2002 in relation to the incident; and
(ii) would have been able, in the ordinary course of its business, to indemnify the person in relation to the incident even if the person had ceased to be a member of the MDO when the claim was made.
The person need not have been a member of the MDO on 30 June 2002 to have incident‑occurring based cover for the incident.
Note: Subparagraph (b)(ii)—If the only cover the person had with the MDO was claims made cover, it would not be in the ordinary course of the MDO’s business to indemnify the person if the claim was made after the person had ceased to be a member of the MDO.
(2) Subparagraph (1)(b)(i) is satisfied even if the MDO would be able to indemnify the person in relation to the incident only if the person were to make a claim during a limited period after 30 June 2002.
(3) To avoid doubt, cover may be incident‑occurring based cover even if it is called:
(a) claims incurred cover; or
(b) extended reporting benefit cover (ERB cover); or
(c) death, disability or retirement cover (DDR cover).
(1) An MDO’s IBNR exposure at a particular time is the total amount, at that time, of the payments that the MDO is likely to have to make after that time in relation to all claims that relate to incidents that satisfy subsection (2).
(2) An incident satisfies this subsection if:
(a) the incident occurred on or before 30 June 2002; and
(b) the incident occurred in the course of, or in connection with, the practice of a medical profession by a person; and
(c) on 30 June 2002, the person had incident‑occurring based cover with the MDO for the incident; and
(d) on 30 June 2002, the MDO:
(i) was not aware of the occurrence of the incident; and
(ii) was not aware of any claim against or by the person in relation to the incident.
This Act extends to every external Territory.
Division 1—IBNR (incurred but not reported) indemnity scheme
10 Guide to the IBNR indemnity provisions
(1) This Division provides that an IBNR indemnity may be paid to an MDO or insurer that makes, or is liable to make, a payment in relation to a claim against or by a person in relation to an incident that is covered by the IBNR indemnity scheme. The incident will only be covered by the scheme if, amongst other things, the person had incident‑occurring based cover with an MDO for the incident on 30 June 2002 and the MDO is a participating MDO.
(2) The following table tells you where to find the provisions dealing with various issues:
Where to find the provisions on various issues | ||
Item | Issue | Provisions |
1 | which MDOs are participating MDOs? | sections 11 to 13 |
2 | which incidents are covered by the scheme? | section 14 |
3 | what conditions must be satisfied for an MDO or insurer to get the IBNR indemnity? | sections 15 to 19 |
4 | what happens if the incidents occurred during the treatment of a public patient in a public hospital? | paragraph 19(a) and section 20 |
5 | how much is the IBNR indemnity? | sections 21 to 23 |
6 | in what circumstances can a payment to an MDO or insurer lead to a repayment of the IBNR indemnity? | sections 24 to 27 |
7 | how do MDOs and insurers apply for the IBNR indemnity? | section 36 |
8 | when will the IBNR indemnity be paid? | section 37 |
9 | what information has to be provided to the HIC about IBNR indemnity matters? | section 38 |
10 | what records must MDOs and insurers keep? | sections 39 and 40 |
11 | how are overpayments of the IBNR indemnity, and indemnity repayments, recovered? | sections 41 and 42 |
Subdivision B—Participating MDOs
(1) An MDO is a participating MDO unless:
(a) the MDO was not in existence on 30 June 2002; or
(b) the Minister determines under section 12 that the MDO is not a participating MDO.
(2) If the Minister makes a determination that an MDO is not a participating MDO, the MDO is taken never to have been a participating MDO.
12 Minister may determine that MDO not a participating MDO
(1) The Minister may determine that an MDO is not a participating MDO.
(2) In deciding whether to make a determination under subsection (1) in relation to an MDO, the Minister must have regard to:
(a) whether the MDO had an unfunded IBNR exposure on 30 June 2002; and
(b) any other matter the Minister considers relevant.
For the purposes of paragraph (a), the Minister is to have regard to the consolidated financial position of the MDO and the entities it controls.
(3) Before making the determination under subsection (1), the Minister must consider a report from the Actuary on whether the MDO had an unfunded IBNR exposure on 30 June 2002.
(4) The Minister must give a copy of the determination to the MDO within 28 days after the day on which it is made.
(5) A determination under subsection (1) is a disallowable instrument for the purposes of section 46A of the Acts Interpretation Act 1901.
13 Process for determining whether a determination should be made under section 12
Report by the Actuary
(1) The Actuary must give the Minister a written report in relation to each MDO that was in existence on 30 June 2002 that:
(a) states whether the Actuary considers that the MDO had an unfunded IBNR exposure on 30 June 2002; and
(b) sets out the reasons for the statement.
(2) In preparing the report, the Actuary must take into account any information that the HIC gives the Actuary in relation to the MDO under subsection (6).
HIC’s information gathering powers
(3) If the HIC believes on reasonable grounds that the MDO is capable of giving information that is relevant to determining whether the MDO had an unfunded IBNR exposure on 30 June 2002, the HIC may request the MDO to give the HIC the information.
Note: Failure to comply with the request is an offence (see section 45).
(4) The request:
(a) must be made in writing; and
(b) must state what information the MDO must give to the HIC; and
(c) may require the information to be verified by statutory declaration; and
(d) must specify a day on or before which the information must be given; and
(e) must contain a statement to the effect that a failure to comply with the request is an offence.
The day specified under paragraph (d) must be at least 28 days after the day on which the request is made.
(5) Without limiting subsection (3), the kind of information that may be requested includes information in the form of:
(a) financial statements; and
(b) a report prepared by a suitably qualified actuary on whether the MDO had an unfunded IBNR exposure on 30 June 2002.
(6) The HIC must give any information the MDO gives the HIC to the Actuary for the purposes of preparing the report for the Minister under subsection (1).
Subdivision C—Incidents covered by the IBNR indemnity scheme
14 Incidents covered by the IBNR indemnity scheme
The IBNR indemnity scheme covers an incident if:
(a) the incident occurred on or before 30 June 2002; and
(b) the incident occurred in the course of, or in connection with, the practice of a medical profession by a person; and
(c) on 30 June 2002, the person had incident‑occurring based cover with an MDO for the incident; and
(d) on 30 June 2002, the MDO:
(i) was not aware of the occurrence of the incident; and
(ii) was not aware of any claim against or by the person in relation to the incident; and
(e) the MDO is a participating MDO.
15 IBNR indemnity may be payable under either section 16 or 17
(1) An IBNR indemnity may be payable to an MDO or insurer under either section 16 or 17.
(2) To avoid doubt, an IBNR indemnity may be payable to an MDO or insurer under section 16 even if the MDO or insurer is an externally‑administered body corporate.
(3) An IBNR indemnity is not payable to an MDO or insurer under section 16 in relation to a payment the MDO or insurer makes to discharge a liability in relation to a claim if an IBNR indemnity is paid to the MDO or insurer under section 17 in relation to the same liability.
16 IBNR indemnity for payment made by MDO or insurer
Basic payability rule
(1) An IBNR indemnity is payable to an MDO or insurer under this section if:
(a) the MDO or insurer makes a payment in relation to a claim against or by a person (the practitioner); and
(b) the claim relates to:
(i) an incident that is covered by the IBNR indemnity scheme (see section 14); or
(ii) a series of related incidents that includes an incident that is covered by the scheme; and
(c) the practitioner had, on 30 June 2002, incident‑occurring based cover with an MDO for the incident that is covered by the IBNR indemnity scheme and that MDO is a participating MDO; and
(d) if it is an MDO that makes the payment—the MDO makes the payment:
(i) consistently with its constitution and the indemnity arrangement between the MDO and the practitioner; and
(ii) in the ordinary course of its business; and
(e) if it is an insurer that makes the payment—the insurer makes the payment:
(i) consistently with the terms of the insurance contract between the insurer and the practitioner; and
(ii) in the ordinary course of its business; and
(f) the MDO or insurer applies to the HIC for the IBNR indemnity in accordance with section 36.
The MDO mentioned in paragraph (c) is referred to as the relevant participating MDO.
(2) Subsection (1) has effect subject to:
(a) subsections (5) and (6) of this section; and
(b) subsection 15(3); and
(c) sections 19 and 20.
Basis on which payment made
(3) The IBNR indemnity is payable to the MDO or insurer regardless of the basis on which the payment is made by the MDO or insurer.
Note: If the criteria for the indemnity set out in subsection (1) are met, the indemnity may be payable to the MDO or insurer even if the MDO or insurer pays the practitioner on the basis of claims made cover the practitioner has with the MDO or insurer.
Payer need not be the relevant participating MDO
(4) If the payment is made by an MDO, the MDO that makes the payment may be the relevant participating MDO or may be a different MDO.
Payment by relevant participating MDO
(5) If the payment is made by the relevant participating MDO, the IBNR indemnity is payable only if the relevant participating MDO:
(a) makes the payment; or
(b) could have made the payment;
in relation to the claim in relation to the incident covered by the IBNR indemnity scheme on the basis of incident‑occurring based cover the practitioner had with the relevant participating MDO for the incident on 30 June 2002.
Payment by someone else
(6) If the payment is not made by the relevant participating MDO, the IBNR indemnity is payable only if the relevant participating MDO could have made the payment in relation to the claim in relation to the incident covered by the IBNR indemnity scheme:
(a) consistently with its constitution and the indemnity arrangement between the MDO and the practitioner; and
(b) in the ordinary course of its business; and
(c) on the basis of incident‑occurring based cover the practitioner had with the participating MDO on 30 June 2002;
if the practitioner made a proper claim in relation to the incident.
17 IBNR indemnity for MDO or insurer in external administration
Basic payability rule
(1) An IBNR indemnity is payable under this section to an MDO or insurer that is an externally‑administered body corporate if:
(a) the MDO or insurer is liable to pay an amount in relation to a claim against or by a person (the practitioner); and
(b) the claim relates to:
(i) an incident that is covered by the IBNR indemnity scheme (see section 14); or
(ii) a series of related incidents that includes an incident that is covered by the scheme; and
(c) the practitioner had, on 30 June 2002, incident‑occurring based cover with an MDO for the incident that is covered by the IBNR indemnity scheme and that MDO is a participating MDO; and
(d) the amount that the MDO or insurer is liable to pay is provable; and
(e) if it is an MDO that is liable to pay the amount—the MDO could pay the amount:
(i) consistently with its constitution and the indemnity arrangement between the MDO and the practitioner; and
(ii) in the ordinary course of its business;
if it were not an externally‑administered body corporate; and
(f) if it is an insurer that is liable to make the payment—the insurer could make the payment:
(i) consistently with the terms of the insurance contract between the insurer and the practitioner; and
(ii) in the ordinary course of its business;
if it were not an externally‑administered body corporate; and
(g) the MDO or insurer applies to the HIC for the IBNR indemnity in accordance with section 36.
The MDO mentioned in paragraph (c) is referred to as the relevant participating MDO.
(2) Subsection (1) has effect subject to:
(a) subsections (5) and (6) of this section; and
(b) sections 19 and 20.
Basis for liability to pay
(3) The IBNR indemnity is payable to the MDO or insurer regardless of the basis on which the amount is payable by the MDO or insurer.
Note: If the criteria for the indemnity set out in subsection (1) are met, the indemnity may be payable to the MDO or insurer even if the MDO or insurer is liable to pay on the basis of claims made cover the practitioner has with the MDO or insurer.
Person liable to pay need not be relevant participating MDO
(4) If an MDO is liable to pay the amount, the MDO that is liable to pay the amount may be the relevant participating MDO or may be a different MDO.
Relevant participating MDO liable to pay
(5) If the amount is one that the relevant participating MDO is liable to pay, the IBNR indemnity is payable only if the relevant participating MDO could have paid the amount in relation to the claim in relation to the incident covered by the IBNR indemnity scheme on the basis of incident‑occurring based cover the practitioner had with the relevant participating MDO on 30 June 2002.
Someone else liable to pay
(6) If the amount is not one that the relevant participating MDO is liable to pay, the IBNR indemnity is payable only if the relevant participating MDO could have paid an amount in relation to the claim in relation to the incident covered by the IBNR indemnity scheme:
(a) consistently with its constitution and the indemnity arrangement between the relevant participating MDO and the practitioner; and
(b) in the ordinary course of its business; and
(c) on the basis of incident‑occurring based cover the practitioner had with the relevant participating MDO on 30 June 2002;
if the practitioner made a proper claim in relation to the incident.
Indemnity to be paid on trust
(7) An IBNR indemnity paid to an MDO or insurer under this section is paid on trust for the benefit of the person to whom the MDO or insurer is liable to make the payment referred to in paragraph (1)(a).
18 Clarification of circumstances in which IBNR indemnity payable
An IBNR indemnity is payable to an MDO or insurer under section 16 or 17 in relation to a payment the MDO or insurer makes, or is liable to make, in relation to a claim even if:
(a) the MDO or insurer:
(i) has insured itself in relation to the payment; or
(ii) has already in fact been paid an amount by an insurer in relation to the payment; or
(b) the incident to which the claim relates occurred outside Australia; or
(c) the MDO or insurer made, or became liable to make, the payment before the commencement of this Act.
An IBNR indemnity is not payable to an MDO or insurer under section 16 or 17 in relation to a payment the MDO or insurer makes, or is liable to make, in relation to a claim against a person if:
(a) the incident, or all the incidents, to which the claim relates occurred in the course of the provision of treatment to a public patient in a public hospital; or
(b) a determination by the HIC is in force under section 53 in relation to the person; or
(c) the payment is an insurer‑to‑insurer payment; or
(d) the payment is a payment prescribed by the regulations for the purposes of this section.
20 Payment partly related to treatment of public patient in public hospital
(1) This section applies if:
(a) an MDO or insurer makes, or is liable to make, a payment in relation to a claim against a person in relation to a series of related incidents; and
(b) some, but not all, of the incidents occurred in the course of the provision of treatment to a public patient in a public hospital.
(2) For the purposes of this Subdivision:
(a) the payment is to be disregarded to the extent to which it relates to, or is reasonably attributable to, the incident or incidents that occurred in the course of the provision of treatment to a public patient in a public hospital; and
(b) any amount that is paid or payable to the MDO or insurer in relation to the payment is to be disregarded to the extent to which it relates to, or is reasonably attributable to, the incident or incidents that occurred in the course of the provision of treatment to a public patient in a public hospital.
Note: Paragraph (b)—see subsection 21(2).
21 Amount of the IBNR indemnity
(1) The amount of the IBNR indemnity is the amount worked out using the following formula:
![]()
where:
adjusted amount of the payment has the meaning given by subsection (2).
relevant participating MDO’s unfunded IBNR factor is the unfunded IBNR factor (see section 22) for the MDO referred to in paragraph 16(1)(c) or 17(1)(c).
Note: In certain circumstances, an amount may be repayable under section 24.
(2) The adjusted amount of the payment is the amount obtained by deducting from the amount the MDO or insurer pays, or is liable to pay, the amount, or the sum of the amounts, that are:
(a) paid; or
(b) payable and liquidated at the time the amount of the IBNR indemnity is worked out;
to the MDO or insurer in relation to the payment the MDO or insurer makes or is liable to make.
(3) Without limiting subsection (2), the amounts to be deducted under that subsection include:
(a) any high cost claim indemnity that is paid or payable to the MDO or insurer in relation to the payment the MDO or insurer makes or is liable to make; and
(b) any amount that is paid or payable to the MDO or insurer because of a right to which the MDO or insurer is subrogated; and
(c) the amount of any payment prescribed by the regulations.
(4) The following amounts are not to be deducted under subsection (2):
(a) any amount that is paid or payable to the MDO or insurer by way of an insurer‑to‑insurer payment;
(b) any amount that is paid or payable to the MDO or insurer by way of membership subscription or insurance premium;
(c) any amount that is payable under this Division;
(d) the amount of any payment prescribed by the regulations.
22 Minister to determine unfunded IBNR factor for a participating MDO
(1) A participating MDO’s unfunded IBNR factor is:
(a) 0 if a determination under paragraph (b) is not in force; or
(b) the factor determined in writing by the Minister for the participating MDO.
The factor determined by the Minister is to be between 0 and 1.
(2) The Minister may not vary or revoke a determination made under paragraph (1)(b).
(3) In making a determination under paragraph (1)(b), the Minister must have regard to:
(a) the extent to which the MDO had, on 30 June 2002, insufficient readily available assets to cover the amount the Minister considers to be its IBNR exposure after satisfying all its other liabilities; and
(b) such other matters as the Minister considers relevant.
For the purposes of paragraph (a), the Minister is to have regard to the consolidated financial position of the MDO and the entities it controls.
(4) Before making a determination under paragraph (1)(b) in relation to a participating MDO, the Minister must consider a report from the Actuary on the factor that should be specified as the MDO’s unfunded IBNR factor.
(5) The Minister must give a copy of the determination to the participating MDO within 28 days after the day on which it is made.
(6) A determination under paragraph (1)(b) is a disallowable instrument for the purposes of section 46A of the Acts Interpretation Act 1901.
23 Process for determining unfunded IBNR factor under section 22
Report by the Actuary
(1) The Actuary must give the Minister a written report in relation to each participating MDO that:
(a) states the factor that the Actuary considers should be set as the unfunded IBNR factor for the participating MDO; and
(b) sets out the reasons for the statement.
(2) In preparing the report, the Actuary must take into account any information that the HIC gives the Actuary in relation to the MDO under subsection (6).
HIC’s information gathering powers
(3) If the HIC believes on reasonable grounds that a participating MDO is capable of giving information that is relevant to determining the MDO’s unfunded IBNR factor, the HIC may request the MDO to give the HIC the information.
Note: Failure to comply with the request is an offence (see section 45).
(4) The request:
(a) must be made in writing; and
(b) must state what information the MDO must give to the HIC; and
(c) may require the information to be verified by statutory declaration; and
(d) must specify the day on or before which the information must be given; and
(e) must contain a statement to the effect that a failure to comply with the request is an offence.
The day specified under paragraph (d) must be at least 28 days after the day on which the request is made.
(5) Without limiting subsection (3), the kind of information that may be requested includes information in the form of financial statements.
(6) The HIC must give any information that the MDO gives the HIC to the Actuary for the purposes of preparing the report for the Minister under subsection (1).
Subdivision E—Recovery of amount paid to MDO or insurer after IBNR indemnity paid
24 Recovery if certain amounts paid to MDO or insurer after IBNR indemnity paid
(1) An MDO or insurer must repay an amount to the Commonwealth if:
(a) an IBNR indemnity has been paid to the MDO or insurer in relation to a claim against or by a person in relation to an incident; and
(b) an amount is paid to the MDO or insurer in relation to the payment the MDO or insurer made in relation to the incident; and
(c) that amount was not taken into account in calculating the amount of the IBNR indemnity paid to the MDO or insurer; and
(d) the amount is not an amount referred to in subsection 21(4); and
(e) the HIC gives the MDO or insurer a notice in relation to the amount under section 26.
(2) The amount to be repaid is the amount obtained by applying the relevant participating MDO’s unfunded IBNR factor to the amount referred to in paragraph (1)(b).
(3) For the purposes of subsection (2), the relevant participating MDO is the MDO referred to in paragraph 16(1)(c) or 17(1)(c) as that paragraph applies for the purposes of determining whether the IBNR indemnity was payable to the MDO or insurer.
(4) The amount to be repaid is a debt due to the Commonwealth.
(5) The amount to be repaid may be recovered:
(a) by action by the HIC against the MDO or insurer in a court of competent jurisdiction; or
(b) by deduction from the amount of an indemnity scheme payment payable to the MDO or insurer; or
(c) under section 42.
The total amount recovered must not exceed the amount to be repaid.
25 MDO or insurer to inform HIC of certain amounts
(1) If:
(a) an IBNR indemnity is paid to an MDO or insurer in relation to a claim against or by a person in relation to an incident; and
(b) an amount to which section 24 applies is paid to the MDO or insurer;
the MDO or insurer must notify the HIC that the amount has been paid to the MDO or insurer.
Note: Failure to notify is an offence (see section 46).
(2) The notification must:
(a) be in writing; and
(b) be given to the HIC within 28 days after the day on which the amount is paid to the MDO or insurer.
26 HIC to notify MDO or insurer of repayable amount
(1) If an amount to which section 24 applies is paid to an MDO or insurer, the HIC may give the MDO or insurer a written notice that specifies:
(a) the amount that is repayable to the Commonwealth; and
(b) the day before which the amount must be repaid to the Commonwealth; and
(c) the effect of section 27.
The day specified under paragraph (b) must be at least 28 days after the day on which the notice is given.
(2) The amount becomes due and payable on the day specified under paragraph (1)(b).
27 Penalty imposed if an amount is repaid late
(1) If:
(a) an MDO or insurer must repay an amount to the Commonwealth under section 24; and
(b) the amount remains wholly or partly unpaid after it becomes due and payable;
the MDO or insurer is liable to pay a late payment penalty under this section.
(2) The late payment penalty is calculated:
(a) at the prescribed rate; and
(b) on the unpaid amount; and
(c) for the period:
(i) starting when the amount becomes due and payable; and
(ii) ending when the amount, and the penalty payable under this section in relation to the amount, have been paid in full.
(3) The HIC may remit the whole or a part of an amount of late payment penalty if the HIC considers that there are good reasons for doing so.
(4) An application may be made to the Administrative Appeals Tribunal for review of a decision of the HIC not to remit, or to remit only part of, an amount of late payment penalty.
Note: Section 27A of the Administrative Appeals Tribunal Act 1975 requires notification of a decision that is reviewable.
Division 2—High cost claim indemnity scheme
28 Guide to the high cost claim indemnity provisions
(1) This Division provides that a high cost claim indemnity may be paid to an MDO or insurer that pays, or is liable to pay, more than a particular amount (referred to as the high cost claim threshold) in relation to a claim against a person in relation to an incident that occurs in the course of, or in connection with, the practice by the person of a medical profession.
(2) The following table tells you where to find the provisions dealing with various issues:
Where to find the provisions on various issues | ||
Item | Issue | Provisions |
1 | what is the high cost claim threshold? | section 29 |
2 | what conditions must be satisfied for an MDO or insurer to get the high cost claim indemnity? | sections 30 to 32 |
3 | what happens if the incidents occurred during the treatment of a public patient in a public hospital? | paragraph 32(a) and section 33 |
4 | how much is the high cost claim indemnity? | section 34 |
5 | how do MDOs and insurers apply for the high cost claim indemnity? | section 36 |
6 | when will the high cost claim indemnity be paid? | section 37 |
7 | what information has to be provided to the HIC about high cost indemnity matters? | section 38 |
8 | what records must MDOs and insurers keep? | sections 39 and 40 |
9 | how are overpayments of high cost claim indemnity recovered? | sections 41 and 42 |
(1) The high cost claim threshold is:
(a) $2 million; or
(b) such other amount as is prescribed by the regulations.
(2) Regulations that specify an amount of more than $2 million for the purposes of paragraph (1)(b) must not take effect earlier than 12 months after the day on which the regulations are notified in the Gazette.
Subdivision B—High cost claim indemnity
30 Circumstances in which high cost claim indemnity payable
Basic payability rule
(1) Subject to section 31, a high cost claim indemnity is payable to an MDO or insurer under this section if:
(a) a claim for compensation or damages is, or was, made by a person against another person (the practitioner); and
(b) the claim relates to:
(i) an incident that occurs or occurred; or
(ii) a series of related incidents that occur or occurred;
in the course of, or in connection with, the practice by the practitioner of a medical profession; and
(c) either:
(i) the incident occurs or occurred; or
(ii) one or more of the incidents in the series occurs or occurred;
in Australia or in an external Territory; and
(d) the MDO or insurer becomes aware of the claim against the practitioner:
(i) on or after 1 January 2003; and
(ii) on or before the date prescribed by the regulations as the termination date for the high cost claim indemnity scheme; and
(e) the MDO or insurer has a qualifying payment, or qualifying payments, in relation to the claim (see subsection (2)); and
(f) the amount of the qualifying payment, or the sum of the amounts of the qualifying payments, exceeds the high cost claim threshold.
The claim referred to in paragraph (a) may be one that was made before, or is made after, the commencement of this Act and an incident referred to in paragraph (b) may be one that occurred before, or occurs after, the commencement of this Act.
Qualifying payments
(2) The MDO or insurer has a qualifying payment in relation to the claim if:
(a) the MDO or insurer:
(i) pays an amount in relation to the claim; or
(ii) is liable to pay an amount in relation to a payment or payments that someone makes, or is liable to make, in relation to the claim under a written agreement between the parties to the claim; or
(iii) is liable to pay an amount in relation to a payment or payments that someone makes, or is liable to make, in relation to the claim under a judgment or order of a court that is not stayed and is not subject to appeal; or
(iv) is an externally‑administered body corporate and is liable to pay a provable amount in relation to the claim; and
(b) the MDO or insurer pays, or is liable to pay, the amount under an insurance contract or other indemnity arrangement between the MDO or insurer and the practitioner; and
(c) the MDO or insurer:
(i) pays, or becomes liable to pay, the amount in the ordinary course of the MDO’s or the insurer’s business; or
(ii) is an externally‑administered body corporate and would be able to pay the amount in the ordinary course of the MDO’s or the insurer’s business if it were not an externally‑administered body corporate.
Note: Subparagraph (a)(iii)—subsection (4) explains when a judgment or order is treated as still being subject to appeal.
(3) The date prescribed by the regulations for the purposes of subparagraph (1)(d)(ii) must be at least 12 months after the day on which the regulations are notified in the Gazette.
(4) For the purposes of subparagraph (2)(a)(iii), a judgment or order is subject to appeal until:
(a) any applicable time limits for lodging an appeal (however described) against the judgment or order have expired; and
(b) if there is such an appeal against the judgment or order—the appeal (and any subsequent appeals) have been finally disposed of.
Indemnity to be paid on trust if MDO or insurer under external administration
(5) If a high cost claim indemnity is paid to an MDO or insurer that is an externally‑administered body corporate, the indemnity is, to the extent to which it is attributable to an amount that the MDO or insurer is liable to pay to a person, paid on trust for the benefit of that person.
31 Aggregating amounts paid or payable by an MDO and insurer
(1) This section applies if:
(a) an MDO pays, or is liable to pay, an amount in relation to a claim; and
(b) an insurer also pays, or is also liable to pay, an amount in relation to the same claim (the insurer amount); and
(c) but for this section, a high cost claim indemnity in respect of the insurer amount:
(i) would be payable to the insurer under subsection 30(1); or
(ii) would be payable to the insurer under that subsection if paragraph 30(1)(f) were omitted; and
(d) the insurer elects in writing to have this section apply to the insurer amount.
(2) For the purposes of this Division (other than this section):
(a) the MDO is taken:
(i) to have paid, or to be liable to pay, the insurer amount in relation to the claim; and
(ii) to satisfy paragraphs 30(1)(a) to (e) and (2)(a) to (c) in relation to the insurer amount; and
(b) a high cost claim indemnity is not payable to the insurer in respect of the insurer amount.
A high cost claim indemnity is not payable to an MDO or insurer under section 30 in relation to a payment the MDO or insurer makes, or is liable to make, in relation to a claim against a person if:
(a) the incident, or all the incidents, to which the claim relates occurred in the course of the provision of treatment to a public patient in a public hospital; or
(b) the claim is a prescribed claim; or
(c) the claim relates to a prescribed incident.
33 Payment partly related to treatment of public patient in public hospital
(1) This section applies if:
(a) an MDO or insurer makes, or is liable to make, a payment in relation to a claim against a person in relation to a series of related incidents; and
(b) some, but not all, of the incidents occurred in the course of the provision of treatment to a public patient in a public hospital.
(2) For the purposes of this Subdivision, the payment is to be disregarded to the extent to which it relates to, or is reasonably attributable to, the incident or incidents that occurred in the course of the provision of treatment to a public patient in a public hospital.
34 Amount of high cost claim indemnity
(1) The amount of a high cost claim indemnity is:
(a) 50%; or
(b) such other percentage as is prescribed by the regulations;
of the amount by which the amount of the MDO’s or insurer’s qualifying payment, or the sum of the amounts of the MDO’s or insurer’s qualifying payments, exceeds the high cost claim threshold.
(2) Regulations that specify a percentage of less than 50% for the purposes of paragraph (1)(b) must not take effect earlier than 12 months after the day on which the regulations are notified in the Gazette.
Division 3—Administration of the indemnity schemes
(1) This Division makes provision for the administration of the IBNR indemnity scheme and high cost claim indemnity scheme.
(2) The following table tells you where to find the provisions dealing with various issues:
Where to find the provisions on various issues | ||
Item | Issue | Provisions |
1 | how do MDOs and insurers apply for the indemnities? | section 36 |
2 | when will the indemnities be paid? | section 37 |
3 | what information has to be provided to the HIC about indemnity matters? | section 38 |
4 | what records must MDOs and insurers keep? | sections 39 and 40 |
5 | how are overpayments of the indemnities, and indemnity repayments, recovered? | sections 41 and 42 |
Subdivision B—Applications for, and payment of, indemnity scheme payments
36 Application for indemnity scheme payment
(1) An application by an MDO or insurer for an indemnity scheme payment must:
(a) be made in writing using a form approved by the HIC; and
(b) be accompanied by the documents and other information required by the form approved by the HIC.
(2) An application by an MDO or insurer for an IBNR indemnity must be made after the unfunded IBNR factor for the relevant participating MDO has been determined by the Minister under paragraph 22(1)(b).
(3) In subsection (2):
relevant participating MDO means the MDO referred to in paragraph 16(1)(c) or 17(1)(c).
37 Payment date for indemnity scheme payment
(1) Subject to subsection (2), the HIC must pay an indemnity scheme payment that is payable to an MDO or insurer before the end of the month that immediately follows the month in which the MDO or insurer applies for the payment.
(2) If:
(a) an MDO or insurer applies for an indemnity scheme payment; and
(b) the HIC requests a person to give information under section 38 in relation to the application; and
(c) the person does not give the HIC the information requested before the end of the month that immediately follows the month in which the MDO or insurer applies for the payment; and
(d) an indemnity scheme payment is payable to the MDO or insurer;
the HIC must pay the indemnity scheme payment to the MDO or insurer before the end of the month that immediately follows the month in which the person gives the HIC the requested information.
(3) In this section:
month means one of the 12 months of the year.
Subdivision C—Information gathering and record keeping
38 HIC may request information
(1) If the HIC believes on reasonable grounds that a person is capable of giving information that is relevant to determining:
(a) whether an indemnity scheme payment is payable to an MDO or insurer; or
(b) the amount of the indemnity scheme payment that is payable to an MDO or insurer;
the HIC may request the person to give the HIC the information.
Note: Failure to comply with the request is an offence (see section 45).
(2) Without limiting subsection (1), any of the following persons may be requested to give information under that subsection:
(a) an MDO;
(b) an insurer;
(c) a member, or former member, of an MDO;
(d) the legal personal representative of a person mentioned in paragraph (c).
(3) Without limiting subsection (1), the HIC may request an MDO or insurer to give the information by giving the HIC a record, or a copy of a record, kept under section 39 or 40.
(4) The request:
(a) must be made in writing; and
(b) must state what information must be given to the HIC; and
(c) may require the information to be verified by statutory declaration; and
(d) must specify the day on or before which the information must be given; and
(e) must contain a statement to the effect that a failure to comply with the request is an offence.
The day specified under paragraph (d) must be at least 28 days after the day on which the request is made.
39 MDOs and insurers to keep relevant records
Records to be kept by MDO or insurer
(1) An MDO or insurer that applies for an indemnity scheme payment must keep records that are relevant to the following matters:
(a) the payability of the indemnity scheme payment to the MDO or insurer;
(b) the amount of the indemnity scheme payment payable to the MDO or insurer;
(c) any amount paid to the MDO or insurer that results in the MDO or insurer being liable to repay an amount under section 24;
(d) any other matter determined by the HIC.
Note: Failure to keep the records is an offence (see section 47).
Records to be retained for certain period
(2) The records must be retained for a period of 5 years (or any other period prescribed by the regulations) starting on the later of:
(a) the day on which the records were created; or
(b) the day on which this Act commences.
Note: Failure to retain the records is an offence (see section 47).
Determination of additional matters to be gazetted
(3) A determination by the HIC under paragraph (1)(d) must:
(a) be published in the Gazette; and
(b) not take effect earlier than 14 days after the day on which it is published in the Gazette.
Retrospective effect not intended
(4) Nothing in this section is to be taken to have required a person to do an act or thing before the commencement of this Act.
40 Participating MDOs to keep additional records
Records to be kept by participating MDO
(1) A participating MDO must keep records that are relevant to the following matters:
(a) determining who the participating members of the MDO are;
(b) determining its IBNR exposure as at 30 June 2002;
(c) determining its unfunded IBNR factor;
(d) determining its IBNR exposure as at the end of a financial year ending immediately before the start of a contribution year for the MDO;
(e) any other matter determined by the HIC.
Note: Failure to keep the records is an offence (see section 47).
Records to be retained for certain period
(2) The records must be retained for a period of 5 years (or any other period prescribed by the regulations) starting on the later of:
(a) the day on which the records were created; or
(b) the day on which this Act commences.
Note: Failure to retain the records is an offence (see section 47).
Determination of additional matters to be gazetted
(3) A determination by the HIC under paragraph (1)(d) must:
(a) be published in the Gazette; and
(b) not take effect earlier than 14 days after the day on which it is published in the Gazette.
Retrospective effect not intended
(4) Nothing in this section is to be taken to have required a person to do an act or thing before the commencement of this Act.
Subdivision D—Overpayments of the indemnities
(1) This section applies if an amount is paid to an MDO or insurer by way of an indemnity scheme payment and:
(a) the amount of indemnity scheme payment is not payable to the MDO or insurer; or
(b) the amount paid is greater than the amount of the indemnity scheme payment that was payable to the MDO or insurer.
(2) The amount overpaid is:
(a) the whole of the amount paid if paragraph (1)(a) applies; or
(b) the difference between the amount that was paid and the amount that was payable if paragraph (1)(b) applies.
(3) The amount overpaid is a debt due to the Commonwealth.
(4) The amount overpaid may be recovered:
(a) by action by the HIC against the MDO or insurer in a court of competent jurisdiction; or
(b) by deduction from the amount of an indemnity scheme payment payable to the MDO or insurer; or
(c) under section 42.
The total amount recovered must not exceed the amount overpaid.
Subdivision E—Recovery of repayment or overpayment debt
42 HIC may collect money from a person who owes money to a person
What this section does
(1) This section allows the HIC to collect money from a person who owes money to an MDO or insurer that has a debt to the Commonwealth under subsection 24(4) or 41(3) (the repayment or overpayment debt).
The HIC may give direction
(2) The HIC may direct a person (the third party) who owes, or may later owe, money (the available money) to the MDO or insurer to pay some or all of the available money to the HIC in accordance with the direction. The HIC must give a copy of the direction to the MDO or insurer.
Limit on directions
(3) The direction must:
(a) not require an amount to be paid to the HIC at a time before it becomes owing by the third party to the MDO or insurer; and
(b) specify a period of not less than 14 days within which the third party must comply with the direction.
Third party to comply
(4) The third party commits an offence if the third party fails to comply with the direction.
Penalty: 20 penalty units.
(5) The third party does not commit an offence against subsection (4) if the third party complies with the direction so far as the third party is able to do so.
Note: A defendant bears an evidential burden in relation to the matter in this subsection (see subsection 13.3(3) of the Criminal Code).
(6) An offence against subsection (4) is an offence of strict liability.
Note: For strict liability, see section 6.1 of the Criminal Code.
Court orders
(7) If a person is convicted of an offence in relation to a failure of the third party to comply with subsection (4), the court may (in addition to imposing a penalty on the convicted person) order the convicted person to pay to the Commonwealth an amount up to the amount involved in the failure of the third party.
Indemnity
(8) Any payment made by the third party under this section is taken to have been made with the authority of the MDO or insurer and of all other persons concerned and the third party is indemnified for the payment.
Notice
(9) If the whole of the repayment or overpayment debt of the MDO or insurer is discharged before any payment is made by the third party, the HIC must immediately give notice to the third party of that fact.
(10) If a part of the repayment or overpayment debt of the MDO or insurer is discharged before any payment is made by the third party, the HIC must:
(a) immediately give notice to the third party of that fact; and
(b) make an appropriate variation to the direction; and
(c) give a copy of the varied direction to the MDO or insurer.
When third party is taken to owe money
(11) The third party is taken to owe money to the MDO or insurer if:
(a) money is due or accruing by the third party to the MDO or insurer; or
(b) the third party holds money for or on account of the MDO or insurer; or
(c) the third party holds money on account of some other person for payment to the MDO or insurer; or
(d) the third party has authority from some other person to pay money to the MDO or insurer;
whether or not the payment of the money to the MDO or insurer is dependent on a pre‑condition that has not been fulfilled.
Division 4—Medical indemnity premium subsidy scheme
43 Minister may formulate subsidy scheme
(1) The Minister may, by writing, formulate a scheme for making payments to medical practitioners to help those medical practitioners meet the cost of purchasing medical indemnity (whether such costs are incurred by way of MDO membership subscriptions, insurance premiums or otherwise).
(2) Without limiting subsection (1), the scheme may make provision for:
(a) the conditions that must be satisfied for a subsidy to be payable; and
(b) the amount of a subsidy; and
(c) the conditions that must be complied with by medical practitioners to whom a subsidy is paid.
(3) Without limiting paragraph (2)(a), the scheme may provide that a subsidy is to be paid only:
(a) to medical practitioners working in particular areas of medical practice; or
(b) for the purchase of particular kinds of medical indemnity.
(4) A scheme formulated under subsection (1) is a disallowable instrument for the purposes of section 46A of the Acts Interpretation Act 1901.
44 HIC may request information
(1) If the HIC believes on reasonable grounds that a person is capable of giving information that is relevant to determining:
(a) whether a subsidy is payable to a person under a scheme formulated under subsection 43(1); or
(b) the amount of a subsidy that is payable to a person under a scheme formulated under subsection 43(1);
the HIC may request the person to give the HIC the information.
Note: Failure to comply with the request is an offence (see section 45).
(2) The request:
(a) must be made in writing; and
(b) must state what information must be given to the HIC; and
(c) may require the information to be verified by statutory declaration; and
(d) must specify a day on or before which the information must be given; and
(e) must contain a statement to the effect that a failure to comply with the request is an offence.
The day specified under paragraph (d) must be at least 28 days after the day on which the request is made.
45 Failing to give information
(1) This section applies if a person is given a request for information under:
(a) subsection 13(3); or
(b) subsection 23(3); or
(c) subsection 38(1); or
(d) subsection 44(1).
(2) The person commits an offence if the person fails to comply with the request.
Penalty: 30 penalty units.
(3) An individual is excused from complying with the request if the giving of the information might tend to incriminate the individual or expose the individual to a penalty.
(4) An offence against subsection (2) is an offence of strict liability.
Note: For strict liability, see section 6.1 of the Criminal Code.
(1) This section applies if section 25 requires a person to notify the HIC of a matter within a particular period.
(2) The person commits an offence if the person fails to notify the HIC of the matter within that period.
Penalty: 30 penalty units.
(3) An offence against subsection (2) is an offence of strict liability.
Note: For strict liability, see section 6.1 of the Criminal Code.
47 Failing to keep and retain records
(1) This section applies if section 39 or 40 requires a person to keep records or to retain records for a particular period.
(2) The person commits an offence if the person fails to keep the records or fails to retain the records for that period.
Penalty: 30 penalty units.
(3) An offence against subsection (2) is an offence of strict liability.
Note: For strict liability, see section 6.1 of the Criminal Code.
The Consolidated Revenue Fund is appropriated for the purposes of paying:
(a) IBNR indemnities; and
(b) high cost claim indemnities; and
(c) subsidies payable under the scheme formulated under subsection 43(1).
Division 7—Reinsurance contracts
49 Indemnity scheme payments disregarded for purposes of reinsurance contracts
(1) If:
(a) a contract is a contract of insurance:
(i) between 2 insurers; or
(ii) between an insurer and an MDO that are not related bodies corporate; and
(b) the contract is governed by the laws of a State or Territory;
the contract has effect as if the contract provided, and had at all times provided, that:
(c) indemnity scheme payments; and
(d) MDOs’ and insurers’ rights to indemnity scheme payments;
were to be disregarded for all purposes and, without limiting this, were to have no effect on the amounts payable under the contract by the insurer providing the insurance.
(2) By force of this subsection, subsection (1) applies to a contract if it is entered into on or after the commencement of this Act.
(3) By force of this subsection, subsection (1) applies to a contract if it was entered into before the commencement of this Act.
Part 3—Contributions towards the cost of providing indemnities
Division 1—IBNR (incurred but not reported) indemnity contribution
50 Guide to the IBNR indemnity contribution provisions
(1) Division 1 of Part 2 provides for the payment of IBNR indemnities.
(2) The Medical Indemnity (IBNR Indemnity) Contribution Act 2002 (the Contribution Act):
(a) imposes contributions on a participating member of a participating MDO; and
(b) imposes those contributions on the imposition days for the contribution years for the MDO; and
(c) specifies the amount of those contributions (by reference to the participating member’s annual subscription for the MDO for the base year).
This Division contains further provisions relating to the contribution.
(3) The following table tells you where to find the provisions dealing with various issues:
Where to find the provisions on various issues | ||
Item | Issue | Provisions |
1 | which years are contribution years for the participating MDO? | section 5 of the Contribution Act |
2 | which day is the imposition day for a contribution year? | section 5 of the Contribution Act |
3 | who must pay the IBNR indemnity contribution? | section 51 of this Act |
4 | who is exempt from the IBNR indemnity contribution? | sections 52 and 53 of this Act |
5 | what is the amount of the IBNR indemnity contribution? | section 6 of the Contribution Act |
6 | how do you work out a person’s annual subscription for the base year? | section 54 of this Act |
7 | what is the time for paying the IBNR indemnity contribution? | sections 61 to 63 of this Act |
8 | when can the IBNR indemnity contributions for the remaining contribution years be paid by lump sum in advance? | section 64 of this Act |
9 | when is late payment penalty payable? | section 65 of this Act |
10 | what method should be used to pay the IBNR indemnity contribution? | section 66 of this Act |
11 | what happens if an amount of IBNR indemnity contribution is overpaid? | section 67 of this Act |
12 | how are IBNR indemnity contributions and late payment penalties recovered? | sections 68 to 70 of this Act |
13 | what information has to be provided to the HIC about IBNR indemnity contribution matters? | sections 71 and 72 of this Act |
Subdivision B—Who pays IBNR indemnity contribution
51 Who is liable to pay the IBNR indemnity contribution
A person is liable to pay an IBNR indemnity contribution for a financial year if:
(a) the person is a participating member of a participating MDO; and
(b) the financial year is a contribution year for the MDO; and
(c) the person was ordinarily resident in Australia or an external Territory on 30 June 2000; and
(d) the person is not exempt from the contribution under section 52.
(1) A person may be exempt from an IBNR indemnity contribution under subsection (2) or under regulations made for the purposes of subsection (4).
(2) A person is exempt from an IBNR indemnity contribution for a contribution year for a participating MDO if:
(a) the person dies before the imposition day in that contribution year; or
(b) the person has not practised a medical profession in Australia for reward at any time after 31 December 2001; or
(c) if the person’s medical income for both:
(i) the financial year starting on 1 July 2001; and
(ii) the financial year immediately before the contribution year;
was less than $5,000; or
(d) the person was not on, or at any time before, 30 June 2000:
(i) a medical practitioner; or
(ii) a health professional;
and is not a person specified in the regulations made for the purposes of this paragraph; or
(e) before the day on which the contribution would otherwise become due and payable, the person paid a lump sum under section 64 in relation to the IBNR indemnity contributions payable by the person; or
(f) the HIC determines under section 53 that the person has comprehensive insurance cover for all incidents covered by the IBNR indemnity scheme.
(3) For the purposes of paragraph (2)(c), a person’s medical income is:
(a) if the person is a medical practitioner—the sum of the medicare benefits payable in respect of professional services rendered by, or on behalf of, the person; and
(b) if the person is a health professional—the sum of the amounts payable in respect of health care related services rendered by, or on behalf of, the person.
(4) The regulations may provide that a person is exempt from IBNR indemnity contribution in the circumstances specified in the regulations.
(5) Regulations made for the purposes of subsection (4) may provide that a person is exempt from IBNR indemnity contribution either generally or for a particular contribution year of a participating MDO.
53 Comprehensive insurance cover determination
(1) The HIC may determine, in writing, that a person who is a participating member of a participating MDO has comprehensive insurance cover for all incidents covered by the IBNR indemnity scheme.
(2) The HIC may make the determination only if satisfied that:
(a) on 30 June 2002, the person had:
(i) an insurance contract or contracts with an insurer; or
(ii) insurance contracts with 2 or more insurers; and
(b) the contract or contracts indemnified the person in relation to claims against or by the person in relation to all the incidents that:
(i) occurred in the course of, or in connection with, the practice of a medical profession by the person; and
(ii) are covered by the IBNR indemnity scheme; and
(c) the insurer or each of the insurers:
(i) is either authorised to carry on insurance business in Australia under the Insurance Act 1973 or is approved by the HIC for the purposes of this subparagraph; and
(ii) is not a related body corporate of the participating MDO; and
(d) the insurer or all the insurers have remained and will continue to remain liable to indemnify the person for claims against and by the person in relation to all those incidents (without any further premium payments by the person at any time after 30 June 2002).
Subdivision C—Determining amount of IBNR indemnity contribution
54 Annual subscription for base year
Background
(1) Under section 6 of the Medical Indemnity (IBNR Indemnity) Contribution Act 2002, the amount of the IBNR indemnity contribution imposed on a participating member of a participating MDO depends on the amount of the member’s annual subscription for the base year.
Membership subscription
(2) The member’s annual subscription for the base year does not include:
(a) a fee paid, or a fee to the extent to which it is paid, by the member:
(i) to join the MDO initially; or
(ii) to re‑join the MDO after having ceased to be a member of the MDO; or
(b) an amount paid by the member in response to a call made by the MDO; or
(c) any other prescribed amount.
Base year
(3) The base year for the member is:
(a) if an amount was payable by the member for membership of the participating MDO for a full year that commenced during the financial year that started on 1 July 2000—that full year; or
(b) if no amount was payable by the member for membership of the participating MDO for a full year that commenced during that financial year—the most recent preceding full year for which an amount was payable by the member for membership of the MDO; or
(c) if neither paragraph (a) nor paragraph (b) applies—the most recent period that started before 1 July 2000 and for which an amount was payable by the member for membership of the MDO.
Subdivision D—Annual reassessment of participating MDO’s IBNR exposure
The object of this Subdivision is to allow the Minister to reassess a participating MDO’s IBNR exposure annually so that:
(a) the amount of the IBNR indemnity contributions imposed on its participating members; or
(b) the years that are contribution years for the MDO;
can be adjusted (if necessary) to appropriately reflect the extent of the Commonwealth’s liability for IBNR indemnities in relation to the members and former members of the MDO.
56 Process for annually reassessing IBNR exposure
Report by the Actuary
(1) For each contribution year for a participating MDO, the Actuary must give the Minister a written report that:
(a) states the Actuary’s assessment of the MDO’s IBNR exposure as at the end of the financial year that ends immediately before the start of that contribution year; and
(b) sets out the reasons for the assessment.
(2) In preparing the report, the Actuary must take into account any information that the HIC gives the Actuary in relation to the MDO under subsection (6).
HIC’s information gathering powers
(3) If the HIC believes on reasonable grounds that a participating MDO is capable of giving information that is relevant to assessing the MDO’s IBNR exposure as at the end of a financial year that ends immediately before the start of a contribution year for the MDO, the HIC may request the MDO to give the HIC the information.
Note: Failure to comply with the request is an offence (see section 73).
(4) Without limiting subsection (3), the kind of information that may be requested includes information in the form of:
(a) financial statements; and
(b) a report prepared by a suitably qualified actuary assessing the MDO’s IBNR exposure as at the end of a financial year that ends immediately before the start of a contribution year for the MDO.
(5) The request:
(a) must be made in writing; and
(b) must state what information the MDO is to give to the HIC; and
(c) may require the information to be verified by statutory declaration; and
(d) must specify the day on or before which the information must be given; and
(e) must contain a statement to the effect that a failure to comply with the request is an offence.
The day specified under paragraph (d) must be at least 28 days after the day on which the request is made.
(6) The HIC must give any information that the MDO gives the HIC to the Actuary for the purposes of preparing the report for the Minister under subsection (1).
Division 2—Enhanced UMP indemnity contribution
57 Guide to the enhanced UMP indemnity contribution provisions
(1) The Commonwealth provides assistance in relation to claims by members and former members of UMP under a Medical Indemnity Agreement.
Note: See the Medical Indemnity Agreement (Financial Assistance—Binding Commonwealth Obligations) Act 2002.
(2) The Medical Indemnity (Enhanced UMP Indemnity) Contribution Act 2002 (the Contribution Act):
(a) imposes contributions on a person who was a member of UMP on 1 July 2002; and
(b) imposes those contributions on the imposition days for the contribution years; and
(c) specifies the amount of those contributions.
This Division contains further provisions relating to the contribution.
(3) The following table tells you where to find the provisions dealing with various issues:
Where to find the provisions on various issues | ||
Item | Issue | Provisions |
1 | which years are contribution years? | section 5 of the Contribution Act |
2 | which day is the imposition day for a contribution year? | section 5 of the Contribution Act |
3 | who must pay the enhanced UMP indemnity contribution? | section 58 of this Act |
4 | who is exempt from the enhanced UMP indemnity contribution? | section 59 of this Act |
5 | what is the amount of the enhanced UMP indemnity contribution? | section 6 of the Contribution Act |
6 | what is the time for paying the enhanced UMP indemnity contribution? | sections 61 to 63 of this Act |
7 | when can the enhanced UMP indemnity contributions for the remaining contribution years be paid by lump sum in advance? | section 64 of this Act |
8 | when is late payment penalty payable? | section 65 of this Act |
9 | what method should be used to pay the enhanced UMP indemnity contribution? | section 66 of this Act |
10 | what happens if an amount of UMP indemnity contribution is overpaid? | section 67 of this Act |
11 | how are enhanced UMP indemnity contributions and late payment penalties recovered ? | sections 68 to 70 of this Act |
12 | what information has to be provided to the HIC about enhanced UMP indemnity contribution matters? | sections 71 and 72 of this Act |
Subdivision B—Who pays enhanced UMP indemnity contribution
58 Who is liable to pay the enhanced UMP indemnity contribution
A person is liable to pay an enhanced UMP indemnity contribution for a financial year if:
(a) the person was a member of UMP on 1 July 2002; and
(b) the financial year is a contribution year; and
(c) the person was ordinarily resident in Australia or an external Territory on 1 July 2002; and
(d) the person is not exempt from the contribution under section 59.
(1) A person may be exempt from an enhanced UMP indemnity contribution under subsection (2) or under regulations made for the purposes of subsection (3).
(2) A person is exempt from an enhanced UMP indemnity contribution for a contribution year if:
(a) the person dies before the imposition day in that contribution year; or
(b) before the day on which the contribution would otherwise become due and payable, the person paid a lump sum under section 64 in relation to the enhanced UMP indemnity contributions payable by the person.
(3) The regulations may provide that a person is exempt from enhanced UMP indemnity contribution in the circumstances specified in the regulations.
(4) Regulations made for the purposes of subsection (3) may provide that a person is exempt from enhanced UMP indemnity contribution either generally or for a particular contribution year.
Division 3—Administration of the medical indemnity contributions
(1) This Division makes provision for the administration of the IBNR indemnity contributions and enhanced UMP indemnity contributions.
(2) The following table tells you where to find the provisions dealing with various issues:
Where to find the provisions on various issues | ||
Item | Issue | Provisions |
1 | what is the time for paying the contributions? | sections 61 to 63 |
2 | when can the contributions for the remaining contribution years be paid by lump sum in advance? | section 64 |
3 | when is late payment penalty payable? | section 65 |
4 | what method should be used to pay the contributions? | section 66 |
5 | what happens if the contributions are overpaid? | section 67 |
6 | how are contributions and late payment penalties recovered? | sections 68 to 70 |
7 | what information has to be provided to the HIC about contribution matters? | sections 71 and 72 |
Subdivision B—Payment and collection of medical indemnity contributions
61 When medical indemnity contribution must be paid
Subject to sections 62, 63 and 64, a medical indemnity contribution for a contribution year becomes due and payable on the payment day for the contribution worked out using the following table:
Payment day for medical indemnity contribution | ||
Item | An indemnity contribution of this kind… | becomes due and payable on… |
1 | IBNR indemnity contribution | (a) 1 November in the contribution year; or (b) such other day in the contribution year as is specified in the regulations as the payment day for the contribution year. |
2 | enhanced UMP indemnity contribution | (a) 1 November for the contribution year; or (b) such other day in the contribution year as is specified in the regulations as the payment day for the contribution year. |
62 Deferral of payment day for medical indemnity contribution
(1) A person who is liable to pay a medical indemnity contribution for a contribution year may apply to the HIC to defer the payment day for the contribution under this section. The person may apply even if the last contribution year for the contribution has not been declared by regulations under the relevant medical indemnity contribution legislation.
(2) The application must be:
(a) in writing; and
(b) made before the contribution becomes due and payable.
(3) The HIC may approve the application if the HIC:
(a) is satisfied that the person meets the conditions specified in the regulations; and
(b) has not approved an application by the person to defer the payment day for that kind of medical indemnity contribution for an earlier contribution year under this section.
(4) If the HIC approves the application, the contribution becomes due and payable on the deferred payment day worked out using the following table:
Deferred payment day for certain contributions | ||
Item | An indemnity contribution of this kind… | becomes due and payable on… |
1 | IBNR indemnity contribution | (a) 1 November in the financial year immediately following the last contribution year; or (b) such other day in the financial year immediately following the last contribution year as is specified in the regulations. |
2 | enhanced UMP indemnity contribution | (a) 1 November in the financial year immediately following the last contribution year; or (b) such other day in the financial year immediately following the last contribution year as is specified in the regulations. |
(5) The HIC must give the person a written notice that:
(a) states whether the application has been approved; and
(b) specifies the deferred payment day worked out under subsection (4); and
(c) states the effect of subsection (7).
(6) An application may be made to the Administrative Appeals Tribunal for review of a decision of the HIC not to approve an application under this section.
Note: Section 27A of the Administrative Appeals Tribunal Act 1975 requires notification of a decision that is reviewable.
(7) If the person dies before the deferred payment day worked out under subsection (4), the contribution becomes due and payable immediately after the person’s death.
63 Medical indemnity contribution may be paid by instalments
(1) If:
(a) a person is liable to pay a medical indemnity contribution for a contribution year; and
(b) the amount of the contribution for that contribution year is $1,000 or more;
the person may apply to the HIC to pay the contribution by instalments.
(2) The application must be:
(a) in writing; and
(b) made before the contribution becomes due and payable.
(3) The HIC must give the person a written notice that:
(a) states whether the application has been approved; and
(b) specifies the period over which the instalments are to be paid; and
(c) specifies for each instalment:
(i) the day within that period on which the instalment becomes due and payable; and
(ii) the amount of the instalment; and
(d) states the effect of subsection (4).
The period specified under paragraph (b) must be one that ends not later than 12 months after the day on which the contribution would become due and payable but for this section.
(4) If:
(a) the HIC approves an application under this section; and
(b) an instalment is not paid on or before the day specified for the instalment under subparagraph (3)(c)(i);
the whole of the unpaid amount of the contribution becomes due and payable on the day after that day.
(5) An application may be made to the Administrative Appeals Tribunal for review of a decision of the HIC to approve or not to approve an application under this section.
Note: Section 27A of the Administrative Appeals Tribunal Act 1975 requires notification of a decision that is reviewable.
64 Discount for lump sum payment of medical indemnity contribution
Election to pay lump sum
(1) A person who is liable to pay a medical indemnity contribution for a contribution year (the current contribution year) may elect to pay the lump sum worked out under subsection (4).
Note: If the person pays the lump sum worked out under subsection (4), the person is exempt from medical indemnity contributions of that kind for any subsequent contribution year.
(2) The election must be:
(a) in writing; and
(b) made before the contribution becomes due and payable.
(3) The HIC must give the person a written notice that specifies:
(a) the lump sum worked out under subsection (4); and
(b) the day on which the lump sum becomes due and payable.
Amount of the lump sum
(4) The lump sum is worked out using the following formula:
![]()
where:
discount factor is the discount factor worked out under subsection (6).
outstanding amount is the amount worked out under subsection (5).
(5) The outstanding amount is worked out using the following formula:
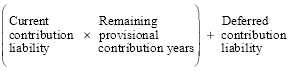
where:
current contribution liability is the amount of the medical indemnity contribution the person is liable to pay for the current contribution year.
deferred contribution liability is the amount (if any) of the contribution of that kind that the person would otherwise be liable to pay on or before the deferred payment day worked out under section 62.
remaining provisional contribution years is the number of provisional contribution years that have not ended.
(6) The discount factor is:
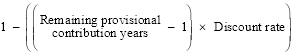
where:
discount rate is:
(a) 0.025; or
(b) such higher or lower number as is specified in the regulations.
remaining provisional contribution years is the number of provisional contribution years that have not ended.
(7) Subject to regulations made for the purposes of subsection (8), the provisional contribution years for a medical indemnity contribution are:
(a) the first financial year that is a contribution year for medical indemnity contributions of that kind; and
(b) the next 9 financial years.
(8) The regulations may specify the financial years that are to be provisional contribution years for a medical indemnity contribution.
(1) If:
(a) a person is liable to pay:
(i) a medical indemnity contribution; or
(ii) a lump sum payable under section 64; and
(b) the contribution or lump sum remains wholly or partly unpaid after it becomes due and payable;
the person is liable to pay a late payment penalty under this section.
(2) The late payment penalty is calculated:
(a) at the prescribed rate; and
(b) on the unpaid amount of contribution or lump sum; and
(c) for the period:
(i) starting when the contribution or lump sum becomes due and payable; and
(ii) ending when the contribution or lump sum, and the penalty payable under this section in relation to the contribution or lump sum, have been paid in full.
Paragraph (c) has effect subject to subsection (3).
(3) The person is not liable to pay a late payment penalty under subsection (1) for any period after the person’s death.
(4) The HIC may remit the whole or a part of an amount of late payment penalty if the HIC considers that there are good reasons for doing so.
(5) An application may be made to the Administrative Appeals Tribunal for review of a decision of the HIC not to remit, or to remit only part of, an amount of late payment penalty.
Note: Section 27A of the Administrative Appeals Tribunal Act 1975 requires notification of a decision that is reviewable.
66 Method of paying certain amounts
(1) A medical indemnity contribution must be paid to the HIC.
(2) A lump sum payable under section 64 must be paid to the HIC.
(3) A late payment penalty payable under section 65 must be paid to the HIC.
(4) The regulations may specify methods for paying an amount referred to in subsection (1), (2) or (3).
Refund of overpaid medical indemnity contribution and late payment penalty
(1) If a person overpays:
(a) a medical indemnity contribution for a contribution year; or
(b) a late payment penalty in relation to a medical indemnity contribution for a contribution year;
the amount overpaid must be refunded to the person unless the person makes an election under subsection (2).
(2) The person may elect in writing to offset the amount overpaid against a medical indemnity contribution the person is liable to pay for a contribution year that immediately follows the contribution year referred to in paragraph (1)(a) or (b).
Refund of overpaid lump sum
(3) If a person overpays a lump sum payable under section 64, the amount overpaid must be refunded to the person.
Appropriation
(4) The Consolidated Revenue Fund is appropriated for the purpose of providing refunds under this section.
Subdivision D—Recovery of contribution debt
68 Recovery of contribution debt
(1) A medical indemnity contribution is a debt due to the Commonwealth.
(2) A lump sum payable under section 64 is a debt due to the Commonwealth.
(3) A late payment penalty payable under section 65 is a debt due to the Commonwealth.
(4) The HIC may recover an amount referred to in subsection (1), (2) or (3) as a debt by action in a court of competent jurisdiction.
69 HIC may collect money from a person who owes money to a person
What this section does
(1) This section allows the HIC to collect money from a person who owes money to a person (the contribution debtor) who has a debt to the Commonwealth under section 68 (a contribution debt).
The HIC may give direction
(2) The HIC may direct a person (the third party) who owes, or may later owe, money (the available money) to the contribution debtor to pay some or all of the available money to the HIC in accordance with the direction. The HIC must give a copy of the direction to the contribution debtor.
Limit on directions
(3) The direction must:
(a) not require an amount to be paid to the HIC at a time before it becomes owing by the third party to the contribution debtor; and
(b) specify a period of not less than 14 days within which the third party must comply with the direction.
Third party to comply
(4) The third party commits an offence if the third party fails to comply with the direction.
Penalty: 20 penalty units.
(5) The third party does not commit an offence against subsection (4) if the third party complies with the direction so far as the third party is able to do so.
Note: A defendant bears an evidential burden in relation to the matter in this subsection (see subsection 13.3(3) of the Criminal Code).
(6) An offence against subsection (4) is an offence of strict liability.
Note: For strict liability, see section 6.1 of the Criminal Code.
Court orders
(7) If a person is convicted of an offence in relation to a failure of the third party to comply with subsection (4), the court may (in addition to imposing a penalty on the convicted person) order the convicted person to pay to the HIC an amount up to the amount involved in the failure of the third party.
Indemnity
(8) Any payment made by the third party under this section is taken to have been made with the authority of the contribution debtor and of all other persons concerned and the third party is indemnified for the payment.
Notice
(9) If the whole of the contribution debt of the contribution debtor is discharged before any payment is made by the third party, the HIC must immediately give notice to the third party of that fact.
(10) If a part of the contribution debt of the contribution debtor is discharged before any payment is made by the third party, the HIC must:
(a) immediately give notice to the third party of that fact; and
(b) make an appropriate variation to the direction; and
(c) give a copy of the varied direction to the contribution debtor.
When third party is taken to owe money
(11) The third party is taken to owe money to the contribution debtor if:
(a) money is due or accruing by the third party to the contribution debtor; or
(b) the third party holds money for or on account of the contribution debtor; or
(c) the third party holds money on account of some other person for payment to the contribution debtor; or
(d) the third party has authority from some other person to pay money to the contribution debtor;
whether or not the payment of the money to the contribution debtor is dependent on a pre‑condition that has not been fulfilled.
(1) The HIC may issue a written certificate:
(a) stating that a person is liable to pay:
(i) a medical indemnity contribution; or
(ii) a lump sum under section 64; or
(iii) a late payment penalty in relation to a medical indemnity contribution; and
(b) setting out particulars of the liability.
(2) In any civil proceedings under, or arising out of, this Act or the medical indemnity contribution legislation, a certificate under subsection (1) is prima facie evidence of the matters in the certificate.
(3) A document purporting to be a certificate under subsection (1) must, unless the contrary is established, be taken to be such a certificate and to have been properly issued.
(4) The HIC may certify that a document is a copy of a certificate issued under subsection (1).
(5) This section applies to the certified copy as if it were the original.
Subdivision E—Information gathering processes
71 HIC may request information
(1) If the HIC believes on reasonable grounds that a person is capable of giving information that is relevant to determining:
(a) whether a person is liable to pay a medical indemnity contribution; or
(b) the amount of the medical indemnity contribution a person is liable to pay;
the HIC may request the person to give the HIC the information.
Note: Failure to comply with the request is an offence (see section 73).
(2) Without limiting subsection (1), any of the following persons may be requested to provide information under that subsection:
(a) an MDO;
(b) an insurer;
(c) a member, or former member, of an MDO;
(d) the legal personal representative of a person mentioned in paragraph (c).
(3) The request:
(a) must be made in writing; and
(b) must state what information must be given to the HIC; and
(c) may require the information to be verified by statutory declaration; and
(d) must specify the day on or before which the information must be given; and
(e) must contain a statement to the effect that a failure to comply with the request is an offence.
The day specified under paragraph (d) must be at least 28 days after the day on which the request is made.
72 HIC must be notified of a change in circumstances etc.
(1) A person who:
(a) is exempt from a medical indemnity contribution because of the existence of particular circumstances; and
(b) ceases to be exempt from the contribution because those circumstances change before the start of, or during, a contribution year;
must notify the HIC of that change in circumstances.
Note: Failure to notify is an offence (see section 74).
(2) The notification must:
(a) be in writing; and
(b) set out details of the change in circumstances; and
(c) be given to the HIC within 28 days after the day on which the person becomes aware of the change in circumstances.
73 Failing to give information
(1) This section applies if a person is given a request for information under:
(a) subsection 56(3); or
(b) subsection 71(1).
(2) The person commits an offence if the person fails to comply with the request.
Penalty: 30 penalty units.
(3) An individual is excused from complying with the request if the giving of the information might tend to incriminate the individual or expose the individual to a penalty.
(4) An offence against subsection (2) is an offence of strict liability.
Note: For strict liability, see section 6.1 of the Criminal Code.
(1) This section applies if section 72 requires a person to notify the HIC, within a particular period, of a change in circumstances.
(2) The person commits an offence if the person fails to notify the HIC of those circumstances within that period.
Penalty: 30 penalty units.
(3) An offence against subsection (2) is an offence of strict liability.
Note: For strict liability, see section 6.1 of the Criminal Code.
75 General administration of this Act and medical indemnity contribution legislation
The HIC has the general administration of this Act and the medical indemnity contribution legislation.
76 Additional functions of the HIC
In addition to the functions of the HIC under the Health Insurance Commission Act 1973, the HIC has such additional functions as are conferred on the HIC under this Act and the medical indemnity contribution legislation.
77 Officers to observe secrecy
(1) In this section:
medical indemnity legislation means:
(a) this Act; or
(b) the medical indemnity contribution legislation.
officer means a person performing duties, or exercising powers or functions, under or in relation to, the medical indemnity legislation.
person to whom this section applies means a person who is or was an officer.
protected document means a document that:
(a) is obtained or made by a person to whom this section applies in the course of, or because of, the person’s functions, powers or duties under or in relation to the medical indemnity legislation; and
(b) contains information relating to a person’s affairs.
protected information means information that:
(a) is disclosed to, or obtained by, a person to whom this section applies in the course of, or because of, the person’s functions, powers or duties under or in relation to the medical indemnity legislation; and
(b) relates to a person’s affairs.
(2) A person to whom this section applies commits an offence if:
(a) the person:
(i) makes a copy or other record of any protected information or of all or part of any protected document; or
(ii) discloses any protected information to another person; or
(iii) produces all or part of a protected document to another person; and
(b) in doing so, is not acting in the performance of his or her duties, or in the exercise of his or her powers or functions, under the medical indemnity legislation; and
(c) in doing so, is not acting for the purpose of enabling a person to perform functions under:
(i) the medical indemnity legislation; or
(ii) the Health Insurance Act 1973; or
(iii) the Health Insurance Commission Act 1973; or
(iv) the National Health Act 1953.
Penalty: Imprisonment for 2 years.
(3) Despite subsection (2), the Secretary or the Managing Director may:
(a) if the Minister certifies, in writing, that it is necessary in the public interest that any protected information should be divulged, divulge that information to such person as the Minister directs; or
(b) divulge any protected information to a person who, in the opinion of the Minister, is expressly or impliedly authorised by the person to whom the information relates to obtain it.
Note: A defendant bears an evidential burden in relation to the matter in this subsection (see subsection 13.3(3) of the Criminal Code).
(4) Despite subsection (2), the Secretary or the Managing Director may divulge any protected information to an authority or person if:
(a) the authority or person is a prescribed authority or person for the purposes of this subsection; and
(b) the information is information of a kind that may, in accordance with the regulations, be provided to the authority or person.
Note: A defendant bears an evidential burden in relation to the matter in this subsection (see subsection 13.3(3) of the Criminal Code).
(5) If protected information is divulged to an authority or person under subsection (3) or (4):
(a) the authority or person; and
(b) any person or employee under the control of the authority or person;
is, in respect of that information, subject to the same rights, privileges, obligations and liabilities under subsection (2) as if he or she were a person performing duties under the medical indemnity legislation and had acquired the information in the performance of those duties.
(6) This section does not prohibit the divulging or communicating to a person of information that relates to the person.
Note: A defendant bears an evidential burden in relation to the matter in this subsection (see subsection 13.3(3) of the Criminal Code).
78 Act not to apply in relation to State insurance within a State
If, but for this section, a provision of this Act:
(a) would have a particular application; and
(b) by virtue of having that application, would be a law with respect to State insurance not extending beyond the limits of the State concerned;
the provision is not to have that application.
(1) The Governor‑General may make regulations prescribing matters:
(a) required or permitted by this Act to be prescribed; or
(b) necessary or convenient to be prescribed for carrying out or giving effect to this Act;
and, in particular, prescribing penalties, not exceeding 10 penalty units, for offences against the regulations.
(2) Without limiting subsection (1), the regulations may make provision for the qualifications of actuaries preparing reports for the purposes of this Act.
(240/02)
[Minister’s second reading speech made in—
House of Representatives on 13 November 2002
Senate on 9 December 2002]