An Act to regulate private health insurance, and for related purposes
Chapter 1—Introduction
Part 1‑1—Introduction
Division 1—Preliminary
1‑1 Short title
This Act may be cited as the Private Health Insurance Act 2007.
1‑5 Commencement
This Act commences on 1 April 2007.
1‑10 Identifying defined terms
(1) Many of the terms in this Act are defined in the Dictionary in Schedule 1.
(2) Most of the terms that are defined in the Dictionary are identified by an asterisk appearing at the start of the term: as in “*health benefits fund”. The footnote with the asterisk contains a signpost to the Dictionary.
(3) An asterisk usually identifies the first occurrence of a term in a section (if not divided into subsections), subsection, definition, table item or diagram. Later occurrences of the term in the same provision are not usually asterisked.
(4) Terms are not asterisked in headings, notes, examples or guides.
(5) If a term is not identified by an asterisk, disregard that fact in deciding whether or not to apply to that term a definition or other interpretation provision.
(6) The following basic terms used throughout the Act are not identified with an asterisk:
Terms that are not identified with an asterisk |
Item | This term ... | is defined in ... |
2 | Federal Court | the Dictionary in Schedule 1 |
3 | insurance | section 5‑1 |
4 | Chief Executive Medicare | the Dictionary in Schedule 1 |
5 | Private Health Insurance Ombudsman | the Dictionary in Schedule 1 |
6 | private health insurer | the Dictionary in Schedule 1 |
1‑15 Extension to Norfolk Island
This Act extends to Norfolk Island.
Division 3—Overview of this Act
3‑1 What this Act is about
This Act is about private health insurance. It:
(a) provides incentives to encourage people to have private health insurance; and
(b) sets out rules governing private health insurance *products.
Note: The Private Health Insurance (Prudential Supervision) Act 2015 sets out the registration process for private health insurers, imposes requirements about how private health insurers conduct health insurance business and deals with other matters in relation to the prudential supervision of private health insurers.
3‑5 Incentives (Chapter 2)
Chapter 2 provides the following incentives:
(a) reductions in premiums for *complying health insurance policies;
(c) a lifetime health cover scheme, under which premiums may rise for people who do not maintain private health insurance from an early age.
3‑10 Complying health insurance products (Chapter 3)
Chapter 3 requires insurers who make private health insurance available to people to do so in a non‑discriminatory way, to offer *products that comply with this Act, and to meet certain other obligations imposed by this Act in relation to those products.
3‑15 Health insurance business, health benefits funds and miscellaneous obligations of private health insurers (Chapter 4)
Chapter 4 defines the key concepts of *health insurance business and *health benefits funds. It also deals with some related matters and imposes miscellaneous obligations on private health insurers.
3‑20 Enforcement (Chapter 5)
Chapter 5 provides for a range of enforcement mechanisms aimed at monitoring and ensuring compliance with this Act and protecting the interests of *policy holders.
3‑25 Administration (Chapter 6)
Chapter 6 contains administrative and machinery provisions relating to the operation of this Act.
3‑30 Dictionary (Schedule 1)
The Dictionary in Schedule 1 contains definitions of terms used throughout this Act.
Division 5—Constitutional matters
5‑1 Meaning of insurance
In this Act:
insurance means insurance to which paragraph 51(xiv) of the Constitution applies.
5‑5 Act not to apply to State insurance within that State
This Act does not apply with respect to State insurance that does not extend beyond the limits of the State concerned.
5‑10 Compensation for acquisition of property
(1) If the operation of this Act would result in an acquisition of property from a person otherwise than on just terms, the Commonwealth is liable to pay a reasonable amount of compensation to the person.
(2) If the Commonwealth and the person do not agree on the amount of the compensation, the person may institute proceedings in the Federal Court for the recovery from the Commonwealth of such reasonable amount of compensation as the court determines.
(3) In this section:
acquisition of property has the same meaning as in paragraph 51(xxxi) of the Constitution.
just terms has the same meaning as in paragraph 51(xxxi) of the Constitution.
Chapter 2—Incentives
Part 2‑1—Introduction
Division 15—Introduction
15‑1 What this Chapter is about
This Chapter contains the following incentives to encourage people to have private health insurance:
(a) reductions in premiums (see Division 23);
(c) lifetime health cover (see Part 2‑3).
Part 2‑2—Premiums reduction scheme
Division 20—Introduction
20‑1 What this Part is about
To encourage people to take out, and continue to hold, private health insurance, this Part provides that people may reduce the premiums payable for their complying health insurance policies by participating in the premiums reduction scheme in Division 23.
Note: The premiums reduction scheme is complemented by the private health insurance offset provided for by Subdivision 61‑G of the Income Tax Assessment Act 1997.
20‑5 Private Health Insurance (Incentives) Rules
Matters relating to the *premiums reduction scheme are also dealt with in the Private Health Insurance (Incentives) Rules. The provisions of this Part indicate when a particular matter is or might be dealt with in these Rules.
Note: The Private Health Insurance (Incentives) Rules are made by the Minister under section 333‑20.
Division 22—PHIIB, PHII benefit and related concepts
Subdivision 22‑A—PHIIB, PHII benefit and related concepts
22‑1 Application of Subdivision
This Subdivision applies if a premium, or an amount in respect of a premium, was paid, or is payable, during a financial year under a *complying health insurance policy in respect of a period (the premium period).
22‑5 Meaning of PHIIB
Adults insured under policy
(1) Each *adult insured under the *complying health insurance policy throughout the premium period is a PHIIB, in respect of the premium or amount.
Note: PHIIB is short for private health insurance incentive beneficiary.
Dependent child‑only policies
(2) Subsections (3) and (4) apply if the only persons insured under the *complying health insurance policy throughout the premium period are one or more *dependent children.
(3) Each person who is a parent (within the meaning of Part 2.11 of the Social Security Act 1991) in relation to one or more of those *dependent children on the last day of the financial year mentioned in section 22‑1 is a PHIIB, in respect of the premium or amount.
(4) However, the person who pays the premium or amount is the only PHIIB, in respect of the premium or amount, if:
(a) disregarding this subsection, more than one person would be a *PHIIB in respect of the premium or amount because of subsection (3); and
(b) those persons are not married to each other (within the meaning of the A New Tax System (Medicare Levy Surcharge—Fringe Benefits) Act 1999) at the end of the financial year; and
(c) the person who pays the premium or amount is not a *dependent child.
22‑10 Meaning of PHII benefit
The amount of the PHII benefit, in respect of the premium or amount, is:
(a) if there is only one *PHIIB in respect of the premium or amount—the PHIIB’s *share of the PHII benefit in respect of the premium or amount; or
(b) if there is more than one PHIIB in respect of the premium or amount—the sum of each of those PHIIB’s share of the PHII benefit in respect of the premium or amount.
Note: PHII benefit is short for private health insurance incentive benefit.
22‑15 Meaning of share of the PHII benefit—single PHIIB
(1) If there is only one *PHIIB in respect of the premium or amount, the amount of the *PHIIB’s share of the PHII benefit, in respect of the premium or amount, is the sum of:
(a) 30% of the amount of the premium, or of the amount in respect of a premium, paid or payable in respect of days in the premium period on which no person insured under the policy was aged 65 years or over; and
(b) 35% of the amount of the premium, or of the amount in respect of a premium, paid or payable in respect of days in the premium period on which:
(i) at least one person insured under the policy was aged 65 years or over; and
(ii) no person insured under the policy was aged 70 years or over; and
(c) 40% of the amount of the premium, or of the amount in respect of a premium, paid or payable in respect of days in the premium period on which at least one person insured under the policy was aged 70 years or over.
Private health insurance tiers
(2) Reduce the amount of each percentage specified in subsection (1) (as affected by subsection (5A)) by 10 percentage points if the *PHIIB is a *tier 1 earner for the financial year mentioned in section 22‑1.
(3) Reduce the amount of each percentage specified in subsection (1) (as affected by subsection (5A)) by 20 percentage points if the *PHIIB is a *tier 2 earner for the financial year mentioned in section 22‑1.
(4) Reduce the amount of each percentage specified in subsection (1) (as affected by subsection (5A)) to nil if the *PHIIB is a *tier 3 earner for the financial year mentioned in section 22‑1.
(5) For the purposes of applying subsections (2), (3) and (4) in relation to the premium or amount, treat the table in subsection 22‑30(1) as applying to the *PHIIB for the financial year if he or she is a PHIIB in respect of the premium or amount because of subsection 22‑5(3) or (4).
Note 1: The table in subsection 22‑30(1) sets out the private health insurance tiers for families.
Note 2: Subsections 22‑5(3) and (4) apply if the only persons insured under the policy are dependent children.
Annual adjustment of percentages
(5A) For each adjustment year, each percentage specified in subsection (1), (2) or (3) is replaced by the percentage worked out as follows:
(a) for the adjustment year starting on 1 April 2014—multiply the specified percentage by the adjustment factor for the adjustment year;
(b) for a later adjustment year—multiply the specified percentage, as worked out under this subsection for the preceding adjustment year, by the adjustment factor for the later adjustment year.
(5B) Percentages are to be worked out under subsection (5A) to 3 decimal places (rounding up if the fourth decimal place is 5 or more).
(5C) The percentages worked out under subsection (5A) for an adjustment year apply in relation to premiums, or amounts in respect of premiums, that were paid, or that are payable, at any time in the adjustment year.
(5D) Each of the following is an adjustment year:
(a) the period of 12 months starting on 1 April 2014;
(b) the period of 12 months starting on each later 1 April.
(5E) The adjustment factor for an adjustment year is to be determined in accordance with the Private Health Insurance (Incentives) Rules. However, if the factor so determined for an adjustment year is more than 1, the adjustment factor for that year is instead taken to be 1.
Lifetime health cover loading
(6) For the purposes of applying paragraphs (1)(a), (b) and (c), reduce the amount of the premium, or the amount in respect of a premium, by any part of that amount that is attributable to an increase in the premium in accordance with Division 34.
22‑20 Meaning of share of the PHII benefit—multiple PHIIBs
If there is more than one *PHIIB in respect of the premium or amount, work out in accordance with section 22‑15 the amount of each of those PHIIB’s share of the PHII benefit, in respect of the premium or amount, on the following assumptions:
(a) assume that the PHIIB is the only person who is a PHIIB in respect of the premium or amount;
(b) assume that the premium or amount is the amount of the premium (or the amount in respect of the premium) divided by the number of persons who are PHIIBs in respect of the premium or amount.
22‑25 Application of subsection 22‑15(1) after a person 65 years or over ceases to be covered by policy
(1) If:
(a) the *PHIIB mentioned in subsection 22‑15(1) was insured under a *complying health insurance policy (the original policy) (whether or not the policy mentioned in section 22‑1) at a time before the start of the premium period mentioned in that section; and
(b) the PHIIB was not a *dependent child at that time; and
(c) at that time, another person (the entitling person) was:
(i) insured under the original policy; and
(ii) aged 65 years or over; and
(d) the entitling person subsequently ceased to be insured under the original policy;
subsection 22‑15(1) applies in relation to the complying health insurance policy mentioned in section 22‑1 as if:
(e) the entitling person were also insured under that policy; and
(f) the entitling person were the same age as the age at which he or she ceased to be insured under the original policy.
(2) Subsection (1) ceases to apply if a person (other than a *dependent child) who was not insured under the original policy at the time the entitling person ceased to be insured under it becomes insured under the *complying health insurance policy mentioned in section 22‑1.
(3) Subsection (1) does not apply if its application would result in the *PHIIB’s *share of the PHII benefit being less than it would otherwise have been.
Subdivision 22‑B—Private health insurance tiers
22‑30 Private health insurance tiers
Families
(1) The following table applies to a person (the first person) for a financial year if:
(a) on the last day of the financial year, the person is married (within the meaning of the A New Tax System (Medicare Levy Surcharge—Fringe Benefits) Act 1999); or
(b) on any day in the financial year, the person contributes in a substantial way to the maintenance of a *dependent child who is:
(i) the person’s child (within the meaning of the Income Tax Assessment Act 1997); or
(ii) the person’s sibling (including the person’s half‑brother, half‑sister, adoptive brother, adoptive sister, step‑brother, step‑sister, foster‑brother or foster‑sister) who is dependent on the person for economic support:
Private health insurance tiers—families |
Item | Column 1 For the financial year, the person is a ... | Column 2 if his or her income for surcharge purposes for the financial year exceeds the following for the financial year … | Column 3 but does not exceed the following (if applicable) for the financial year … |
1 | tier 1 earner | his or her *family tier 1 threshold | his or her *family tier 2 threshold. |
2 | tier 2 earner | his or her *family tier 2 threshold | his or her *family tier 3 threshold. |
3 | tier 3 earner | his or her *family tier 3 threshold | not applicable. |
(2) For the purposes of subsection (1), if paragraph (1)(a) applies, treat the *income for surcharge purposes for the financial year of the person to whom the first person is married (as mentioned in that paragraph) as included in the first person’s income for surcharge purposes for the financial year.
(3) Subdivision 960‑J of the Income Tax Assessment Act 1997 (Family relationships) applies to subparagraphs (1)(b)(i) and (ii) of this section in the same way as it applies to that Act.
Singles
(4) The following table applies to a person for a financial year if the table in subsection (1) does not apply to the person for the financial year:
Private health insurance tiers—singles |
Item | Column 1 For the financial year, the person is a ... | Column 2 if his or her income for surcharge purposes for the financial year exceeds the following for the financial year … | Column 3 but does not exceed the following (if applicable) for the financial year … |
1 | tier 1 earner | his or her *singles tier 1 threshold | his or her *singles tier 2 threshold. |
2 | tier 2 earner | his or her *singles tier 2 threshold | his or her *singles tier 3 threshold. |
3 | tier 3 earner | his or her *singles tier 3 threshold | not applicable. |
22‑35 Private health insurance singles thresholds
(1) A person’s singles tier 1 threshold for the 2008‑09 financial year is $70,000. This amount is indexed annually.
(2) A person’s singles tier 2 threshold for the 2010‑11 financial year is $90,000. This amount is indexed annually.
(3) A person’s singles tier 3 threshold for the 2010‑11 financial year is $120,000. This amount is indexed annually.
Note 1: A person may be a tier 1 earner, tier 2 earner or tier 3 earner if his or her income for surcharge purposes exceeds the applicable threshold for that tier: see section 22‑30.
Note 2: Section 22‑45 shows how to index amounts.
22‑40 Private health insurance family thresholds
(1) A person’s family tier 1 threshold for a financial year is an amount equal to double his or her *singles tier 1 threshold for the financial year.
(2) A person’s family tier 2 threshold for a financial year is an amount equal to double his or her *singles tier 2 threshold for the financial year.
(3) A person’s family tier 3 threshold for a financial year is an amount equal to double his or her *singles tier 3 threshold for the financial year.
(4) However, if the person has 2 or more dependants (within the meaning of the A New Tax System (Medicare Levy Surcharge—Fringe Benefits) Act 1999) who are children, increase his or her family tier 1 threshold, family tier 2 threshold and family tier 3 threshold for the financial year by the result of the following formula:

Example: If the person has 3 such dependants who are children, his or her family tier 2 threshold for the 2010‑11 financial year is:

Note: A person may be a tier 1 earner, tier 2 earner or tier 3 earner if his or her income for surcharge purposes exceeds the applicable threshold for that tier: see section 22‑30.
22‑45 Indexation
(1) This section applies in relation to an amount mentioned in section 22‑35 (Private health insurance singles thresholds).
Indexing amounts
(2) Index the amount by:
(a) firstly:
(i) if the amount is mentioned in subsection 22‑35(1) (singles tier 1 threshold)—multiplying the amount for the 2008‑2009 financial year by its *indexation factor mentioned in subsection (4); or
(ii) if the amount is mentioned in subsection 22‑35(2) or (3) (singles tier 2 threshold or singles tier 3 threshold)—multiplying the amount for the 2010‑2011 financial year by its indexation factor mentioned in subsection (5); and
(b) next, rounding the result in paragraph (a) down to the nearest multiple of $1,000.
Example 1:If the amount to be indexed is $90,000 and the indexation factor increases this to an indexed amount of $90,500, the indexed amount is rounded back down to $90,000.
Example 2:If the amount to be indexed is $120,000 and the indexation factor increases this to an indexed amount of $121,500, the indexed amount is rounded down to $121,000.
(3) Do not index the amount if its indexation factor mentioned in subsection (4) or (5) is 1 or less.
(3A) Do not index the amount for the 2015‑16, 2016‑17, 2017‑18, 2018‑19, 2019‑20 or 2020‑21 financial year.
(3B) If the amount is not indexed for a financial year because of the operation of subsection (3A), the amount for the financial year is the amount for the most recent financial year for which the amount was indexed.
Indexation factor
(4) For indexation of the amount on an annual basis in accordance with subparagraph (2)(a)(i), the indexation factor is:

(5) For indexation of the amount on an annual basis in accordance with subparagraph (2)(a)(ii), the indexation factor is:

(6) Work out the *indexation factor mentioned in subsection (4) or (5) to 3 decimal places (rounding up if the fourth decimal place is 5 or more).
Index number
(7) For calculating the amounts, the index number for a *quarter is the estimate of full‑time adult average weekly ordinary time earnings for the middle month of the quarter first published by the Australian Statistician in respect of that month.
Division 23—Premiums reduction scheme
Subdivision 23‑A—Amount of reduction
23‑1 Reduction in premiums
(1) The amount of premiums payable under a *complying health insurance policy in respect of a period is reduced in accordance with this section if a person is a *participant in the *premiums reduction scheme in respect of the policy.
(2) The amount of the reduction for each premium is the *PHII benefit in respect of the premium.
Subdivision 23‑B—Participation in the premiums reduction scheme
23‑15 Registration as a participant in the premiums reduction scheme
(1) A person may apply to a private health insurer, in the *approved form, to become a *participant in the *premiums reduction scheme in respect of a *complying health insurance policy issued by the insurer if:
(a) the insurer is a *participating insurer; and
(b) the person is a *PHIIB in respect of a premium paid or payable under the policy; and
(c) the person meets any requirements specified in the Private Health Insurance (Incentives) Rules for the purposes of this paragraph.
(2) A private health insurer that receives an application under subsection (1) must notify the Chief Executive Medicare of the application, in the *approved form, no more than 14 days (or any other period determined by the Chief Executive Medicare) after receiving the application.
(3) If notified of an application and satisfied that paragraphs (1)(a), (b) and (c) apply, the Chief Executive Medicare must register the applicant as a *participant in respect of the policy.
(4) The Chief Executive Medicare must notify the private health insurer that issued the policy if the Chief Executive Medicare registers a person as a *participant in the *premiums reduction scheme in respect of the policy.
23‑20 Refusal to register
(1) If the Chief Executive Medicare refuses to register the applicant in respect of a policy, the Chief Executive Medicare must give the applicant, and the private health insurer that issued the policy, notice of the refusal together with reasons for the refusal.
Note: Refusals to register are reviewable under Part 6‑9.
(2) The applicant is taken to be registered as a *participant in respect of the policy if the Chief Executive Medicare does not give notice of refusal within 14 days after receiving the notice under subsection 23‑15(2) from the private health insurer to which the applicant applied for registration.
23‑30 Participants who want to withdraw from scheme
(1) A *participant must notify the private health insurer that issued the policy in respect of which a person is a participant if the person no longer wishes to be registered in respect of the policy.
(2) A private health insurer must notify the Chief Executive Medicare of each notice the insurer receives under subsection (1), in the *approved form and no more than 14 days (or any other period determined by the Chief Executive Medicare) after receiving the notice.
(3) If notified under subsection (2), the Chief Executive Medicare must revoke the person’s registration in respect of the policy.
23‑35 Revocation of registration
(1) The Chief Executive Medicare must revoke a person’s registration in respect of a *complying health insurance policy if the Chief Executive Medicare is satisfied that the person is not eligible to participate in the *premiums reduction scheme in respect of the policy.
Note: Revocations of registration are reviewable under section Part 6‑9.
(2) Revocation of registration under subsection (1) does not affect a person’s right to make another application for registration under section 23‑15.
(3) The Chief Executive Medicare must give notice of the revocation of a person’s registration in respect of a *complying health insurance policy to the person, and to the private health insurer that issued the policy, within 28 days after the day on which the revocation occurs.
23‑40 Variation of registration
(1) A private health insurer must notify the Chief Executive Medicare if the treatments *covered by a *complying health insurance policy, issued by the private health insurer and in respect of which a person is a *participant, are varied.
(2) On receiving such a notice, the Chief Executive Medicare must vary the details of the registration accordingly and give notice of the variation to the private health insurer.
23‑45 Retention of applications by private health insurers
(1) A private health insurer must retain an application made to it under subsection 23‑15(1) for the period of 5 years beginning on the day on which the application was made.
(2) The private health insurer may retain the application in any form approved in writing by the Chief Executive Medicare.
(3) An application retained in such a form must be received in all courts or tribunals as evidence as if it were the original.
Part 2‑3—Lifetime health cover
Division 31—Introduction
31‑1 What this Part is about
People are encouraged to take out hospital cover by the time they turn 30. A person who is older than 30 when he or she takes out hospital cover for the first time, or who drops hospital cover for a period after having turned 30, may have to pay higher premiums for hospital cover. This scheme is known as lifetime health cover.
31‑5 Private Health Insurance (Lifetime Health Cover) Rules
Matters relating to lifetime health cover are also dealt with in the Private Health Insurance (Lifetime Health Cover) Rules. The provisions of this Part indicate when a particular matter is or might be dealt with in these Rules.
Note: The Private Health Insurance (Lifetime Health Cover) Rules are made by the Minister under section 333‑20.
Division 34—General rules about lifetime health cover
34‑1 Increased premiums for person who is late in taking out hospital cover
(1) A private health insurer must increase the amount of premiums payable for *hospital cover in respect of an *adult if the adult did not have hospital cover on his or her *lifetime health cover base day.
(2) The amount of the increase is worked out as follows:
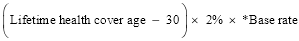
where:
base rate, for *hospital cover, is the amount of premiums that would be payable for the cover if:
(a) the premiums were not increased under this Part; and
(b) there was no discount of the kind allowed under subsection 66‑5(2).
lifetime health cover age, in relation to an *adult who takes out *hospital cover after his or her *lifetime health cover base day, means the adult’s age on the 1 July before the day on which the adult took out the hospital cover.
34‑5 Increased premiums for person who ceases to have hospital cover after his or her lifetime health cover base day
(1) A private health insurer must increase the amount of premiums payable for *hospital cover in respect of an *adult if, after the adult’s *lifetime health cover base day, the adult ceases to have hospital cover.
(2) The amount of the increase is worked out as follows:

where:
base rate is the *base rate for the *hospital cover.
years without hospital cover is the number obtained by:
(a) dividing by 365 the number of days (other than *permitted days without hospital cover), after the first day on which subsection (1) applied to the *adult, on which he or she did not have *hospital cover; and
(b) rounding up the result to the nearest whole number.
(3) Any increase under this section in the amount of premiums payable for *hospital cover is in addition to any increase under section 34‑1 in the amount of premiums payable for that hospital cover.
34‑10 Increased premiums stop after 10 years’ continuous cover
(1) A private health insurer must stop increasing the amount of premiums payable for *hospital cover in respect of an *adult under this Part if the adult has had hospital cover (including under an *applicable benefits arrangement), the premiums for which have been increased under this Part or *old Schedule 2:
(a) for a continuous period of 10 years; or
(b) for a period of 10 years that has been interrupted only by *permitted days without hospital cover or periods during which the adult was taken to have had hospital cover otherwise than because of paragraph 34‑15(2)(a) (none of which count towards the 10 years).
(2) The amount must stop being increased on the day after the last day of the 10 year period.
(3) The amount of premiums payable for *hospital cover in respect of the *adult must start to be increased under this Part again if:
(a) after the end of the 10 year period, the adult ceases to have hospital cover; and
(b) the adult later takes out hospital cover again; and
(c) the days in the period between ceasing to have the cover and taking it out again are not all *permitted days without hospital cover in respect of the adult.
(4) Subsection (3) does not prevent this section applying again in respect of any later 10 year period.
(5) In subsection (1):
old Schedule 2 means Schedule 2 to the National Health Act 1953 as in force before 1 April 2007.
34‑15 Meaning of hospital cover
(1) Hospital cover is so much of a *complying health insurance policy as *covers *hospital treatment. An *adult has hospital cover if he or she is insured under a complying health insurance policy that covers hospital treatment.
(2) An *adult is taken to have *hospital cover:
(a) at any time during which the adult was covered by an *applicable benefits arrangement; or
(b) at any time during which the adult holds a *gold card; or
(c) at any time during which the adult is in a class of adults specified in the Private Health Insurance (Lifetime Health Cover) Rules for the purposes of this paragraph.
(3) In this section:
gold card means a card that evidences a person’s entitlement to be provided with treatment:
(a) in accordance with the Treatment Principles prepared under section 90 of the Veterans’ Entitlements Act 1986; or
(b) in accordance with a determination made under section 286 of the Military Rehabilitation and Compensation Act 2004 in respect of the provision of treatment.
34‑20 Meaning of permitted days without hospital cover
(1) Any of the following days that occur after an *adult ceases, for the first time after his or her *lifetime health cover base day, to have *hospital cover are permitted days without hospital cover in respect of that adult:
(a) days on which the cover was suspended by the private health insurer in accordance with the rules for suspensions set out in the Private Health Insurance (Lifetime Health Cover) Rules;
(b) days (not counting days covered by paragraph (a)) on which the adult is *overseas that form part of a continuous period overseas of more than one year;
(c) the first 1,094 days (not counting days covered by paragraph (a) or (b)) on which the adult did not have hospital cover.
(2) The Private Health Insurance (Lifetime Health Cover) Rules may specify days that, despite subsection (1), are taken not to be *permitted days without hospital cover.
34‑25 Meaning of lifetime health cover base day
General rule: 1 July after person turns 31
(1) Subject to subsections (2), (3), (4) and (4A), a person’s lifetime health cover base day is the 1 July after the person turns 31.
Note: See also section 37‑5.
Person who had lifetime health cover base day on or before 30 June 2010
(2) If a person had a lifetime health cover base day on or before 30 June 2010, that lifetime health cover base day remains the person’s lifetime health cover base day.
Person who is not an Australian citizen and is not covered by subsection (2)
(3) Subject to subsection (4), the lifetime health cover base day of a person who is not an Australian citizen on the person’s *medicare eligibility day and is not covered by subsection (2) is the later of:
(a) the 1 July after the person turns 31; and
(b) the first anniversary of the person’s medicare eligibility day.
Note: See also section 37‑5.
Person overseas on day worked out under subsection (1) or (3)
(4) However, if the person is *overseas on the day worked out under subsection (1) or (3), the person’s lifetime health cover base day is the first anniversary of:
(a) the person’s first return to Australia from overseas; or
(b) the person’s first entry to Australia;
after the day worked out under subsection (1) or (3), whichever is applicable.
Person living on Norfolk Island at the final transition time
(4A) If:
(a) a person was living on Norfolk Island at the final transition time (within the meaning of the Norfolk Island Act 1979); and
(b) the person had turned 31 before that time;
the person’s lifetime health cover base day is the first day after the end of the 12‑month period that began at that time.
(4B) If:
(a) a person is living on Norfolk Island at the final transition time (within the meaning of the Norfolk Island Act 1979); and
(b) the person turns 31 at or after that time;
the person’s lifetime health cover base day is whichever is the later of the following:
(c) the 1 July after the person turns 31;
(d) the first day after the 12‑month period that began at that time.
Medicare eligibility day
(5) A person’s medicare eligibility day is the day on which the person is registered by the Chief Executive Medicare as an eligible person within the meaning of section 3 of the Health Insurance Act 1973.
34‑30 When a person is overseas or enters Australia
(1) Without limiting when a person is taken to be *overseas for the purposes of this Part:
(a) a person who lived on Norfolk Island before the final transition time (within the meaning of the Norfolk Island Act 1979) is taken, while the person was living on Norfolk Island before that time, to have been overseas; and
(b) any period in which a person returns to Australia for less than 90 days counts as part of a continuous period overseas.
(2) For the purposes of this Part, a person is taken not to have returned to Australia from *overseas, or entered Australia, if the person returns to Australia, or enters Australia, but remains in Australia for a period of less than 90 days.
Division 37—Exceptions to the general rules about lifetime health cover
37‑1 People born on or before 1 July 1934
(1) The amount of premiums payable for *hospital cover in respect of an *adult does not increase under this Part if the adult was born on or before 1 July 1934.
(2) However, this section does not prevent section 37‑20 applying to the *hospital cover in respect of any *adults who were born after 1 July 1934.
37‑5 People over 31 and overseas on 1 July 2000
A person:
(a) who turned 31 on or before 1 July 2000; and
(aa) who:
(i) was an Australian citizen on 1 July 2000; or
(ii) was an Australian resident (within the meaning of section 3 of the Health Insurance Act 1973) on 1 July 2000; or
(iii) had a lifetime health cover base day on or before 30 June 2010; and
(b) who was *overseas on 1 July 2000;
is taken, for the purposes of section 34‑1, to have had *hospital cover on the person’s *lifetime health cover base day.
37‑7 Person yet to turn 31
If the 1 July after a person turns 31 has not arrived, lifetime health cover does not yet apply to the person.
37‑10 Hardship cases
A person is treated for the purposes of this Part as if he or she had *hospital cover on 1 July 2000 if a determination under clause 10 of Schedule 2 to the National Health Act 1953 (as in force immediately before 1 April 2007) had effect in relation to the person immediately before 1 April 2007.
37‑15 Increases cannot exceed 70% of base rates
The maximum amount of any increase under this Part in the amount of premiums payable for *hospital cover in respect of an *adult is an amount equal to 70% of the *base rate for the hospital cover.
37‑20 Joint hospital cover
(1) If:
(a) more than one *adult is covered under the same *hospital cover; and
(b) the amount of premiums payable for the cover in respect of at least one of those adults is increased under this Part;
the amount of the premiums payable for the cover in respect of all of the adults is increased.
(2) The amount of the increase in the premiums payable for the cover is worked out by:
(a) dividing the *base rate for the cover by the number of *adults it covers; and
(b) using that rate to work out for each adult what the amount of the increase for that adult (if any) would be; and
(c) adding together the results of paragraph (b).
Division 40—Administrative matters relating to lifetime health cover
40‑1 Notification to insured people etc.
(1) A private health insurer must comply with any requirements specified in the Private Health Insurance (Lifetime Health Cover) Rules relating to providing information to:
(a) *adults in respect of *hospital cover with the private health insurer; and
(b) other adults who apply for, or inquire about, that hospital cover;
about increases under this Part in the amounts of premiums payable for hospital cover in respect of those adults.
(2) A private health insurer must comply with any requirements specified in the Private Health Insurance (Lifetime Health Cover) Rules relating to providing information to other private health insurers about increases under this Part in the amounts of premiums payable for *hospital cover with the private health insurer.
(3) The Private Health Insurance (Lifetime Health Cover) Rules may require or permit a private health insurer to provide information of a kind referred to in this section in the form of an age notionally attributed, to an *adult or other person, as the age from which the adult or other person will be treated as having had continuous *hospital cover.
(4) A private health insurer must keep separate records in relation to each *adult who has *hospital cover.
(5) When an *adult ceases to be *covered by *hospital cover under which more than one adult was covered, the private health insurer must notify each other adult that the adult has ceased to be covered by the cover.
40‑5 Evidence of having had hospital cover, or of a person’s age
A private health insurer must comply with any requirements specified in the Private Health Insurance (Lifetime Health Cover) Rules relating to whether, and in what circumstances, particular kinds of evidence are to be accepted, for the purposes of this Part, as conclusive evidence of:
(a) whether a person had *hospital cover at a particular time, or during a particular period; or
(b) a person’s age.
Chapter 3—Complying health insurance products
Part 3‑1—Introduction
Division 50—Introduction
50‑1 What this Chapter is about
Broadly, health insurance that is made available to the public must meet the requirements in this Chapter. This means that:
(a) the insurance must be community‑rated (that is, made available in a way that does not discriminate between people) (see Part 3‑2); and
(b) the insurance must be in the form of a complying health insurance product (see Part 3‑3); and
(c) the private health insurers who make the products available must meet certain obligations to people insured or seeking to be insured under the products (see Part 3‑4).
50‑5 Private Health Insurance Rules relevant to this Chapter
Matters relating to *complying health insurance products are also dealt with in the Private Health Insurance (Complying Product) Rules, the Private Health Insurance (Benefit Requirements) Rules, the Private Health Insurance (Prostheses) Rules and the Private Health Insurance (Accreditation) Rules. The provisions of this Chapter indicate when a particular matter is or may be dealt with in these Rules.
Note: These Rules are all made by the Minister under section 333‑20.
Part 3‑2—Community rating
Division 55—Principle of community rating
55‑1 What this Part is about
To ensure that everybody who chooses has access to health insurance, the principle of community rating prevents private health insurers from discriminating between people on the basis of their health or for any other reason described in this Part.
55‑5 Principle of community rating
(1) A private health insurer must not:
(a) take or fail to take any action; or
(b) in making a decision, have regard or fail to have regard to any matter;
that would result in the insurer *improperly discriminating between people who are or wish to be insured under a *complying health insurance policy of the insurer.
(2) Improper discrimination is discrimination that relates to:
(a) the suffering by a person from a chronic disease, illness or other medical condition or from a disease, illness or medical condition of a particular kind; or
(b) the gender, race, sexual orientation or religious belief of a person; or
(c) the age of a person, except to the extent allowed under Part 2‑3 (lifetime health cover) or subsection 63‑5(4); or
(d) where a person lives, except to the extent allowed under subsection 66‑10(2) or section 66‑20; or
(e) any other characteristic of a person (including but not just matters such as occupation or leisure pursuits) that is likely to result in an increased need for *hospital treatment or *general treatment; or
(f) the frequency with which a person needs hospital treatment or general treatment; or
(g) the amount or extent of the benefits to which a person becomes entitled during a period under a *complying health insurance policy, except to the extent allowed under section 66‑15; or
(h) any matter set out in the Private Health Insurance (Complying Product) Rules for the purposes of this paragraph.
(3) Despite subsection (2), discrimination by a *restricted access insurer is not improper discrimination to the extent to which the insurer:
(a) takes or fails to take an action; or
(b) in making a decision, has regard or fails to have regard to a matter;
only to ensure that its *complying health insurance products are not made available to persons to whom its constitution or *rules prohibits it from making the products available.
(4) Despite subsection (2), discrimination by a private health insurer is not improper discrimination to the extent to which:
(a) the insurer:
(i) takes or fails to take an action; or
(ii) in making a decision, has regard or fails to have regard to a matter; and
(b) taking or failing to take the action, or having regard or failing to have regard to that matter, has the effect of the premiums payable under an insurance policy that covers a person who is:
(i) employed by a particular person or body; or
(ii) under contract to provide services to a particular person or body;
being the subject of a discount or discounts (whether or not the policy also covers one or more persons who are not so employed and are not under such a contract); and
(c) the premiums meet the premium requirement in section 66‑5.
(5) To avoid doubt, subsection (4) does not apply if taking or failing to take the action, or having regard or failing to have regard to that matter, has the effect of an insurance policy being cancelled because a person ceases to be an employee of, or ceases to be under contract to provide services to, a particular employer.
55‑10 Closed products, and terminated products and product subgroups
The principle of community rating in section 55‑5 does not:
(a) prevent a private health insurer from closing a *complying health insurance product, such that the *product will not be available to anyone except those persons, who at the time of closing, are insured under a policy forming part of the product; or
(b) prevent a private health insurer from terminating a complying health insurance product or a *product subgroup of a complying health insurance product, such that:
(i) in the case of a product—the product will not be available to any person insured under a policy forming part of the product; and
(ii) in the case of a product subgroup—the product subgroup will not be available to any person insured under a policy that belongs to the product subgroup.
55‑15 Pilot projects
(1) The principle of community rating in section 55‑5 does not prevent a private health insurer from:
(a) taking or failing to take any action; or
(b) in making a decision, having regard or failing to have regard to any matter;
for the purposes of conducting a pilot project in accordance with the Private Health Insurance (Complying Product) Rules.
(2) The Private Health Insurance (Complying Product) Rules may permit pilot projects of a kind specified in the Rules to be conducted by private health insurers in accordance with requirements specified in the Rules.
Part 3‑3—Requirements for complying health insurance products
Division 60—Introduction
60‑1 What this Part is about
Complying health insurance products (which are made up of complying health insurance policies) are the only kind of insurance that private health insurers are allowed to make available as part of their health insurance business (see section 63‑1 and Division 84). This Part sets out the requirements that an insurance policy must meet in order to be a complying health insurance policy.
Division 63—Basic rules about complying health insurance products
63‑1 Obligation to ensure products are complying products
(1) A private health insurer must ensure that the only kind of insurance that it makes available as part of its *health insurance business is insurance in the form of *complying health insurance products.
(2) However, subsection (1) does not apply in relation to *health insurance business of a kind that the Private Health Insurance (Complying Product) Rules specify is excluded from subsection (1).
63‑5 Meaning of complying health insurance product
(1) A complying health insurance product is a *product made up of *complying health insurance policies.
(2) A product is all the insurance policies issued by a private health insurer:
(a) that *cover the same treatments; and
(b) that provide benefits that are worked out in the same way; and
(c) whose other terms and conditions are the same as each other.
(2A) A product subgroup, of a *product, is all the insurance policies in the product:
(a) under which the addresses of the people insured, as known to the private health insurer, are located in the same *risk equalisation jurisdiction; and
(b) under which the same kind of insured group (within the meaning of the Private Health Insurance (Complying Product) Rules) is insured.
(2B) The Private Health Insurance (Complying Product) Rules may specify insured groups for the purposes of paragraph (2A)(b). An insured group may be specified by reference to any or all of the number of people in the group, the kind of people in the group, or any other matter. A group may consist of only one person.
(3) Different premiums may be payable under policies in the same *product.
(4) A premium payable for a policy that covers an insured group of 2 or more people that includes a *dependent child non‑student may be higher than a premium payable for a policy in the same *product that covers an insured group of 2 or more people that includes one or more *dependent children but no dependent child non‑student.
(5) A dependent child non‑student is a *dependent child who:
(a) is aged between 18 and 24 (inclusive); and
(b) is not receiving full‑time education at a school, college or university.
63‑10 Meaning of complying health insurance policy
A complying health insurance policy is an insurance policy that meets:
(a) the community rating requirements in Division 66; and
(b) the coverage requirements in Division 69; and
(c) if the policy *covers *hospital treatment—the benefit requirements in Division 72; and
(d) the waiting period requirements in Division 75; and
(e) the portability requirements in Division 78; and
(f) the quality assurance requirements in Division 81; and
(g) any requirements set out in the Private Health Insurance (Complying Product) Rules for the purposes of this paragraph.
Division 66—Community rating requirements
66‑1 Community rating requirements
(1) An insurance policy meets the community rating requirements in this Division if:
(a) the policy prohibits the private health insurer that issued the policy from breaching the principle of community rating in section 55‑5 in relation to a person insured under the policy; and
(b) the policy has no terms or conditions that would allow the insurer to *improperly discriminate against a person insured under the policy; and
(c) the only discounts (if any) available under the policy are discounts allowed under subsection 66‑5(2); and
(d) unless the policy is issued under a new *product (see subsection (2))—the premiums payable under the policy meet the premium requirement in section 66‑5.
(2) For the purposes of paragraph (1)(d), an insurance policy is issued under a new *product if the amount of premiums charged under policies in the product has not changed since the first policy in the product was issued.
66‑5 Premium requirement
(1) For the purposes of paragraph 66‑1(1)(d), the premiums payable under an insurance policy for a period meet the premium requirement in this section if the amount of premiums payable under the policy for the period:
(a) is the amount specified for the *product subgroup to which the policy belongs in the most recent approval under section 66‑10; or
(b) is the proportion, for the period, of that amount; or
(c) would be the amount mentioned in paragraph (a) or (b) except that a different amount is payable:
(i) because of the application of Part 2‑3 (lifetime health cover); or
(ii) because of a discount or discounts allowed under subsection (2), if the total percentage discount (not counting discounts available for the reason in paragraph (3)(f)) does not exceed the percentage specified in the Private Health Insurance (Complying Product) Rules as the maximum percentage discount allowed; or
(iii) because of a combination of subparagraphs (i) and (ii).
(2) A discount is allowed if:
(a) it is for a reason in subsection (3); and
(b) the discount is also available for that reason under every policy in the *product; and
(c) if there are different percentage discounts available for that reason—the same percentage discount is available on the same basis under every policy in the product; and
(d) any other conditions set out in the Private Health Insurance (Complying Product) Rules are met.
(3) A discount may be for any of these reasons:
(a) because premiums are paid at least 3 months in advance;
(b) because premiums are paid by payroll deduction;
(c) because premiums are paid by pre‑arranged automatic transfer from an account at a bank or other financial institution;
(d) because the persons insured under the policy have agreed to communicate with the private health insurer, and make claims under the policy, by electronic means;
(e) because a person insured under the policy is, under the *rules of the private health insurer, treated as belonging to a contribution group;
(f) because the insurer is not required to pay a levy in relation to the policy under a law of a State or Territory;
(g) for a reason set out in the Private Health Insurance (Complying Product) Rules.
66‑10 Minister’s approval of premiums
(1) A private health insurer that proposes to change the premiums charged under a *complying health insurance product must apply to the Minister for approval of the change:
(a) in the *approved form; and
(b) at least 60 days before the day on which the insurer proposes the change to take effect.
(2) The application may propose different changes for policies in the *product, but the proposed changed amount must be the same for each policy in the product that belongs to the same *product subgroup.
(3) The Minister must, by written instrument, approve the proposed changed amount or amounts, unless the Minister is satisfied that a change that would increase the amount or amounts would be contrary to the public interest.
(4) If the Minister approves the proposed changed amount or amounts, the approval has effect:
(a) from the day specified in the approval as the day the change takes effect; and
(b) until replaced by another approval for the *product under this section.
(6) If the Minister refuses to approve the proposed changed amount or amounts, the Minister must table the Minister’s reasons for refusal in each House of the Parliament no later than 15 sitting days of that House after the refusal.
(7) An instrument made under subsection (3) is not a legislative instrument.
66‑15 Entitlement to benefits for general treatment
Neither:
(a) the community rating principle in section 55‑5; nor
(b) the community rating requirement in paragraph 66‑1(1)(b);
prevents a private health insurer from determining a person’s entitlement under a *complying health insurance policy to a benefit for *general treatment (other than *hospital‑substitute treatment) in respect of a period by having regard to the amount of benefits for that kind of treatment already claimed for the person in respect of the period.
66‑20 Different amount of benefits depending on where people live
Neither:
(a) the community rating principle in section 55‑5; nor
(b) the community rating requirements in section 66‑1;
prevents the amount of a benefit for a treatment under a *complying health insurance policy from being different from the amount of a benefit for the same treatment under another policy that is in the same *product, if the difference is only because the persons insured under the policies live in different *risk equalisation jurisdictions.
Division 69—Coverage requirements
69‑1 Coverage requirements
(1) An insurance policy meets the coverage requirements in this Division if:
(a) the only treatments the policy *covers are:
(i) specified treatments that are *hospital treatment; or
(ii) specified treatments that are hospital treatment and specified treatments that are *general treatment; or
(iii) specified treatments that are general treatment but none that are hospital‑substitute treatment; and
(b) if the policy provides a benefit for anything else—the provision of the benefit is authorised by the Private Health Insurance (Complying Product) Rules.
(2) Despite paragraph (1)(a), the policy must also *cover any treatment that a policy of its kind is required by the Private Health Insurance (Complying Product) Rules to cover.
(3) Despite paragraph (1)(a), the policy must not *cover any treatment that a policy of its kind is not allowed under the Private Health Insurance (Complying Product) Rules to cover.
69‑5 Meaning of cover
(1) An insurance policy covers a treatment if, under the policy, the insurer undertakes liability in respect of some or all loss arising out of a liability to pay fees or charges relating to the provision of goods or a service that is or includes that treatment.
(2) An insurance policy also covers a treatment if the insurer provides an insured person, or arranges for an insured person to be provided with, goods or a service that is or includes that treatment.
(3) If an insurance policy *covers a treatment in the way described in subsection (2), this Part applies as if the provision of the goods or service were a benefit provided under the policy.
69‑10 Meaning of hospital‑substitute treatment
Hospital‑substitute treatment means *general treatment that:
(a) substitutes for an episode of *hospital treatment; and
(b) is any of, or any combination of, nursing, medical, surgical, podiatric surgical, diagnostic, therapeutic, prosthetic, pharmacological, pathology or other services or goods intended to manage a disease, injury or condition; and
(c) is not specified in the Private Health Insurance (Complying Product) Rules as a treatment that is excluded from this definition.
Division 72—Benefit requirements for policies that cover hospital treatment
72‑1 Benefit requirements
(1) An insurance policy that *covers *hospital treatment meets the benefit requirements in this Division if:
(a) the policy meets the requirements in the table in subsection (2); and
(b) the policy meets any requirements specified in the Private Health Insurance (Complying Product) Rules to be benefit requirements; and
(c) the policy does not provide benefits for:
(i) the cost of care and accommodation in an aged care service (within the meaning of the Aged Care Act 1997); or
(ii) a charge for a pharmaceutical benefit supplied under Part VII of the National Health Act 1953, unless the circumstances of the charge are covered by section 92B of that Act; or
(iii) any other treatment specified in the Private Health Insurance (Complying Product) Rules as a treatment for which benefits must not be provided; and
(d) the *rules of the private health insurer that issues the policy meet the rules requirement in section 72‑5.
(2) These are the requirements that a policy must meet for the purposes of paragraph (1)(a):
Requirements that a policy that *covers *hospital treatment must meet |
Item | There must be a benefit for ... | The amount of the benefit must be ... |
1 | any part of *hospital treatment that is one or more of the following: (a) psychiatric care; (b) rehabilitation; (c) palliative care; if the treatment is provided in a *hospital and no *medicare benefit is payable for that part of the treatment. | at least the amount set out, or worked out using the method set out, in the Private Health Insurance (Benefit Requirements) Rules as the minimum benefit, or method for working out the minimum benefit, for that treatment. |
2 | *hospital treatment *covered under the policy for which a *medicare benefit is payable. | (a) if the charge for the treatment is less than the *schedule fee for the treatment—so much of the charge (if any) as exceeds 75% of the schedule fee; and (b) otherwise—at least 25% of the schedule fee for the treatment. |
3 | if the policy *covers *hospital‑substitute treatment—hospital‑substitute treatment covered under the policy for which a *medicare benefit is payable. | (a) if the charge for the treatment is less than the *schedule fee for the treatment—so much of the charge (if any) as exceeds 75% of the schedule fee; and (b) otherwise—at least 25% of the schedule fee for the treatment; but the benefit must not be provided if a medicare benefit of an amount that is at least 85% of the schedule fee is claimed for the treatment. |
4 | (a) *hospital treatment *covered under the policy; and (b) if the policy covers *hospital‑substitute treatment—hospital‑substitute treatment covered under the policy; that is the provision of a prosthesis, of a kind listed in the Private Health Insurance (Prostheses) Rules, as described in either of the following paragraphs: (c) the prosthesis is provided in circumstances in which a *medicare benefit is payable, and, if those Rules set out conditions that must be satisfied in relation to the provision of the prosthesis in those circumstances, those conditions are satisfied; (d) the prosthesis is provided in other circumstances set out in those Rules, and, if those Rules set out conditions that must be satisfied in relation to the provision of the prosthesis in those circumstances, those conditions are satisfied. | (a) at least the amount set out, or worked out using the method set out, in the Private Health Insurance (Prostheses) Rules as the minimum benefit, or method for working out the minimum benefit, for the prosthesis; and (b) if the Private Health Insurance (Prostheses) Rules set out an amount, or a method for working out an amount, as the maximum benefit, or method for working out the maximum benefit, for the prosthesis—no more than that amount or the amount worked out using that method. |
5 | any treatment for which the Private Health Insurance (Benefit Requirements) Rules specify there must be a benefit. | at least the amount set out, or worked out using the method set out, in the Private Health Insurance (Benefit Requirements) Rules as the minimum benefit, or method for working out the minimum benefit, for that treatment. |
Note: If a private health insurer provides an insured person with, or arranges for an insured person to be provided with, treatment, it is treated as a benefit for the purposes of this Division (see subsection 69‑5(3)).
72‑5 Rules requirement in relation to provision of benefits
(1) For the purposes of paragraph 72‑1(1)(d), the *rules of the private health insurer that issues the policy meet the rules requirement in this section if the rules have the effect required by subsection (2).
(2) The effect required is that if, under an agreement or arrangement with a private health insurer, a particular *health care provider (other than a *medical practitioner) provides particular *hospital treatment or *hospital‑substitute treatment to people insured under the same *complying health insurance product of the insurer, any charge for the treatment:
(a) that is payable by an insured person; and
(b) which is not recoverable by a benefit under the product;
must be the same for all of the people insured under the product, irrespective of:
(c) the frequency with which that provider provides that particular treatment to people insured under that product; or
(d) any other matter.
(3) The Private Health Insurance (Complying Product) Rules may modify the effect required by subsection (2) in relation to all or particular kinds of *complying health insurance products, benefits, treatments or *health care providers. To the extent the Rules do so, the rules requirement is taken to be met if the conditions in the Rules are met.
72‑10 Minimum benefits for prostheses
(1) Private Health Insurance (Prostheses) Rules made for the purposes of item 4 of the table in subsection 72‑1(2) must only list a kind of prosthesis if:
(a) an application has been made under subsection (2) in relation to that kind of prosthesis; and
(b) the Minister has granted the application.
(2) A person may apply to the Minister to have the Private Health Insurance (Prostheses) Rules list a prosthesis of the kind to which the application relates.
(3) The application must be:
(a) in the *approved form; and
(b) accompanied by any application fee imposed under the Private Health Insurance (Prostheses Application and Listing Fees) Act 2007.
(4) The Minister must inform the applicant in writing of the Minister’s decision whether or not to grant the application. If the Minister decides not to grant the application, the Minister must also inform the applicant of the reason for that decision.
(5) If:
(a) the Minister grants the application; and
(b) the applicant pays to the Commonwealth any initial listing fee imposed under the Private Health Insurance (Prostheses Application and Listing Fees) Act 2007 within 14 days of being informed of the Minister’s decision to grant the application;
the Minister must, on the next occasion when the Minister makes or varies the Private Health Insurance (Prostheses) Rules:
(c) list the kind of prosthesis to which the application relates in those Rules; and
(d) set out in those Rules a minimum benefit for the prosthesis; and
(e) if the Minister considers it appropriate—set out in those Rules a maximum benefit for the prosthesis.
(6) The Private Health Insurance (Prostheses) Rules may set out criteria (listing criteria) to be satisfied in order for an application (a listing application) made under subsection (2) to be granted. The Rules may provide for different listing criteria to apply in different circumstances.
(7) The Minister must not grant a listing application if any applicable listing criteria are not satisfied in relation to the application.
Note: The Minister may refuse to grant a listing application even if the applicable listing criteria are satisfied.
72‑15 Ongoing listing fee for prostheses
(1) This section applies if the Minister lists a kind of prosthesis in the Private Health Insurance (Prostheses) Rules as a result of an application under subsection 72‑10(2).
(2) The applicant must pay to the Commonwealth the ongoing listing fee for which the applicant is liable under the Private Health Insurance (Prostheses Application and Listing Fees) Act 2007, within 28 days of each day specified under that Act as an ongoing listing fee imposition day.
(3) If the applicant fails to pay an ongoing listing fee in accordance with subsection (2), the Minister may remove the kind of prosthesis from the list in the Private Health Insurance (Prostheses) Rules.
72‑20 Other matters
The Private Health Insurance (Prostheses) Rules may, in relation to application fees, initial listing fees or ongoing listing fees imposed under the Private Health Insurance (Prostheses Application and Listing Fees) Act 2007, provide for, or for matters relating to, any or all of the following:
(a) methods for payment;
(b) extending the time for payment;
(c) refunding or otherwise applying overpayments.
Division 75—Waiting period requirements
75‑1 Waiting period requirements
(1) An insurance policy meets the waiting period requirements in this Division if the *waiting period that applies to a person who did not *transfer to the policy is no longer than:
(a) for a benefit for *hospital treatment or *hospital‑substitute treatment that is obstetric treatment or treatment for a *pre‑existing condition (other than treatment covered by paragraph (b))—12 months; and
(b) for a benefit for hospital treatment or hospital‑substitute treatment that is psychiatric care, rehabilitation or palliative care (whether or not for a pre‑existing condition)—2 months; and
(c) for any other benefit for hospital treatment or hospital‑substitute treatment—2 months.
(2) The Private Health Insurance (Complying Product) Rules may modify the requirements in subsection (1) in relation to all or particular kinds of private health insurers, benefits or insured persons. To the extent the Rules do so, the waiting period requirements in this Division are taken to be met if the conditions in the Rules are met.
Note: If a private health insurer provides an insured person with, or arranges for an insured person to be provided with, treatment, it is treated as a benefit for the purposes of this Division (see subsection 69‑5(3)).
75‑5 Meaning of waiting period
The waiting period that applies to a person for a benefit under an insurance policy is the period:
(a) starting at the time the person becomes insured under the policy; and
(b) ending at the time specified in the policy;
during which the person is not entitled to the benefit.
75‑10 Meaning of transfers
A person transfers to a policy (the new policy) from another policy (the old policy) if:
(a) either:
(i) the person is insured under the old policy at the time the person becomes insured under the new policy; or
(ii) the person ceased to be insured under the old policy no more than 7 days, or a longer number of days allowed by the new policy’s insurer for this purpose, before becoming insured under the new policy; and
(b) the old policy is a *complying health insurance policy; and
(c) the person’s premium payments under the old policy were up to date at the time the person became insured under the new policy.
Note: See section 99‑1 about transfer certificates.
75‑15 Meaning of pre‑existing condition
(1) A person insured under an insurance policy has a pre‑existing condition if:
(a) the person has an ailment, illness or condition; and
(b) in the opinion of a *medical practitioner appointed by the insurer that issued the policy, the signs or symptoms of that ailment, illness or condition existed at any time in the period of 6 months ending on the day on which the person became insured under the policy.
(2) In forming an opinion for the purposes of paragraph (1)(b), the *medical practitioner must have regard to any information in relation to the ailment, illness or condition that the medical practitioner who treated the ailment, illness or condition gives him or her.
(3) If:
(a) a private health insurer replaces a *complying health insurance product with another complying health insurance product; and
(b) a person who was insured under a policy that was in the replaced *product is *transferred by the insurer to a policy that is in the replacement product;
the reference in paragraph (1)(b) to the day on which the person became insured under the policy is taken to be a reference to the day on which the person became insured under the replaced policy.
Division 78—Portability requirements
78‑1 Portability requirements
(1) An insurance policy meets the portability requirements in this Division if the policy meets the requirements in subsections (2), (3), (4) and (5A).
(2) An insurance policy meets the requirement in this subsection if the *waiting period that applies to a person who *transferred to the policy (the new policy) from another policy (the old policy) is no longer than:
(a) for a benefit for *hospital treatment or *hospital‑substitute treatment that was not *covered under the old policy—the period allowed under section 75‑1; and
(b) for a benefit for hospital treatment or hospital‑substitute treatment that was covered under the old policy—the balance of any unexpired waiting period for that benefit that applied to the person under the old policy.
(3) An insurance policy meets the requirement in this subsection if the policy does not impose on a person who *transferred to the policy any period (other than a *waiting period allowed under subsection (2)) during which the amount of a benefit in relation to any particular *hospital treatment or *hospital‑substitute treatment is less than the amount the person would be eligible for during any other period.
(4) An insurance policy meets the requirement in this subsection if, in relation to a benefit for *hospital treatment or *hospital‑substitute treatment:
(a) that was *covered under the old policy; and
(b) in respect of which a higher excess or higher co‑payment applied under the old policy than is the case under the new policy;
any period during which the higher excess or higher co‑payment continues to apply under the new policy to a person who *transferred to the policy is no longer than the *waiting period allowed under section 75‑1 for a benefit for that treatment.
(5) In working out:
(a) for the purposes of subsection (2) or (4), whether a treatment was *covered under an old policy; or
(b) for the purposes of subsection (3), whether the amount of a benefit under a new policy during a period is less than the amount it would be during another period;
disregard the existence or otherwise of contracts between the insurer in relation to either of the policies and particular *health care providers or groups of health care providers.
(5A) An insurance policy meets the requirement in this subsection if:
(a) the policy forms part of a *complying health insurance product or belongs to a *product subgroup of a complying health insurance product; and
(b) the *product or product subgroup is being terminated by the private health insurer, and as a consequence, an *adult insured under the policy is to be transferred to a new policy; and
(c) the insurer informs the adult insured under the policy, in writing, of the matters set out in the Private Health Insurance (Complying Product) Rules; and
(d) the adult insured under the policy is informed of those matters a reasonable time before the transfer to the new policy is to take effect.
Note: See also section 55‑10.
(6) The Private Health Insurance (Complying Product) Rules may modify the requirements in this section in relation to all or particular kinds of private health insurers, benefits or insured persons. To the extent the Rules do so, the portability requirements in this Division are taken to be met if the conditions in the Rules are met.
Note: If a private health insurer provides an insured person with, or arranges for an insured person to be provided with, treatment, it is treated as a benefit for the purposes of this Division (see subsection 69‑5(3)).
Division 81—Quality assurance requirements
81‑1 Quality assurance requirements
An insurance policy meets the quality assurance requirements in this Division if the policy prohibits the payment of benefits for a treatment that does not meet the standards in the Private Health Insurance (Accreditation) Rules.
Note: The Private Health Insurance (Accreditation) Rules are made by the Minister under section 333‑20.
Division 84—Enforcement of this Part
84‑1 Offence: advertising, offering or insuring under non‑complying policies
(1) A person commits an offence if:
(a) the person:
(i) advertises a *product; or
(ii) offers a person insurance under a policy; or
(iii) insures a person under a policy; or
(iv) arranges for another person to do a thing mentioned in subparagraph (i), (ii) or (iii); and
(b) the insurance under the policy, or under a policy in the product, is *health insurance business; and
(c) the policy is not a *complying health insurance policy; and
(d) the *health insurance business is not business of a kind specified in the Private Health Insurance (Complying Product) Rules as excluded from subsection 63‑1(1).
Penalty: 1,000 penalty units or imprisonment for 5 years, or both.
(2) In imposing a penalty on a private health insurer for an offence under subsection (1), the court:
(a) must have regard to the possible impact of a penalty on the insurer’s capital adequacy, solvency and the level of premiums for its *complying health insurance products; and
(b) must not impose a penalty if satisfied that doing so would adversely affect the insurer’s capital adequacy or solvency, or be likely to lead to an increase in premiums for its products.
84‑5 Offence: directors and chief executive officers liable if systems not in place to prevent breaches
A person commits an offence if:
(a) the person is a *director or *chief executive officer of a private health insurer; and
(b) the insurer commits an offence under section 84‑1; and
(c) the person failed to exercise due diligence to ensure that adequate systems were in place to prevent the insurer from committing the offence.
Penalty: 1,000 penalty units or imprisonment for 5 years, or both.
84‑10 Injunction in relation to non‑complying policies
(1) If a private health insurer has engaged, is engaging, or is proposing to engage, in conduct:
(a) that contravenes or would contravene section 63‑1; or
(b) that is or that would be an offence against section 84‑1;
the Federal Court may, on application by a person mentioned in subsection (3), grant an injunction restraining the insurer from engaging in the conduct.
(2) If:
(a) a private health insurer has refused or failed, is refusing or failing, or is proposing to refuse or fail, to do a thing; and
(b) the refusal or failure:
(i) contravenes or would contravene section 63‑1; or
(ii) is or would be an offence against section 84‑1;
the Federal Court may, on application by a person mentioned in subsection (3), grant an injunction requiring the insurer to do the thing.
(3) For the purposes of subsections (1) and (2), an application may be made by:
(a) the Minister; or
(c) any other person.
(4) The court may grant an interim injunction pending the determination of an application under subsection (1) or (2).
(5) The court must not require an applicant for an injunction to give an undertaking as to damages as a condition of granting an interim injunction.
(6) The court may discharge or vary an injunction granted under this section.
(7) The power of the court to grant an injunction restraining a private health insurer from engaging in conduct may be exercised:
(a) whether or not it appears to the court that the insurer intends to engage again, or to continue to engage, in conduct of that kind; and
(b) whether or not the insurer has previously engaged in conduct of that kind.
(8) The power of the court to grant an injunction requiring a private health insurer to do a thing may be exercised:
(a) whether or not it appears to the court that the insurer intends to refuse or fail again, or to continue to refuse or fail, to do that thing; and
(b) whether or not the insurer has previously refused or failed to do that thing.
84‑15 Remedies for people affected by non‑complying policies
On application by the Minister, if the Federal Court is satisfied that:
(a) a private health insurer has engaged in conduct that contravenes section 63‑1 or is an offence against section 84‑1; or
(b) both:
(i) a private health insurer has refused or failed to do a thing; and
(ii) that refusal or failure contravenes section 63‑1 or is an offence against section 84‑1;
the court may order the insurer to do either or both of the following:
(c) take specified action to ensure that an insurance policy becomes a *complying health insurance policy;
(d) take specified action to ensure that a person insured under an insurance policy is put in the position the person would have been in, had the policy always been a complying health insurance policy.
Part 3‑4—Obligations relating to complying health insurance products
Division 90—Introduction
90‑1 What this Part is about
Private health insurers have obligations to people insured under their complying health insurance products and people seeking to become insured under those products. Private health insurers also have to keep the Department and the Private Health Insurance Ombudsman informed about their health insurance business.
Division 93—Giving information to consumers
93‑1 Maintaining up to date standard information statements
(1) A private health insurer must ensure that it maintains at all times an *up to date *standard information statement:
(a) for each *product subgroup of each *complying health insurance product that it makes available; and
(b) for each product subgroup of each complying health insurance product under which it insures people.
(1A) A single *standard information statement may be the standard information statement for more than one *product subgroup of a *complying health insurance product if the premiums payable under policies in the subgroups the statement covers are the same.
(2) The *standard information statement for a *product subgroup of a *complying health insurance product is up to date at a particular time, if, at that time, the information in the statement is accurate.
(3) A private health insurer commits an offence if there is no *standard information statement for a *product subgroup of a *complying health insurance product of the insurer.
Penalty: 60 penalty units.
(4) A private health insurer commits an offence if:
(a) there is a *standard information statement for a *product subgroup of a *complying health insurance product of the insurer; and
(b) the standard information statement is not *up to date.
Penalty: 60 penalty units.
(5) Strict liability applies to subsections (3) and (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
93‑5 Meaning of standard information statement
(1) A standard information statement for a *product subgroup of a *complying health insurance product is a statement about the product subgroup that contains the information, and is in the form, set out in the Private Health Insurance (Complying Product) Rules.
(2) The Private Health Insurance (Complying Product) Rules may set out methods by which *standard information statements are to be made available to people who ask for information about *complying health insurance products.
93‑10 Making standard information statements available
A private health insurer must ensure that, if a person asks an *officer, employee or agent of the insurer for information about a *complying health insurance product of the insurer:
(a) the person is told about the *standard information statement for the *product subgroup that is likely to apply to the person and how to obtain a copy of the statement; and
(b) if the person asks for a copy—the person is given an *up to date copy of the statement for that subgroup.
93‑15 Giving information to newly insured people
(1) A private health insurer must ensure that, when an *adult first becomes insured under a *complying health insurance policy of the insurer, the adult is given:
(a) an *up to date copy of the *standard information statement for the *product subgroup that the policy belongs to, by a method (if any) set out in the Private Health Insurance (Complying Product) Rules; and
(b) details about what the policy *covers and how benefits provided under it are worked out; and
(c) a statement identifying the *health benefits fund to which the policy is referable.
(2) If more than one *adult becomes insured under a single *complying health insurance policy of a private health insurer, the insurer is taken to comply with subsection (1) if the insurer complies with that subsection in relation to only one of those adults.
93‑20 Keeping insured people up to date
(1) A private health insurer must ensure that an *adult insured under a *complying health insurance policy issued by the insurer is given the *standard information statement for the *product subgroup that the policy belongs to, at least once every 12 months.
(2) A private health insurer must ensure that, if a proposed change to the insurer’s *rules:
(a) is or might be detrimental to the interests of an insured person; and
(b) will require an update to the *standard information statements for a *complying health insurance product of the insurer;
an *adult insured under each *complying health insurance policy in the product:
(c) is informed about the proposed change a reasonable time before the change takes effect; and
(d) is given the updated standard information statement for the *product subgroup that the policy belongs to as soon as practicable after the statement is updated.
(3) A private health insurer must ensure that, if an *adult who is insured under a *complying health insurance policy of the insurer asks an *officer, employee or agent of the insurer for information about what the policy covers or the benefits the policy provides, the adult is given the information as soon as practicable.
(4) If a private health insurer changes the *health benefits fund to which a *complying health insurance policy of the insurer is *referable, the insurer must ensure that:
(a) before the change takes effect, an *adult insured under the policy is given a statement identifying the health benefits fund to which the policy will be referable as a result of the change; or
(b) within 2 weeks after the change takes effect, an adult insured under the policy is given a statement identifying the health benefits fund to which the policy is referable as a result of the change.
Note: The health benefits fund to which a policy is referable may change in accordance with Division 4 of Part 3 of the Private Health Insurance (Prudential Supervision) Act 2015.
(5) If more than one *adult is insured under a single *complying health insurance policy of a private health insurer, the insurer is taken to comply with subsection (1), (2) or (4) if the insurer complies with the subsection in relation to only one of those adults.
93‑25 Giving advance notice of detrimental changes to rules
(1) A private health insurer must ensure an *adult insured under a *complying health insurance policy issued by the insurer is informed about any proposed change to the insurer’s *rules (other than a change to which subsection 93‑20(2) applies), a reasonable time before the change takes effect, if the proposed change is or might be detrimental to the interests of an insured person.
(2) If more than one *adult is insured under a single *complying health insurance policy of a private health insurer, the insurer is taken to comply with subsection (1) if the insurer complies with that subsection in relation to only one of those adults.
93‑30 Failure to give information to consumers
(1) A private health insurer commits an offence if:
(a) the insurer is required under section 93‑10, 93‑15, 93‑20 or 93‑25 to ensure that a particular thing happens in relation to a particular person; and
(b) the thing does not happen in relation to the person.
Penalty: 60 penalty units.
(2) Strict liability applies to subsection (1).
Note: For strict liability, see section 6.1 of the Criminal Code.
Division 96—Giving information to the Department and the Private Health Insurance Ombudsman
96‑1 Giving standard information statements on request
A private health insurer must ensure that, if:
(a) the Secretary of the Department; or
(c) the Private Health Insurance Ombudsman;
requests the private health insurer for the *standard information statements for a *complying health insurance product of the insurer, the insurer gives the person who made the request *up to date copies of the statements, as soon as practicable after being asked and by the method (if any) specified by the person.
96‑5 Giving standard information statements for new products
A private health insurer must ensure that copies of the *standard information statements for a *complying health insurance product of the insurer are given to:
(a) the Secretary of the Department; and
(c) the Private Health Insurance Ombudsman;
no later than the first day on which the insurer first begins to make the *product available.
96‑10 Giving updated standard information statements
A private health insurer must ensure that, if the *standard information statements for a *complying health insurance product of the insurer are updated, copies of the updated statements are given to:
(a) the Secretary of the Department; and
(c) the Private Health Insurance Ombudsman;
as soon as practicable after the statement is updated.
96‑15 Giving additional information on request
(1) Any of the following:
(a) the Secretary of the Department;
(c) the Private Health Insurance Ombudsman;
may request a private health insurer for specified information about, or in relation to, a *complying health insurance product or products, or a *complying health insurance policy, of the insurer.
(2) The request must:
(a) be in writing; and
(b) specify the time by which the information requested is to be given.
(3) The request may specify the manner and form in which the information requested is to be given.
(4) A private health insurer must ensure that the request is complied with, by the time specified in the request or any longer time allowed by the person who made the request.
96‑20 Failure to give information to Department or Private Health Insurance Ombudsman
(1) A private health insurer commits an offence if:
(a) the insurer is required under section 96‑1, 96‑5, 96‑10 or 96‑15 to ensure that a particular thing is given to a particular person; and
(b) the thing is not given to the person.
Penalty: 60 penalty units.
(2) Strict liability applies to subsection (1).
Note: For strict liability, see section 6.1 of the Criminal Code.
96‑25 Giving information required by the Private Health Insurance (Complying Product) Rules
The Private Health Insurance (Complying Product) Rules may set out any or all of the following:
(a) information in relation to *complying health insurance products;
(b) persons to whom the information is to be given (who may include, but need not be limited to, the Secretary of the Department or the Private Health Insurance Ombudsman);
(c) the time within which, or the intervals at which, the information is to be given to a person;
(d) the manner and form in which the information is to be given to a person.
Division 99—Transfer certificates
99‑1 Transfer certificates
Certificate for the insured person
(1) A private health insurer (the old insurer) must, if a person ceases to be insured under a *complying health insurance policy of the insurer and does not become insured under another policy of the insurer, give the person a certificate under this subsection:
(a) in the *approved form; and
(b) within the period set out in the Private Health Insurance (Complying Product) Rules.
Certificate for the new insurer
(2) A private health insurer (the new insurer) must request a certificate from an old insurer if:
(a) a person who is or has been insured under a *complying health insurance policy of the old insurer *transfers to a complying health insurance policy of the new insurer; and
(b) the person does not give the new insurer the certificate the old insurer gave the person under subsection (1) within 7 days of becoming insured by the new insurer.
The request must be made:
(c) in the *approved form; and
(d) within the period set out in the Private Health Insurance (Complying Product) Rules.
(2A) A private health insurer must not request a certificate except in the circumstances set out in subsection (2).
(3) If a certificate is requested by the new insurer (whether or not the request is in the *approved form or made within the period mentioned in paragraph (2)(d)), the old insurer must give the new insurer a certificate:
(a) in the approved form; and
(b) within the period set out in the Private Health Insurance (Complying Product) Rules.
Offence
(4) A private health insurer commits an offence if:
(a) the insurer is required to do a thing under subsection (1), (2) or (3); and
(b) the insurer does not do the thing.
Penalty: 60 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
Division 102—Private health insurers to offer cover for hospital treatment
102‑1 Private health insurers to offer cover for hospital treatment
At any time when a private health insurer makes available a *complying health insurance product that *covers *general treatment, the insurer must also make available a complying health insurance product that covers *hospital treatment.
Chapter 4—Health insurance business, health benefits funds and miscellaneous obligations of private health insurers
Part 4‑1—Introduction
Division 110—Introduction
110‑1 What this Chapter is about
This Chapter defines the key concepts of health insurance business and health benefits funds. It also deals with some related matters and imposes miscellaneous obligations on private health insurers.
Part 4‑2—Health insurance business
Division 115—Introduction
115‑1 What this Part is about
This Part defines the key concept of health insurance business.
Note: Entities are only permitted to carry on health insurance business if they are registered under Division 3 of Part 2 of the Private Health Insurance (Prudential Supervision) Act 2015.
115‑5 Private Health Insurance (Health Insurance Business) Rules
(1) The Private Health Insurance (Health Insurance Business) Rules also deal with matters relating to *health insurance business. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Health Insurance Business) Rules are made by the Minister under section 333‑20.
(2) Before making Private Health Insurance (Health Insurance Business) Rules, the Minister must consult *APRA. However, a failure to consult APRA does not affect the validity of those Rules.
Note: This consultation requirement also applies to any repeal or amendment of such Rules: see subsection 33(3) of the Acts Interpretation Act 1901.
115‑10 Whether a business etc. is health insurance business
The following diagram shows how to work out whether a business or arrangement is *health insurance business:

Division 121—What is health insurance business?
121‑1 Meaning of health insurance business
(1) Health insurance business is:
(a) the business of undertaking liability, by way of insurance; or
(b) an *employee health benefits scheme;
that relates, in a way referred to in subsection (2), to *hospital treatment or *general treatment.
Note: The following kinds of insurance business are not health insurance business:
(a) accident and sickness insurance business (see section 121‑20);
(b) liability insurance business (see section 121‑25);
(c) insurance business excluded by the Private Health Insurance (Health Insurance Business) Rules (see section 121‑30).
(2) The liability by way of insurance, or the arrangement to make payments under the *employee health benefits scheme, must relate to:
(a) loss arising out of a liability to pay fees or charges relating to provision in Australia of such treatment; or
(b) provision in Australia of such treatment; or
(c) the happening of an occurrence connected with the provision in Australia of such treatment; or
(d) the happening of an occurrence in Australia that ordinarily requires the provision of such treatment.
(3) It does not matter for the purposes of paragraph (2)(d) whether payment of benefits to the insured is dependent upon one or more of the following:
(a) such treatment or benefit being provided to the insured;
(b) the insured requiring such treatment or benefit;
(c) fees or charges being payable by the insured in relation to the provision of such treatment or benefit.
121‑5 Meaning of hospital treatment
(1) Hospital treatment is treatment (including the provision of goods and services) that:
(a) is intended to manage a disease, injury or condition; and
(b) is provided to a person:
(i) by a person who is authorised by a *hospital to provide the treatment; or
(ii) under the management or control of such a person; and
(c) either:
(i) is provided at a hospital; or
(ii) is provided, or arranged, with the direct involvement of a hospital.
(2) Without limiting subsection (1), hospital treatment includes any other treatment, or treatment included in a class of treatments, specified in the Private Health Insurance (Health Insurance Business) Rules for the purposes of this subsection.
(3) Without limiting subsection (1) or (2), the reference to treatment in those subsections includes a reference to any of, or any combination of, accommodation, nursing, medical, surgical, podiatric surgical, diagnostic, therapeutic, prosthetic, pharmacological, pathology or other services or goods intended to manage a disease, injury or condition.
(4) Despite subsections (1) and (2), treatment is not *hospital treatment if it is specified in, or is included in a class of treatments specified in, the Private Health Insurance (Health Insurance Business) Rules for the purposes of this subsection.
(5) A hospital is a facility for which a declaration under subsection (6) is in force.
(6) The Minister may, in writing:
(a) declare that a facility is a *hospital; or
(b) revoke such a declaration.
Note: Refusals to make declarations, and revocations of declarations are reviewable under Part 6‑9.
(7) In deciding whether to declare that a facility is a *hospital, or to revoke such a declaration, the Minister must have regard to:
(a) the nature of the facility; and
(b) the range and scope of the services provided, or proposed to be provided, under the management or control of the facility and at or on behalf of the facility; and
(c) whether the necessary approvals by a State or Territory, or by an authority of a State or Territory, have been obtained in relation to the facility; and
(d) whether the accreditation requirements of an appropriate accrediting body have been met; and
(e) whether undertakings have been made, or have been complied with, relating to providing to private health insurers information, of the kind specified in the Private Health Insurance (Health Insurance Business) Rules, relating to treatment of persons insured under *complying health insurance products that are *referable to *health benefits funds; and
(ea) if the Minister is deciding whether to revoke such a declaration—any contravention of conditions to which the declaration is subject; and
(f) any other matters specified in the Private Health Insurance (Health Insurance Business) Rules.
(8) A declaration under subsection (6) that a facility is a *hospital must include either a statement that the hospital is a public hospital or a statement that the hospital is a private hospital.
121‑7 Conditions on declarations of hospitals
(1) A declaration under paragraph 121‑5(6)(a) that a facility is a hospital is subject to:
(a) any conditions specified under subsection (2); and
(b) any conditions that the Minister specifies under subsection (3) in relation to the facility.
Note: Decisions by the Minister to specify conditions in relation to particular facilities are reviewable under Part 6‑9.
(2) The Private Health Insurance (Health Insurance Business) Rules may specify conditions to which declarations under paragraph 121‑5(6)(a) are subject. Any conditions so specified apply to all such declarations, whether or not the declarations were made before the conditions were so specified.
(3) The Minister may specify:
(a) in a declaration under paragraph 121‑5(6)(a) relating to a facility; or
(b) in a written notice given to a facility for which such a declaration is already in force;
conditions, or additional conditions, to which the declaration is subject.
(4) A contravention of a condition to which a declaration under paragraph 121‑5(6)(a) is subject does not cause the declaration to cease to have effect.
Note: Contraventions are taken into consideration in deciding whether to revoke a declaration.
121‑10 Meaning of general treatment
(1) General treatment is treatment (including the provision of goods and services) that:
(a) is intended to manage or prevent a disease, injury or condition; and
(b) is not *hospital treatment.
(2) Without limiting subsection (1), general treatment includes any other treatment, or treatment included in a class of treatments, specified in the Private Health Insurance (Health Insurance Business) Rules for the purposes of this subsection.
(3) Despite subsections (1) and (2), neither of the following is *general treatment:
(a) the rendering in Australia of a service for which *medicare benefit is payable, unless the Private Health Insurance (Health Insurance Business) Rules provide otherwise;
(b) any other treatment, or treatment included in a class of treatments, specified in the Private Health Insurance (Health Insurance Business) Rules for the purposes of this paragraph.
121‑15 Extension to employee health benefits schemes
(1) An arrangement is an employee health benefits scheme if:
(a) the arrangement provides for a person (an employer) to arrange payment in respect of the whole or part of the fees and charges that an employee of, or a person providing services to, the employer incurred in relation to *hospital treatment or *general treatment; and
(b) one or more of the following applies:
(i) the employer is a *constitutional corporation;
(ii) the employer is a body corporate incorporated in a Territory;
(iii) the employer carries on business in a Territory.
(2) It does not matter for the purposes of this section whether the arrangement:
(a) constitutes a business of undertaking liability by way of insurance; or
(b) is a minor or incidental part of the employer’s business; or
(c) does not require the employee, or person providing services, to pay any contributions; or
(d) does not require the employee, or person providing services, to pay contributions that reflect the value of the benefits that the employer is providing under the arrangement; or
(e) provides for the employer to make payments in relation to *hospital treatment, or *general treatment, provided to a person other than the employee or person providing services; or
(f) confers on the employer or another person a discretion whether to make payments.
(3) However, an arrangement:
(a) is not an *employee health benefits scheme merely because, under the arrangement, the employer will pay, or will reimburse employees, or persons providing services, for payment of, one or both of the following:
(i) the premiums payable by them for *complying health insurance policies;
(ii) the difference between benefits payable to them under policies, and amounts that they are liable to pay, for health services provided to them or members of their families; and
(b) is not an employee health benefits scheme if the Private Health Insurance (Health Insurance Business) Rules provide that:
(i) it is not an employee health benefits scheme; or
(ii) arrangements of a class in which it is included are not employee health benefits schemes; and
(c) is not an employee health benefits scheme to the extent (if any) that the arrangement constitutes State insurance within the meaning of paragraph 51(xiv) of the Constitution.
121‑20 Exception: accident and sickness insurance business
(1) Despite section 121‑1, *health insurance business does not include the business of undertaking liability, by way of insurance, to pay a lump sum, or to make periodic payments, on the happening of a personal accident, disease or sickness.
(2) However, this section does not apply to:
(a) business where liability is undertaken with respect to loss arising out of a liability to pay fees or charges in relation to the provision in Australia of *hospital treatment or *general treatment; or
(b) business of a kind specified in the Private Health Insurance (Health Insurance Business) Rules for the purposes of this paragraph.
121‑25 Exception: liability insurance business
Despite section 121‑1, *health insurance business does not include the business of undertaking liability, by way of insurance, with respect to any loss arising out of a liability to pay compensation or damages, including:
(a) a liability to pay compensation or damages because of the use of a motor vehicle; or
(b) a liability to pay compensation or damages to an employee because of an event occurring in connection with the employee’s employment.
121‑30 Exception: insurance business excluded by the Private Health Insurance (Health Insurance Business) Rules
Despite section 121‑1, *health insurance business does not include a business of a kind that the Private Health Insurance (Health Insurance Business) Rules state not to be a health insurance business.
Part 4‑4—Health benefits funds
Division 131—Health benefits funds
131‑1 What this Part is about
This Part defines the key concept of a health benefits fund.
This Part also defines the concepts of health‑related business and risk equalisation jurisdictions, and deals with some related matters (including the operation of health‑related businesses through health benefits funds).
Note: The Private Health Insurance (Prudential Supervision) Act 2015 requires private health insurers to have health benefits funds. Health benefits funds must be operated in accordance with the requirements of that Act.
131‑5 Private Health Insurance (Health Benefits Fund Policy) Rules
(1) *Health benefits funds (and some related matters) are also dealt with in the Private Health Insurance (Health Benefits Fund Policy) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Health Benefits Fund Policy) Rules are made by the Minister under section 333‑20.
(2) Before making Private Health Insurance (Health Benefits Fund Policy) Rules for the purposes of section 131‑15, the Minister must consult *APRA. However, a failure to consult APRA does not affect the validity of those Rules.
Note: This consultation requirement also applies to any repeal or amendment of such Rules: see subsection 33(3) of the Acts Interpretation Act 1901.
131‑10 Meaning of health benefits fund
A health benefits fund is a fund that:
(a) is established in the records of a private health insurer; and
(b) relates solely to:
(i) its *health insurance business, or a particular part of that business; or
(ii) its health insurance business, or a particular part of that business, and some or all of its *health‑related businesses, or particular parts of those businesses.
131‑15 Meaning of health‑related business
(1) Health‑related business is business that is any one or more of the following:
(a) a business of providing goods or services (or both) in order to manage or prevent diseases, injuries or conditions;
(b) a business of undertaking liability, by way of insurance, to indemnify people who are *ineligible for Medicare for costs associated with providing treatment, goods or services that:
(i) are provided to those people in Australia; and
(ii) are provided to manage or prevent diseases, injuries or conditions;
(c) a business of providing a financial service to assist people insured under *complying health insurance products to meet the costs associated with treatment, goods or services that are provided to manage or prevent diseases, injuries or conditions;
(d) any other business, or business included in a class of businesses, specified in the Private Health Insurance (Health Benefits Fund Policy) Rules for the purposes of this paragraph.
(2) Despite subsection (1), neither of the following is health‑related business:
(a) business that is *health insurance business; or
(b) any other business, or business included in a class of businesses, specified in the Private Health Insurance (Health Benefits Fund Policy) Rules for the purposes of this paragraph.
131‑20 Risk equalisation jurisdictions
(1) An area is a risk equalisation jurisdiction if the Private Health Insurance (Health Benefits Fund Policy) Rules so provide.
(2) The Private Health Insurance (Health Benefits Fund Policy) Rules may specify circumstances in which a private health insurer may (despite subsection 23(2) of the Private Health Insurance (Prudential Supervision) Act 2015) have more than one *health benefits fund in respect of a particular *risk equalisation jurisdiction.
131‑25 Operation of health‑related businesses through health benefits funds
If a private health insurer has a *health benefits fund in respect of its *health insurance business and some or all of its *health‑related businesses, the insurer must comply with any requirements specified in the Private Health Insurance (Health Benefits Fund Policy) Rules relating to how the health‑related businesses are to be conducted.
Part 4‑5—Miscellaneous obligations of private health insurers
Division 157—Introduction
157‑1 What this Part is about
This Part imposes miscellaneous notification and other obligations on private health insurers.
157‑5 Private Health Insurance (Data Provision) Rules
Obligations of private health insurers are also dealt with in the Private Health Insurance (Data Provision) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Data Provision) Rules are made by the Minister under section 333‑20.
Division 169—Notification obligations
169‑10 Private health insurers to notify any changes to rules
(1) A private health insurer that proposes to change its *rules (other than a change to which section 66‑10 applies) must notify the Secretary of the Department of the proposed change:
(a) in the *approved form; and
(b) before the day on which the insurer proposes the change to take effect.
Note: See section 93‑25 for a private health insurer’s obligation to notify insured persons of changes to its rules.
(2) The Minister may, in writing, direct the insurer not to make the change if the Minister is satisfied that the change might or would result in a breach of the Act.
Note: Directions are reviewable under Part 6‑9.
(3) The Minister must give the Secretary and *APRA a copy of a direction under subsection (2).
Division 172—Other obligations
172‑5 Agreements with medical practitioners
Medical purchaser‑provider agreements
(1) If a private health insurer enters into an agreement with a *medical practitioner for the provision of treatment to persons insured by the insurer, the agreement must not limit the medical practitioner’s professional freedom, within the scope of accepted clinical practice, to identify and provide appropriate treatments.
Practitioner agreements
(2) If a hospital or day hospital facility enters into an agreement with a *medical practitioner, under which treatment is provided to persons insured by the insurer, the agreement must not limit the medical practitioner’s professional freedom, within the scope of accepted clinical practice, to identify and provide appropriate treatments.
Note: Medical practitioners may, in dealings with private health insurers, be able to take advantage of the collective bargaining provisions of Subdivision B of Division 2 of Part VII of the Competition and Consumer Act 2010.
172‑10 Private health insurers to give information to Secretary
(1) The Private Health Insurance (Data Provision) Rules may specify kinds of information, relating to treatment of persons insured under *complying health insurance products that are *referable to *health benefits funds, that private health insurers are to give to the Secretary of the Department.
(2) A private health insurer must, in accordance with the Private Health Insurance (Data Provision) Rules, give to the Secretary of the Department any information of that kind that the insurer receives from a *hospital.
172‑15 Restrictions on payment of pecuniary penalties etc.
A private health insurer must not:
(a) use its money, or permit the use of its money, for:
(i) the payment of a pecuniary penalty imposed on a *director or *officer of the insurer because of an offence under this Act; or
(ii) the payment of an amount that a director or officer of the insurer, or a person who has been such a director or officer, is liable to pay under Division 203; or
(b) reimburse:
(i) a director or officer of the insurer in respect of a pecuniary penalty imposed on the director or officer because of an offence under this Act; or
(ii) a director or officer of the insurer, or a person who has been such a director or officer, in respect of a liability imposed on the director under Division 203.
Chapter 5—Enforcement
Part 5‑1—Introduction
Division 180—Introduction
180‑1 What this Chapter is about
Private health insurers who do not comply with this Act may have action taken against them under this Chapter.
Note: The methods set out in this Chapter are not the only enforcement methods available (see for example Division 84).
Part 5‑2—General enforcement methods
Division 185—What this Part is about
185‑1 Introduction
This Part gives the Minister powers to enable him or her to find out whether a private health insurer is complying with its enforceable obligations and to encourage or compel an insurer to comply with those obligations.
The Minister can:
(a) set performance indicators for insurers; or
(b) seek explanations from insurers; or
(c) investigate insurers; or
(d) obtain enforceable undertakings from insurers; or
(e) direct insurers to do particular things; or
(f) seek remedies in the Federal Court; or
(g) revoke an insurer’s entitlement to offer tax rebates as premium reductions.
185‑5 Meaning of enforceable obligation
All of the following provisions are enforceable obligations:
(a) a provision of this Act;
(b) a provision of any Private Health Insurance Rules made under section 333‑20;
(c) a provision of the regulations;
(d) a direction given to a private health insurer under this Act;
(e) if the insurer is a *restricted access insurer—a provision included in the insurer’s constitution or *rules in order to comply with subsection 15(3) of the Private Health Insurance (Prudential Supervision) Act 2015.
Division 188—Performance indicators
188‑1 Performance indicators
(1) The Private Health Insurance (Complying Product) Rules may set out performance indicators to be used by the Minister in monitoring private health insurers’ compliance with the principle of community rating in section 55‑5 and the community rating requirements in Division 66.
(2) The performance indicators are to be framed:
(a) to assist the Minister in detecting breaches of the principle of community rating in section 55‑5 or the community rating requirements in Division 66; and
(b) to alert the Minister to any practices of a private health insurer in relation to community rating that may require investigation; and
(c) to alert the Minister to any practices of one or more private health insurers in relation to community rating that may be contrary to government health policy and may require a regulatory response.
Division 191—Explanation of private health insurer’s operations
191‑1 Minister may seek an explanation from a private health insurer
(1) If, having regard to information available to the Minister or to any performance indicators under the Private Health Insurance (Complying Product) Rules, the Minister believes that a private health insurer may have contravened an *enforceable obligation, the Minister may write to the private health insurer:
(a) explaining the Minister’s concerns; and
(b) asking the insurer to explain its operations in relation to those concerns; and
(c) specifying the period within which the Minister requires the insurer’s response.
(2) The private health insurer must respond within the specified period, or any longer period that the Minister, in writing before the end of the specified period, allows.
(3) If the Minister refuses a request by the private health insurer for a longer period to respond, the Minister must state the Minister’s reasons for refusing.
Note: Refusals of requests for longer periods to respond are reviewable under Part 6‑9.
191‑5 Minister must respond to insurer’s explanation
The Minister must, after receiving an explanation from a private health insurer in response, inform the insurer in writing:
(a) whether the Minister is or is not satisfied with the explanation; and
(b) if the Minister is not satisfied with the explanation—what steps the Minister intends to take.
Division 194—Investigation of private health insurer’s operations
194‑1A Purposes for which powers may be exercised etc.
(1) The powers in this Division may only be exercised for the purposes of this Act.
(2) The powers in this Division cannot be exercised for the purposes of this Act, as it applies in relation to:
(a) levy imposed under the Private Health Insurance (Risk Equalisation Levy) Act 2003; or
(b) the Risk Equalisation Special Account.
194‑1 Minister may investigate a private health insurer
The Minister may, at any time and for any reason, begin an investigation of the operations of a private health insurer by doing either or both of the following:
(a) giving a notice under any one or more sections of this Division;
(b) authorising a person under section 194‑25.
194‑5 Notice to give information
(1) The Minister may give a written notice to a person who is or who has been an *officer, employee or agent of:
(a) a private health insurer; or
(b) an entity that was a private health insurer at any time in the year ending on the day on which the notice is given;
requiring the person to give the Minister or the person specified in the notice, within the period specified in the notice, information about the area of the insurer’s operations specified in the notice.
(2) The Minister may require the person to give the information orally or in writing.
(3) The Minister may require the person to give the information on oath or affirmation. For that purpose, the Minister or the person specified in the notice may administer an oath or affirmation.
(4) The person is not excused from giving information on the ground that giving the information might tend to incriminate the person or make the person liable to a penalty. However, the information, or anything obtained as a direct or indirect consequence of the information, is not admissible in evidence against the person in any proceedings, other than proceedings for an offence against section 137.1 or 137.2 of the Criminal Code.
194‑10 Notice to produce documents
(1) The Minister may give a written notice to a person who is or who has been an *officer, employee or agent of:
(a) a private health insurer; or
(b) an entity that was a private health insurer at any time in the year ending on the day on which the notice is given;
requiring the person to produce, at the time and place specified in the notice, records, books, accounts and other documents of the insurer that are in the person’s custody or under the person’s control and that relate to the area of the insurer’s operations specified in the notice.
(2) The person is not excused from producing a document on the ground that the production of the document might tend to incriminate the person or make the person liable to a penalty. However, the production of the document, or anything obtained as a direct or indirect consequence of the production, is not admissible in evidence against the person in any proceedings, other than proceedings for an offence against section 137.1 or 137.2 of the Criminal Code.
194‑15 Notice to give evidence
(1) The Minister may give a written notice to a person who is or who has been an *officer, employee or agent of:
(a) a private health insurer; or
(b) an entity that was a private health insurer at any time in the year ending on the day on which the notice is given;
requiring the person to attend, at the time and place specified in the notice, before the Minister or the person specified in the notice and give evidence relating to an area of the insurer’s operations specified in the notice.
(2) The Minister may require the person to give the evidence orally or in writing.
(3) The Minister may require the person to give the evidence on oath or affirmation. For that purpose, the Minister or the person specified in the notice may administer an oath or affirmation.
(4) The person is not excused from answering a question on the ground that the answer to the question might tend to incriminate the person or make the person liable to a penalty. However, the answer, or anything obtained as a direct or indirect consequence of the answer, is not admissible in evidence against the person in any proceedings, other than proceedings for an offence against section 137.1 or 137.2 of the Criminal Code.
194‑20 Offences in relation to investigation notices
(1) A person must not fail to comply with a requirement contained in a notice given to the person:
(a) under section 194‑5 (notice to give information); or
(b) under section 194‑10 (notice to produce documents); or
(c) under section 194‑15 (notice to give evidence).
Penalty: 10 penalty units.
(2) A person must not fail to be sworn or to make an affirmation when required to do so:
(a) under section 194‑5 (notice to give information); or
(b) under section 194‑15 (notice to give evidence).
Penalty: 10 penalty units.
(3) An offence under subsection (1) or (2) is an offence of strict liability.
Note: For strict liability, see section 6.1 of the Criminal Code.
194‑25 Authorisation to examine books and records etc.
(1) The Minister may, in writing, authorise a person to examine and report on the records, books, accounts and other documents of:
(a) a private health insurer; or
(b) an entity that was a private health insurer at any time in the year ending on the day on which the authorisation is given.
(2) A person authorised under subsection (1) must, at all reasonable times, have full and free access to any *premises at which the records, books, accounts and other documents are kept and may take extracts from, or copies of, the records, books, accounts and other documents.
194‑35 Minister must notify outcome of investigation
After completing an investigation under this Division of a private health insurer or former private health insurer, the Minister must inform the insurer in writing:
(a) whether the Minister is or is not satisfied with the performance of the insurer; and
(b) if the Minister is not satisfied with the performance of the insurer—what steps the Minister intends to take.
Division 197—Enforceable undertakings
197‑1 Minister may accept written undertakings given by a private health insurer
(1) The Minister may accept a written undertaking, given by a private health insurer at the Minister’s request, if the Minister considers that compliance with the undertaking will:
(a) be likely to improve the performance of the insurer in relation to one or more matters of a kind regulated by this Act; or
(b) if the Minister is satisfied that the insurer has contravened an *enforceable obligation—be likely to ensure that the insurer will cease to be in contravention of the enforceable obligation.
(3) The private health insurer may withdraw or vary the undertaking at any time with the consent of the acceptor of the undertaking.
197‑5 Enforcement of undertakings
(1) If the Minister considers that a private health insurer that gave an undertaking under this Division has contravened any of its terms, the Minister may apply to the Federal Court for an order under subsection (2).
(2) If the Federal Court is satisfied that the private health insurer has contravened a term of the undertaking, the court may make one or more of the following orders:
(a) an order directing the insurer to comply with the terms of the undertaking;
(b) if there is a contravention of an *enforceable obligation—any other order of a kind set out in Division 203 that the court considers appropriate.
Division 200—Ministerial directions
200‑1 Minister may give directions
(1) If, at any time and for any reason, the Minister considers that it will assist in the prevention of *improper discrimination to do so, the Minister may give a direction to a private health insurer requiring it:
(a) to modify its day‑to‑day operations in a particular respect; or
(b) to modify its *rules in a particular respect; or
(c) if the insurer is a *restricted access insurer—to modify the provisions included in its constitution or *rules in order to comply with subsection 15(3) of the Private Health Insurance (Prudential Supervision) Act 2015 in a particular respect.
Note: A decision to give a direction is reviewable under Part 6‑9.
(2) If, at any time and for any reason, the Minister considers that there appears to be a contravention of an *enforceable obligation involving *improper discrimination by a private health insurer, the Minister may give a direction to the insurer requiring it to address the contravention by:
(a) modifying its day‑to‑day operations; or
(b) modifying its *rules; or
(c) if the insurer is a *restricted access insurer—modifying the provisions included in its constitution or *rules in order to comply with subsection 15(3) of the Private Health Insurance (Prudential Supervision) Act 2015.
Note: A decision to give a direction is reviewable under Part 6‑9.
(3) A direction mentioned in subsection (1) or (2) may, if the Minister considers it proper to do so, include requirements with respect to the reconsideration by the private health insurer of an application or claim made to the insurer and dealt with by it before the direction takes effect.
(4) A private health insurer must, in reconsidering an application or claim in accordance with subsection (3), deal with the application or claim as if the direction had been in force at the time when the application or claim was first considered.
(5) A direction given under this section must be published on the Department’s website not later than 5 working days after the direction is given.
200‑5 Direction requirements
A direction given under this Division to a private health insurer:
(a) must be in writing; and
(b) must be signed by the Minister; and
(c) may be served on the insurer by serving a copy on the insurer’s *chief executive officer.
Division 203—Remedies in the Federal Court
203‑1 Minister may apply to the Federal Court
If the Minister is satisfied that a private health insurer has contravened an *enforceable obligation, the Minister may apply to the Federal Court for:
(a) a *declaration of contravention; and
(b) any one or more of the following orders:
(i) a pecuniary penalty order under section 203‑10;
(ii) a compensation order under section 203‑15;
(iii) an adverse publicity order under section 203‑20;
(iv) any other order that the Minister considers to be appropriate to redress the contravention.
203‑5 Declarations of contravention
(1) If the Federal Court is satisfied that a private health insurer has contravened an *enforceable obligation, it must make a declaration of contravention.
(2) The declaration must specify:
(a) the *enforceable obligation that was contravened; and
(b) the private health insurer that contravened the provision; and
(c) the conduct that constituted the contravention; and
(d) if the court is satisfied that an *officer of the private health insurer failed to take reasonable steps to prevent the insurer contravening the enforceable obligation—the officer.
(3) A *declaration of contravention is conclusive evidence of the matters mentioned in subsection (2).
203‑10 Pecuniary penalty order
(1) If the Federal Court has made a *declaration of contravention that specifies an *officer of a private health insurer (see paragraph 203‑5(2)(d)), the court may order the officer to pay the Commonwealth a pecuniary penalty of up to 1,000 penalty units.
(2) The court must not make an order under subsection (1) if it is satisfied that a court has ordered the *officer to pay damages in the nature of punitive damages in respect of:
(a) the contravention of the *enforceable obligation; or
(b) the officer’s failure to take reasonable steps to prevent the insurer contravening the enforceable obligation.
(3) The penalty is a civil debt payable to the Commonwealth. The Commonwealth may enforce the order as if it were an order made in civil proceedings against the *officer to recover a debt due by the officer. The debt arising from the order is taken to be a judgment debt.
203‑15 Compensation order
(1) If the Federal Court has made a *declaration of contravention, the court may order the private health insurer specified in the declaration to compensate an individual for any injury or loss suffered by the individual as a result of the contravention.
(2) The order must specify the amount of compensation.
(3) The order may be enforced as if it were a judgment of the court.
203‑20 Adverse publicity order
(1) If the Federal Court has made a *declaration of contravention, the court may make an order requiring the private health insurer specified in the declaration to do either or both of the following:
(a) disclose in a way, and to the person or persons, specified in the order, the information specified in the notice to correct or counter the effect of the contravention;
(b) publish, in the way specified in the order, an advertisement to correct or counter the effect of the contravention in the terms specified in, or determined in accordance with, the order.
(2) The order may be enforced as if it were a judgment of the court.
203‑25 Other order
(1) If the Federal Court has made a *declaration of contravention, the court may make any order that the applicant applies for.
(2) The order may be enforced as if it were a judgment of the court.
203‑30 Time limit for declarations and orders
Proceedings under this Division may be started no later than 6 years after the contravention.
203‑35 Civil evidence and procedure rules for declarations and orders
The Federal Court must apply the rules of evidence and procedure for civil matters in proceedings under this Division.
Note: The standard of proof in civil proceedings is the balance of probabilities (see section 140 of the Evidence Act 1995).
203‑40 Civil proceedings after criminal proceedings
The Federal Court must not make a pecuniary penalty order against an *officer of a private health insurer under section 203‑10 if the officer has been convicted of an offence constituted by conduct that is substantially the same as the conduct to which the court had regard in satisfying itself that the officer failed to take reasonable steps to prevent the insurer contravening the *enforceable obligation.
203‑45 Criminal proceedings during civil proceedings
(1) Proceedings for a pecuniary penalty order against an *officer of a private health insurer are stayed if:
(a) criminal proceedings are started or have already been started against the officer for an offence; and
(b) the offence is constituted by conduct that is substantially the same as the conduct to which the court had regard in satisfying itself that the officer failed to take reasonable steps to prevent the insurer contravening the *enforceable obligation.
(2) The proceedings for the order may be resumed if the *officer is not convicted of the offence. Otherwise, the proceedings for the order are dismissed.
203‑50 Criminal proceedings after civil proceedings
Criminal proceedings may be started against a person for conduct that is substantially the same as conduct constituting a contravention of an *enforceable obligation regardless of whether:
(a) a *declaration of contravention has been made that specifies the person; or
(b) an order has been made against the person under this Division.
203‑55 Evidence given in proceedings for penalty not admissible in criminal proceedings
Evidence of information given or evidence of production of documents by an *officer of a private health insurer is not admissible in criminal proceedings against the officer if:
(a) the officer previously gave the evidence or produced the documents in proceedings for a pecuniary penalty order against the officer under section 203‑10 (whether or not the order was made); and
(b) the conduct alleged to constitute the offence is substantially the same as the conduct to which the court had regard in satisfying itself that the officer failed to take reasonable steps to prevent the insurer contravening the *enforceable obligation.
However, this does not apply to a criminal proceeding in respect of the falsity of the evidence given by the officer in the proceedings for the pecuniary penalty order.
203‑60 Minister may require person to assist
(1) The Minister may, in writing, require a person to give all reasonable assistance in connection with:
(a) an application:
(i) for a *declaration of contravention in relation to a private health insurer; or
(ii) for a declaration of contravention that specifies an *officer of a private health insurer; or
(iii) for a pecuniary penalty order under section 203‑10 in relation to an officer of a private health insurer; or
(b) criminal proceedings against a private health insurer, or an officer of a private health insurer, for an offence against this Act.
The person must comply with the request.
Penalty: 5 penalty units.
(3) The Minister must not require the person to assist in connection with an application for a declaration or order unless:
(a) it appears to the Minister that someone other than the person required to assist may have contravened an *enforceable obligation; and
(b) the Minister suspects or believes that the person required to assist can give information relevant to the application.
(4) The Minister must not require the person to assist in connection with criminal proceedings unless:
(a) it appears to the Minister that the person required to assist is unlikely to be a defendant in the proceedings; and
(b) the person required to assist is an employee or agent (including a banker or auditor) of the private health insurer concerned.
(5) The Minister may require the person to assist regardless of whether:
(a) an application for the declaration or order has actually been made; or
(b) criminal proceedings for the offence have actually begun.
(6) The person cannot be required to assist if the person is or has been a lawyer for:
(a) in an application for a declaration or order—the person suspected of the contravention; or
(b) in criminal proceedings—a defendant or likely defendant in the proceedings.
(7) The Federal Court may order the person to comply with the requirement in a specified way. Only the Minister may apply to the court for an order under this subsection.
203‑65 Relief from liability for contravening an enforceable obligation
(1) If, in proceedings brought against a person under this Division, it appears to the Federal Court that:
(a) the person has, or may have:
(i) contravened an *enforceable obligation; or
(ii) if the person is an *officer of a private health insurer—failed to take reasonable steps to prevent the insurer from contravening an enforceable obligation; but
(b) the person has acted honestly and, having regard to all the circumstances of the case, the person ought fairly to be excused for the contravention;
the court may relieve the person either wholly or partly from a liability to which the person would otherwise be subject, or that might otherwise be imposed on the person, because of the contravention.
(2) A person who thinks that proceedings will or may be begun against the person under this Division may apply to the Federal Court for relief.
(3) On an application under subsection (2), the court may grant relief under subsection (1) as if the proceedings had been begun in the court.
(4) For the purposes of subsection (1) as applying for the purposes of a case tried by a judge with a jury:
(a) a reference in that subsection to the court is a reference to the judge; and
(b) the relief that may be granted includes withdrawing the case in whole or in part from the jury and directing judgment to be entered for the defendant on such terms as to costs as the judge thinks appropriate.
203‑70 Powers of Federal Court
A provision of this Act conferring a power on the Federal Court does not affect any other power of the court conferred by this Act or otherwise.
Division 206—Revoking entitlement to offer rebate as a premium reduction
206‑1 Revocation of status of participating insurer
(1) If a *participating insurer:
(b) has failed to comply with a condition specified in the Private Health Insurance (Incentives) Rules as a condition of participation in the *premiums reduction scheme; or
(c) refuses or fails to comply with:
(i) a direction given by the Minister under section 200‑1; or
(ii) the principle of community rating in section 55‑5;
the Minister may, by notice given to the insurer, revoke the insurer’s status as a participating insurer.
(2) Upon the giving of the notice, the insurer ceases to be a *participating insurer.
Note: Decisions to revoke an insurer’s status as a participating insurer are reviewable under Part 6‑9.
Chapter 6—Administration
Part 6‑1—Introduction
Division 230—Introduction
230‑1 What this Chapter is about
This Chapter:
(c) deals with some general administrative matters relating to the premiums reduction scheme in Part 2‑2;
(e) deals with administration and collection of private health insurance levies;
(f) provides for the Private Health Insurance Risk Equalisation Special Account;
(g) protects information obtained for the purposes of this Act and sets out the circumstances in which such information may be used;
(h) provides for review by the Administrative Appeals Tribunal of certain decisions made under this Act;
(i) provides for miscellaneous other matters such as delegations, the approval of forms and the making of Private Health Insurance Rules and regulations.
Part 6‑4—Administration of premiums reduction scheme
Division 276—Introduction
276‑1 What this Part is about
Part 2‑2 provides for a premiums reduction scheme. This Part provides:
(a) for private health insurers to be reimbursed for premiums that were reduced under the premiums reduction scheme in Division 23; and
(b) for the Chief Executive Medicare to supervise that reimbursement and related matters; and
(c) for recovery of amounts paid in error; and
(d) for various other related administrative matters in relation to the scheme.
Division 279—Reimbursement of participating insurers and powers of Chief Executive Medicare
Subdivision 279‑A—Reimbursement of private health insurers for premiums reduced under scheme
279‑1 Participating insurers may claim reimbursement
A private health insurer may claim reimbursement from the Chief Executive Medicare in accordance with section 279‑10 for each month during which it is a *participating insurer.
279‑5 Participating insurers
(1) A private health insurer may apply to the Minister, in the *approved form, to become a *participating insurer for the purposes of this Part.
(2) If the Minister approves the application, the private health insurer becomes a *participating insurer.
(3) The Minister must approve the application, unless:
(a) the insurer’s status as a *participating insurer has previously been revoked under subsection 206‑1(1); and
(b) the Minister is satisfied that the insurer is continuing, or will continue, to fail to comply with a provision or condition mentioned in that subsection.
Note: Rejections of applications are reviewable under Part 6‑9.
(4) The Minister must notify the applicant, within 28 days after the date of the decision, whether the application has been approved or rejected.
(5) If the application is rejected, the Minister must include his or her reasons for rejecting the application in the notice.
279‑10 Requirements for claims
(1) A claim by a private health insurer in respect of a month must be made to the Chief Executive Medicare, in the *approved form, on or before the seventh day of the following month.
(2) If the Chief Executive Medicare decides the claim is correct, the Chief Executive Medicare must pay the insurer, in accordance with section 279‑15, the amount payable under that section in respect of the month to which the claim relates.
279‑15 Amounts payable to the private health insurer
(1) Subject to subsection (2), the amount payable to the private health insurer in respect of the month is the sum of the amounts by which premiums in respect of that month under the *complying health insurance policies issued by the private health insurer were reduced because of the operation of Division 23.
(2) The amount must be paid to the private health insurer within the period of 15 days starting on the first day of the following month.
(3) The amount must be paid in the way determined, in writing, by the Chief Executive Medicare.
279‑20 Notifying private health insurers if amount is not payable
(1) If the Chief Executive Medicare considers that a claim is incorrect, the Chief Executive Medicare may either refuse the claim or pay only such part of the claim as he or she is satisfied is correct.
(2) The Chief Executive Medicare must notify a private health insurer if the Chief Executive Medicare makes a decision mentioned in subsection (1).
(3) A notice under subsection (2) must include reasons for the decision.
(4) The Chief Executive Medicare is taken, for the purposes of this Part, to have decided that a claim is correct if the Chief Executive Medicare does not give notice of his or her decision that the claim is incorrect on or before the day under subsection 279‑15(2) on or before which, if the claim were correct, it would have been required to have been paid.
279‑25 Additional payment if insurer claims less than entitlement
(1) This section applies to a private health insurer in respect of a month if:
(a) the private health insurer is a *participating insurer in respect of the month; and
(b) the private health insurer made a claim in respect of the month under section 279‑1; and
(c) the amount claimed by the private health insurer was less than the sum of the amounts by which premiums in respect of the month under the *complying health insurance policies issued by the private health insurer were reduced because of the operation of this Division.
(2) The private health insurer may apply to the Chief Executive Medicare for payment of an amount (the additional amount) not exceeding the difference between:
(a) the sum of the amounts by which premiums in respect of the month under the *complying health insurance policies issued by the private health insurer were reduced because of the operation of this Division; and
(b) the amount already paid to the private health insurer under section 279‑1 in respect of the month.
(3) An application under subsection (2) may relate to more than one month.
279‑30 Additional payment if insurer makes a late claim
(1) This section applies to a private health insurer in respect of a month if:
(a) the private health insurer did not make a claim in respect of the month on or before the seventh day of the following month; and
(b) premiums in respect of the month under the *complying health insurance policies issued by the private health insurer were reduced because of the operation of this Division.
(2) The private health insurer may apply to the Chief Executive Medicare for payment of an amount (the additional amount) not exceeding the sum of the amounts by which premiums in respect of the month under the *complying health insurance policies issued by the private health insurer were reduced because of the operation of Division 23.
(3) An application under subsection (2) may relate to more than one month.
279‑35 Content and timing of application
(1) An application by a private health insurer under section 279‑25 or 279‑30 for payment of an additional amount must be in the *approved form.
(2) The application must be made:
(a) if the application relates to only one month—within 3 years of the end of that month; or
(b) if the application relates to more than one month—within 3 years of the end of the first of those months.
279‑40 Decision on application
(1) If a private health insurer makes an application under section 279‑25 or 279‑30 for payment of an additional amount, the Chief Executive Medicare must pay the additional amount sought if the Chief Executive Medicare is satisfied:
(a) that the additional amount sought is correct; and
(b) that it would be reasonable to grant the application.
(2) The Chief Executive Medicare may refuse the application, or decide to pay only part of the additional amount sought, if the Chief Executive Medicare is satisfied:
(a) that the additional amount sought is incorrect; or
(b) that it would not be reasonable to grant the application.
(3) The Chief Executive Medicare must notify the private health insurer of the Chief Executive Medicare’s decision on the application.
(4) A notice under subsection (3) must include reasons for the decision.
(5) The Chief Executive Medicare is taken, for the purposes of this Part, to have decided that:
(a) the additional amount sought is correct; and
(b) that it would be reasonable to grant the application;
if the Chief Executive Medicare does not give notice of his or her decision that the additional amount sought is incorrect, or that it would not be reasonable to grant the application, within the period of 3 months after the application was received by the Chief Executive Medicare.
(6) If the Chief Executive Medicare is taken to have made a decision under subsection (5) in respect of a private health insurer, the Chief Executive Medicare is taken to have given notice of that decision to the private health insurer.
279‑45 Reconsideration of decisions
(1) A private health insurer that has been given a notice under subsection 279‑20(2) or 279‑40(3) may request the Chief Executive Medicare to reconsider the decision.
(2) The request must:
(a) set out the reasons for the request; and
(b) be made within the period of 28 days after the day on which the Chief Executive Medicare gave the notice.
(3) As soon as practicable after receiving the request, the Chief Executive Medicare must reconsider the decision and:
(a) affirm it; or
(b) vary it; or
(c) revoke it and make a fresh decision.
Note: Decisions on reconsideration are reviewable under Part 6‑9.
(4) If the Chief Executive Medicare varies the decision or revokes the decision and makes a fresh decision, the decision as varied, or the fresh decision, as the case may be, has effect according to its terms and is taken always to have had that effect from the time when the original decision was made.
(5) The Chief Executive Medicare must notify the private health insurer stating the Chief Executive Medicare’s decision on the reconsideration together with a statement of his or her reasons for the decision.
(6) The Chief Executive Medicare is taken, for the purposes of this Part, to have revoked the decision if the Chief Executive Medicare does not notify the private health insurer of his or her decision on the reconsideration within 28 days after receiving the request.
Subdivision 279‑B—Powers of Chief Executive Medicare in relation to participating insurers
279‑50 Audits by Chief Executive Medicare
(1) The Chief Executive Medicare may, at any time, audit the accounts and records of a private health insurer that is, or has been, a *participating insurer.
(2) An audit under subsection (1) must relate only to the accounts and records of the private health insurer to the extent that they deal with:
(a) participation by persons in the *premiums reduction scheme; or
(b) reductions of premium payable under *complying health insurance policies under the premiums reduction scheme; or
(c) receipt of money from the Chief Executive Medicare under this Division.
(3) The Chief Executive Medicare must not carry out an audit unless he or she has given notice to the private health insurer concerned stating that an audit is to be carried out.
(4) The private health insurer must ensure that the Chief Executive Medicare has full and free access to all accounts, records, documents and papers of the private health insurer that are relevant to the audit.
(5) The person carrying out the audit may make copies of, or take extracts from, such accounts, records, documents or papers for use in the audit.
(6) Without limiting the powers of the Chief Executive Medicare under this section, the Chief Executive Medicare may, by notice given to a private health insurer, require the insurer to give to the Chief Executive Medicare, within a period specified in the notice beginning at the end of a financial year, a certificate in writing by a registered company auditor as to the correctness of the accounts and records of the insurer for that year to the extent that those accounts and records deal with matters mentioned in paragraphs (2)(a), (b) and (c).
279‑55 Chief Executive Medicare may require production of applications
(1) The Chief Executive Medicare may, by notice given to a private health insurer, require the private health insurer:
(a) to produce to the Chief Executive Medicare, within the period and in the manner specified in the notice, applications retained under section 23‑45; or
(b) to make copies of any such applications and give them to the Chief Executive Medicare within the period and in the manner specified in the notice.
(2) A period specified under subsection (1) must not be less than one month.
(3) A private health insurer is entitled to be paid by the Chief Executive Medicare reasonable compensation for complying with paragraph (1)(b).
Division 282—Recovery of amounts and other matters
Subdivision 282‑A—When and how payments can be recovered
282‑1 Recovery of payments
(1) The following amounts are recoverable as debts due to the Commonwealth:
(d) so much of a payment made under section 279‑15 or 279‑40 as relates to a *complying health insurance policy that covers a person who was:
(i) a *participant in the premiums reduction scheme for the financial year concerned in respect of the policy; and
(ii) not eligible to participate in that scheme in respect of that policy;
(e) so much of a payment made under section 279‑15 or 279‑40 as relates to a premium for which a reduction was not allowable under section 23‑1;
(f) 150% of so much of a payment made under section 279‑15 or 279‑40 as:
(i) is not reflected in reductions in premiums payable under complying health insurance policies issued by the private health insurer concerned; or
(ii) relates to a person whose application under subsection 23‑15(1) has not been retained by the private health insurer as required by section 23‑45; or
(iii) relates to a person whose application under subsection 23‑15(1) has been so retained, but has not been produced to the Chief Executive Medicare by the private health insurer in accordance with a requirement made by the Chief Executive Medicare under section 279‑55;
(g) so much of a payment purportedly made under section 279‑15 or 279‑40 as was not payable under that section;
(h) interest payable under subsection 282‑5(2).
(1A) However, an amount is not recoverable under paragraph (1)(d), (e), (f) or (g) if the situation giving rise to the amount did not occur due to the fault of the private health insurer.
(2) The amounts are recoverable from:
(b) if paragraph (1)(d), (e), (f) or (g) applies—the private health insurer to which the payment concerned was made; or
(c) if paragraph (1)(h) applies:
(i) if the payment was made to a private health insurer—that insurer; or
(ii) if the payment was made to an individual—the individual or his or her estate.
(3) An amount recoverable under subsection (1) is recoverable whether or not any person has been convicted of an offence relating to the payment.
282‑5 Interest on amounts recoverable
(1) If the Chief Executive Medicare has served, on an individual from whom an amount is recoverable or the legal personal representative of such an individual, or on a private health insurer from which an amount is recoverable, under subsection 282‑1(1) a notice claiming an amount as a debt due to the Commonwealth and:
(a) an arrangement for the repayment of the amount has been entered into between the Chief Executive Medicare and the individual or the individual’s legal personal representative, or the private health insurer, as the case may be, within the period referred to in subsection (3), and there has been a default in payment of an amount required to be paid under the arrangement; or
(b) at the end of the period such an arrangement has not been entered into and all or part of the amount remains unpaid;
then, from and including the day after the end of the period, interest becomes payable on so much of the amount as from time to time remains unpaid.
(2) Interest is payable:
(a) at the rate of 15% per annum; or
(b) if a lower rate is specified in the Private Health Insurance (Incentives) Rules for the purposes of this paragraph—that rate.
(3) The period for entering into an arrangement under paragraph (1)(a) is the period of 3 months following the service of the notice under subsection (1), or such longer period as the Chief Executive Medicare allows.
(4) Despite subsection (1), in any proceedings instituted by the Commonwealth for the recovery of an amount due under paragraph 282‑1(1)(h), the court may order that the interest payable under that paragraph is, and is taken to have been, so payable from and including a day later than the day referred to in subsection (1).
282‑10 Chief Executive Medicare may set off debts against amounts payable
(1) Despite any other provision of Part 2‑2 or this Part, if:
(a) except for this section, an amount would be payable by the Chief Executive Medicare to a person or his or her estate, or to a private health insurer, under Part 2‑2 or this Part; and
(b) an amount is recoverable under section 282‑1 by the Commonwealth from the person or his or her estate, or from the insurer, as the case may be;
the Chief Executive Medicare may set off the whole or a part of the amount referred to in paragraph (b) against the amount referred to in paragraph (a).
(2) If the Chief Executive Medicare decides to make such a set‑off in respect of a person or his or her estate, the Chief Executive Medicare must serve on the person or his or her legal personal representative or the legal personal representative of his or her estate a notice of the decision.
(3) If the Chief Executive Medicare makes such a set‑off:
(a) the Chief Executive Medicare is liable to pay to the person or his or her estate, or to the insurer, only the amount remaining after the set‑off; and
(b) the amount referred to in paragraph (1)(b) is reduced by the amount set off.
282‑15 Reconsideration of certain decisions under this Division
(1) A person (the applicant) may apply to the Chief Executive Medicare for the Chief Executive Medicare to reconsider the following decisions:
(a) a decision that an amount is recoverable as a debt due to the Commonwealth under paragraph 282‑1(1)(h) in respect of a payment made to an individual;
(b) a decision under subsection 282‑10(1) to set off a debt against an amount otherwise payable to a person (other than a private health insurer) or his or her estate.
(2) The application must:
(a) be in writing; and
(b) set out the reasons for the application.
(3) The application must be made within:
(a) 28 days after the day on which the applicant is notified of the decision; or
(b) if, either before or after the end of that period of 28 days, the Chief Executive Medicare extends the period within which the application may be made—the extended period for making the application.
(4) Upon receiving such an application, the Chief Executive Medicare must:
(a) reconsider the decision; and
(b) either affirm or revoke the decision.
Note: Decisions affirming an original decision of the Chief Executive Medicare are reviewable under Part 6‑9.
(5) If the Chief Executive Medicare revokes the decision, the revocation is taken to be a decision:
(a) in the case of a decision mentioned in paragraph (1)(a)—to waive the debt; or
(b) in the case of a decision mentioned in paragraph (1)(b)—not to set off a debt against an otherwise payable amount.
(6) The Chief Executive Medicare must give the applicant a notice stating his or her decision on the reconsideration together with a statement of his or her reasons for the decision.
(7) The Chief Executive Medicare must make his or her decision on the reconsideration within 28 days after the day on which he or she received the application for the reconsideration.
(8) The Chief Executive Medicare is taken, for the purposes of this Subdivision, to have made a decision confirming the original decision if the Chief Executive Medicare has not told the applicant of his or her decision on the reconsideration before the end of the period of 28 days.
Subdivision 282‑AA—Recovery of certain amounts by Commissioner of Taxation
282‑16 Administration of this Subdivision by Commissioner of Taxation
The Commissioner of Taxation has the general administration of:
(a) this Subdivision; and
(b) any other provision of this Act to the extent that it relates to this Subdivision.
282‑17 Subdivision operates in addition to Subdivision 282‑A
(1) This Subdivision:
(a) operates in addition to Subdivision 282‑A; and
(b) does not limit the operation of that Subdivision.
(2) Subdivision 282‑A does not limit the operation of this Subdivision.
No double recovery
(3) Despite subsections (1) and (2):
(a) an amount is not recoverable under section 282‑1 to the extent that it has already been recovered in accordance with section 282‑18; and
(b) an amount is not recoverable under section 282‑18 to the extent that it has already been recovered in accordance with section 282‑1.
Note: This section means that an amount that is recoverable under both paragraph 282‑1(1)(e) and section 282‑18 is recoverable from the private health insurer in accordance with section 282‑1 or from the participant in accordance with section 282‑18.
282‑18 Liability for excess private health insurance premium reduction or refund
(1) This section applies if the amount of a premium payable during a financial year under a *complying health insurance policy is reduced because of the operation or purported operation of Division 23.
(2) Divide the total of the reduction by the number of persons who are *PHIIBs in respect of the premium.
(3) If the amount worked out under subsection (2) exceeds the *share of the PHII benefit of a person who is a *PHIIB in respect of the premium, that person is liable to pay the amount of that excess to the Commonwealth.
(4) If subsection (3) applies, the Commissioner of Taxation must give the person a notice stating that the person is liable to pay the amount of that excess to the Commonwealth.
(5) A notice given to a person under subsection (4) may be contained in a notice of assessment under the Income Tax Assessment Act 1936.
(6) An amount that a person is liable to pay under subsection (3) is due and payable at the same time as the income tax the person must pay for the financial year is due and payable under section 5‑5 of the Income Tax Assessment Act 1997. For the purposes of determining that time, assume that the person must pay income tax for the financial year and that the Commissioner of Taxation makes an assessment of the income tax.
Note: The liability is a tax‑related liability: see Part 4‑15 in Schedule 1 to the Taxation Administration Act 1953 for collection and recovery provisions.
(7) If the person is dissatisfied with the notice under subsection (4), he or she may object against it in the manner set out in Part IVC of the Taxation Administration Act 1953.
Reallocation of liability between spouses
(8) Subsection (10) applies if:
(a) a person (the first person) is a *PHIIB in respect of the premium; and
(b) the first person is, on the last day of the financial year, married (within the meaning of the A New Tax System (Medicare Levy Surcharge—Fringe Benefits) Act 1999; and
(c) the person to whom the first person is married is also a PHIIB in respect of the premium; and
(d) either:
(i) the first person has made a choice under section 61‑215 of the Income Tax Assessment Act 1997 in relation to the *income year corresponding to the financial year mentioned in subsection (1); or
(ii) the requirement in subsection (9) is satisfied.
(9) The requirement in this subsection is satisfied if:
(a) during an *income year (the lodgement year), the first person lodges his or her income tax return for the income year (the return year) corresponding to the financial year mentioned in subsection (1); and
(b) the person to whom the first person is married does not lodge his or her income tax return for the return year before the end of the lodgement year (whether or not he or she is required to lodge such a return).
(10) If this subsection applies:
(a) the amount (if any) that the person to whom the first person is married is liable to pay under subsection (3) in respect of the premium is reduced to nil; and
(b) the first person’s liability under subsection (3) is increased by that amount.
282‑19 When general interest charge payable
(1) If:
(a) a person is liable under section 282‑18 to pay an amount; and
(b) the whole or a part of the amount remains unpaid after the time by which the amount is due to be paid;
the person is liable to pay *general interest charge on the unpaid amount.
(2) A person who is liable under this section to pay *general interest charge on an unpaid amount is liable to pay the charge for each day in the period that:
(a) started at the beginning of the day by which the unpaid amount was due to be paid; and
(b) finishes at the end of the last day at the end of which any of the following remains unpaid:
(i) the unpaid amount;
(ii) general interest charge on any of the unpaid amount.
Subdivision 282‑B—Miscellaneous
282‑20 Notification requirements—private health insurers
(1) The Chief Executive Medicare may, by notice given to a private health insurer, require the insurer, within the period specified in the notice, to provide information specified in the notice about a person who:
(a) is covered at any time during a financial year specified in the notice by a *complying health insurance policy issued by the insurer; or
(b) paid premiums under such a policy.
(2) The information must be given in the *approved form.
(3) A private health insurer commits an offence if:
(a) the insurer is required by a notice under subsection (1) to provide information within a specified period about a person or matter; and
(b) the insurer fails to comply with the requirement.
Penalty: 20 penalty units.
Note: The obligation to provide information in response to a notice under subsection (1) is a continuing obligation and a private health insurer commits an offence for each day, after the period specified in the notice, until the information is provided (see section 4K of the Crimes Act 1914).
(4) Strict liability applies to subsection (3).
Note: For strict liability, see section 6.1 of the Criminal Code.
282‑25 Use etc. of information relating to another person
A person commits an offence if:
(a) the person uses, makes a record of, or discloses or communicates to any person, any information that relates to the affairs of another person and was acquired under or for the purposes of Part 2‑2, this Part or paragraph 323‑5(c); and
(b) the use, making of the record, disclosure or communication was not carried out in the performance of a function or obligation, or the exercise of a power, under Part 2‑2, this Part or paragraph 323‑5(c).
Penalty: Imprisonment for 1 year.
282‑30 Information to be provided to the Commissioner of Taxation
(1) The Chief Executive Medicare must, within 120 days after the end of each financial year, give to the Commissioner of Taxation the information that the Commissioner of Taxation, by legislative instrument, determines.
(2) A determination under subsection (1) must not require the Chief Executive Medicare to give:
(a) the *tax file number of any person; or
(b) information about the physical, psychological or emotional health of any person.
282‑35 Delegation
The Chief Executive Medicare may, by writing, delegate all or any of his or her powers under Part 2‑2 or this Part to a Departmental employee (within the meaning of the Human Services (Medicare) Act 1973).
Note: The Minister may also delegate his or her powers under Part 2‑2 or this Part (see section 333‑5).
282‑40 Appropriation
The Consolidated Revenue Fund is appropriated for the purpose of making payments under Part 2‑2 and this Part.
Part 6‑6—Private health insurance levies
Division 304—Introduction
304‑1 What this Part is about
Each private health insurance levy is imposed under a levy Act. This Part deals with collection of the levies and other matters relating to their administration.
304‑5 Private Health Insurance (Levy Administration) Rules
The collection of *private health insurance levies and other matters relating to administration of the levies are also dealt with in the Private Health Insurance (Levy Administration) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Levy Administration) Rules are made by the Minister under section 333‑20.
304‑10 Meaning of private health insurance levy
Each of the following levies is a private health insurance levy:
(b) levy imposed under the Private Health Insurance (Complaints Levy) Act 1995 (complaints levy);
(d) levy imposed under the Private Health Insurance (Risk Equalisation Levy) Act 2003 (risk equalisation levy);
(e) levy imposed under the Private Health Insurance (National Joint Replacement Register Levy) Act 2009 (national joint replacement register levy).
Note: Private health insurers are also liable to pay levies imposed by the Private Health Insurance Supervisory Levy Imposition Act 2015 and the Private Health Insurance (Collapsed Insurer Levy) Act 2003. This Part does not apply to those levies. The collection of those levies is dealt with in the Financial Institutions Supervisory Levies Collection Act 1998.
Division 307—Collection and recovery of private health insurance levies
307‑1 When private health insurance levy must be paid
(1) A *private health insurance levy that is imposed on a particular day (the imposition day) becomes due and payable on the day specified as the payment day for that imposition day in:
(a) a determination made by the Minister, by legislative instrument, if the levy is:
(iii) *complaints levy imposed on a supplementary complaints levy administration day (within the meaning of the Private Health Insurance (Complaints Levy) Act 1995; or
(iv) *risk equalisation levy imposed on a supplementary risk equalisation levy day (within the meaning of the Private Health Insurance (Risk Equalisation Levy) Act 2003; or
(v) *national joint replacement register levy imposed on a supplementary national joint replacement register levy day (within the meaning of the Private Health Insurance (National Joint Replacement Register Levy) Act 2009); and
(b) otherwise—the Private Health Insurance (Levy Administration) Rules.
(2) The Minister must obtain, and take into account, advice from *APRA in relation to the day that is to be specified as the payment day in a determination made under subparagraph (1)(a)(iv).
307‑5 Late payment penalty
(1) If a *private health insurance levy remains wholly or partly unpaid by a person after it becomes due and payable, the person is liable to pay a late payment penalty under this section.
(2) The *late payment penalty is calculated:
(a) at the rate specified in the Private Health Insurance (Levy Administration) Rules (which must not be higher than 15%); and
(b) on the unpaid amount of the levy; and
(c) for the period:
(i) starting when the levy becomes due and payable; and
(ii) ending when the levy, and the penalty payable under this section, have been paid in full.
307‑10 Payment of levy and late payment penalty
(1) The following must be paid to the Commonwealth:
(a) a *complaints levy;
(b) a *late payment penalty in respect of a complaints levy;
(c) a *national joint replacement register levy;
(d) a late payment penalty in respect of a national joint replacement register levy.
(2) The following must be paid to *APRA, on behalf of the Commonwealth:
(a) *risk equalisation levy;
(b) *late payment penalty in respect of risk equalisation levy.
Note: These amounts are to be credited to the Risk Equalisation Special Account: see section 318‑5.
307‑15 Recovery of levy and late payment penalty
(1) A *private health insurance levy that is due and payable is a debt due to the Commonwealth.
(2) A *late payment penalty is a debt due to the Commonwealth.
(3) An amount referred to in subsection (1) or (2) may be recovered as a debt by action in a court of competent jurisdiction by:
(a) the Commonwealth, in respect of a debt payable to the Commonwealth under subsection 307‑10(1); or
(b) *APRA (as agent of the Commonwealth), in respect of a debt payable under subsection 307‑10(2).
307‑20 Waiver of late payment penalty
(1) The Minister may waive the whole or part of an amount of *late payment penalty in respect of an unpaid amount of:
(a) *complaints levy; or
(b) *national joint replacement register levy;
if the Minister considers that there are good reasons for doing so.
(2) *APRA may waive the whole or part of an amount of *late payment penalty in respect of an unpaid amount of *risk equalisation levy if APRA considers that there are good reasons for doing so.
307‑30 Other matters
The Private Health Insurance (Levy Administration) Rules may, in relation to *private health insurance levy or *late payment penalty, provide for, or for matters relating to, any or all of the following:
(a) methods for payment;
(b) extending the time for payment;
(c) refunding or otherwise applying overpayments.
Division 310—Returns, requesting information and keeping records: private health insurers
310‑1 Returns relating to complaints levy
(1) A private health insurer must lodge a return for each day that, under the Private Health Insurance (Complaints Levy) Act 1995, is a census day.
(3) The return must:
(a) be in the *approved form; and
(b) be lodged with the Secretary of the Department within 28 days after the census day.
(4) A private health insurer commits an offence if the insurer fails to lodge the return.
Penalty: 60 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
310‑5 Insurer must keep records
(1) A private health insurer must keep all records that are relevant to either or both of following:
(a) whether the insurer is liable to pay a *private health insurance levy;
(b) the amount of the private health insurance levy that the insurer is liable to pay.
(2) The records must be kept in:
(a) an electronic form; or
(b) another form approved by:
(i) the Secretary of the Department, if the records relate to *complaints levy; or
(ii) *APRA, if the records relate to *risk equalisation levy.
(3) The records must be retained for a period of 7 years (or a shorter period allowed by the Private Health Insurance (Levy Administration) Rules) starting on the later of:
(a) the day on which the records were created; or
(b) 1 July 2004.
(4) A private health insurer commits an offence if the insurer fails to:
(a) keep the records; or
(b) keep the records in the form required by or under subsection (2); or
(c) retain the records for the period required by or under subsection (3).
Penalty: 60 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
(6) Nothing in this section is to be taken to have required an insurer to do an act or thing before the day on which this Act commences.
310‑10 Power to request information from insurer
(1) *APRA may, if it believes on reasonable grounds that a private health insurer is capable of giving information that is relevant to:
(a) whether the insurer is liable to pay *risk equalisation levy; or
(b) the amount of risk equalisation levy that the insurer is liable to pay;
request the insurer to give APRA the information or records that are specified in the request, before the end of the period specified in the request.
(2) The Secretary of the Department may, if he or she believes on reasonable grounds that a private health insurer is capable of giving information that is relevant to:
(a) whether the insurer is liable to pay *complaints levy; or
(b) the amount of complaints levy that the insurer is liable to pay;
request the insurer to give him or her the information or records that are specified in the request, before the end of the period specified in the request.
(3) A request under subsection (1) or (2):
(a) must be served on the *chief executive officer of the insurer; and
(b) may require the information to be verified by statutory declaration; and
(c) must specify the manner in which the information must be given; and
(d) must contain a statement to the effect that a failure to comply with the request is an offence.
(4) A private health insurer commits an offence if the insurer fails to comply with a request under subsection (1) or (2).
Penalty: 60 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
Division 313—Power to enter premises and search for documents related to complaints levy
313‑1 Authorised officer may enter premises with consent
(1) A person (an authorised officer) who is authorised in writing by the Minister for this purpose may enter any *premises for the purpose of exercising *search powers in relation to *levy‑related documents if:
(c) the *occupier of the premises consents to the entry; and
(d) the officer shows the occupier his or her identity card.
(2) A levy‑related document is a document (including a copy of a document) that contains information relevant to:
(a) whether a private health insurer is liable to pay *complaints levy; or
(b) the amount of complaints levy that the insurer is liable to pay.
(3) Before obtaining the consent of the *occupier, the *authorised officer must inform the occupier that he or she may refuse consent.
(4) An entry by an *authorised officer with the consent of the *occupier is not lawful if the consent of the occupier is not voluntary.
(5) The *authorised officer must leave the *premises if the *occupier asks the officer to do so.
313‑5 Authorised officer may enter premises under warrant
(1) If an *authorised officer has reason to believe that there are *levy‑related documents on particular *premises, the officer may apply to a magistrate for a warrant authorising the officer to enter the premises for the purpose of exercising *search powers in relation to the documents.
(2) If the magistrate is satisfied by information on oath or affirmation that there are reasonable grounds for believing that there are *levy‑related documents on the *premises, the magistrate may issue a warrant.
(3) The warrant must:
(a) authorise one or more *authorised officers to enter the *premises for the purpose of exercising *search powers in relation to *levy‑related documents; and
(b) state whether the entry is authorised at any time of the day or night or during specified hours of the day or night; and
(c) authorise the officers to use such assistance and force as is necessary and reasonable to enter the premises for the purpose of exercising search powers in relation to levy‑related documents.
(4) The *authorised officers do not have to be named in the warrant.
313‑10 Announcement before entry
An *authorised officer executing a warrant under section 313‑5 in respect of *premises must, before entering the premises under the warrant:
(a) announce that he or she is authorised to enter the premises; and
(b) before using assistance and force under the warrant to enter the premises—give any person on the premises an opportunity to allow the authorised officer to enter the premises without the use of assistance and force.
313‑15 Executing a warrant to enter premises
Circumstances in which this section applies
(1) This section applies if:
(a) a warrant under section 313‑5 is being executed by an *authorised officer in respect of *premises; and
(b) the *occupier of the premises is present.
Obligations of authorised officer executing a warrant
(2) The *authorised officer must:
(a) make a copy of the warrant available to the *occupier; and
(b) show the occupier the officer’s identity card; and
(c) inform the occupier of the occupier’s rights and responsibilities under subsections (3) to (6).
Persons entitled to observe execution of warrant
(3) The *occupier, or a person nominated by the occupier who is readily available, is entitled to observe the execution of the warrant.
(4) The right to observe the execution of the warrant ceases if the *occupier or the nominated person impedes that execution.
(5) Subsection (3) does not prevent the execution of the warrant in 2 or more areas of the *premises at the same time.
Occupier to provide reasonable facilities and assistance
(6) An *occupier commits an offence if the occupier fails to provide the *authorised officer and any person assisting that officer with all reasonable facilities and assistance for the effective exercise of their powers under the warrant.
Penalty: 60 penalty units.
313‑20 Identity cards
(1) For the purposes of this Division, the Secretary of the Department must issue an identity card to an *authorised officer in the *approved form. It must contain a recent photograph of the authorised officer.
(2) A person commits an offence if:
(a) the person has been issued with an identity card; and
(b) the person ceases to be an *authorised officer; and
(c) the person does not, as soon as it is practicable after so ceasing, return the identity card to the Secretary of the Department.
Penalty: 1 penalty unit.
(3) Strict liability applies to subsection (2).
Note: For strict liability, see section 6.1 of the Criminal Code.
(4) An *authorised officer must carry the identity card at all times when exercising powers or performing functions under this Division as an authorised officer.
Part 6‑7—Private Health Insurance Risk Equalisation Special Account
Division 318—Private Health Insurance Risk Equalisation Special Account
318‑1 Private Health Insurance Risk Equalisation Special Account
(1) The Private Health Insurance Risk Equalisation Special Account (the Risk Equalisation Special Account) is established by this section.
(2) The *Risk Equalisation Special Account is a special account for the purposes of the Public Governance, Performance and Accountability Act 2013.
318‑5 Credits to the Risk Equalisation Special Account
There must be credited to the *Risk Equalisation Special Account amounts equal to the following:
(a) amounts received by *APRA by way of:
(i) *risk equalisation levy; or
(ii) *late payment penalty in respect of unpaid amounts of risk equalisation levy;
(b) any of the following other amounts received by APRA:
(i) amounts received under paragraph 45(b), or section 46, of the Private Health Insurance (Prudential Supervision) Act 2015;
(ii) repayments of collapsed insurer assistance payments (within the meaning of section 54H of the Australian Prudential Regulation Authority Act 1998);
(c) amounts paid to the Commonwealth or APRA, by a State or Territory, for crediting to the Risk Equalisation Special Account.
Note: An Appropriation Act may contain a provision to the effect that, if any of the purposes of a special account is a purpose that is covered by an item in the Appropriation Act (whether or not the item expressly refers to the special account), then amounts may be debited against the appropriation for that item and credited to that special account.
318‑10 Purpose of the Risk Equalisation Special Account
(1) The purpose of the *Risk Equalisation Special Account is for *APRA to make payments to private health insurers in accordance with the Private Health Insurance (Risk Equalisation Policy) Rules.
Note: See section 80 of the Public Governance, Performance and Accountability Act 2013 (which deals with special accounts).
(2) The Private Health Insurance (Risk Equalisation Policy) Rules must specify:
(a) the circumstances in which private health insurers are to be paid amounts debited from the *Risk Equalisation Special Account; and
(b) the method for working out the amount to be so debited from the Account for payment to a private health insurer; and
(c) the method for working out the amount to be paid, for crediting to the Account, by private health insurers as *risk equalisation levy.
(3) Before making Private Health Insurance (Risk Equalisation Policy) Rules, the Minister must consult *APRA. However, a failure to consult APRA does not affect the validity of those Rules.
Note: This consultation requirement also applies to any repeal or amendment of such Rules: see subsection 33(3) of the Acts Interpretation Act 1901.
318‑15 Record keeping
The Private Health Insurance (Risk Equalisation Administration) Rules may set out requirements for private health insurers that are liable to *risk equalisation levy to keep particular kinds of records, and requirements relating to how those records are to be kept.
Part 6‑8—Disclosure of information
Division 323—Disclosure of information
323‑1 Prohibition on disclosure of information
(1) A person commits an offence if:
(a) the person has, or has at any time had, a duty, function or power under this Act; and
(aa) the duty, function or power is not an *APRA private health insurance duty, function or power; and
(b) the person discloses information to another person; and
(c) the information is *protected information; and
(d) the disclosure is not an *authorised disclosure.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
(1A) An APRA private health insurance duty, function or power is a duty, function or power of *APRA, or that a person has in the person’s capacity as an officer (within the meaning of section 56 of the Australian Prudential Regulation Authority Act 1998), under any of the following:
(a) this Act;
(b) the Private Health Insurance (Prudential Supervision) Act 2015;
(c) the Financial Institutions Supervisory Levies Collection Act 1998, as that Act applies in relation to levies imposed on private health insurers;
(d) the Financial Sector (Collection of Data) Act 2001, as that Act applies in relation to private health insurers.
Note: The disclosure of information regime for information obtained under APRA private health insurance duties, functions and powers is Part 6 of the Australian Prudential Regulation Authority Act 1998 (rather than this Division).
(2) Information is protected information if the information:
(a) either:
(i) is obtained by a person in the course of performing or exercising a duty, function or power under this Act, other than an *APRA private health insurance duty, function or power; or
(ii) was information to which subparagraph (i) applied and is obtained by a person by way of an *authorised disclosure under section 323‑10, 323‑15 or 323‑20; and
(b) relates to a person other than the person who obtained it.
(3) A disclosure of information is an authorised disclosure if the disclosure is one that the person may make under section 323‑5, 323‑10, 323‑15, 323‑20, 323‑25 or 323‑30.
323‑5 Authorised disclosure: official duties
For the purposes of subsection 323‑1(3), a person may disclose information if the disclosure is made:
(a) in the course of performing or exercising a duty, function or power under this Act, other than an *APRA private health insurance duty, function or power; or
(aa) for the purpose of enabling a person to perform or exercise an *APRA private health insurance duty, function or power; or
(b) for the purpose of enabling a person to perform functions in connection with a *medicare program; or
(c) for the purpose of enabling a person to perform functions under:
(i) a provision of the A New Tax System (Medicare Levy Surcharge—Fringe Benefits) Act 1999; or
(ii) a provision of the Medicare Levy Act 1986; or
(iii) a provision of Subdivision 61‑G of the Income Tax Assessment Act 1997; or
(iv) any other provision of the Income Tax Assessment Act 1997, or of any other Act, to the extent that the provision relates to a provision mentioned in subparagraph (i), (ii) or (iii); or
(d) for the purpose of enabling a person to perform functions under Part IID of the Ombudsman Act 1976.
323‑10 Authorised disclosure: sharing information about insurers among agencies
(1) This section applies to information if the information:
(a) relates to any or all of the following:
(i) a private health insurer;
(ii) an applicant to become a private health insurer;
(iii) a person carrying on *health insurance business;
(iv) a *director or *officer of a person mentioned in subparagraph (i), (ii) or (iii); and
(b) is not information of a kind specified in the Private Health Insurance (Information Disclosure) Rules as information that must not be disclosed under this section.
(1A) For the purposes of subsection 323‑1(3), a person to whom subsection (2) applies may disclose the information to:
(a) another person to whom subsection (2) applies; or
(b) the Private Health Insurance Ombudsman; or
(c) an APS employee in, or a person holding or performing the duties of an office in, the Statutory Agency of the Commonwealth Ombudsman; or
(d) *APRA; or
(e) an APRA member or APRA staff member (within the meaning of the Australian Prudential Regulation Authority Act 1998);
if the disclosure is made in accordance with any requirements in the Private Health Insurance (Information Disclosure) Rules.
(2) This subsection applies to the following persons:
(a) the Minister;
(b) the Secretary of the Department;
(c) an APS employee in, or a person holding or performing the duties of an office in, the Department;
(h) the Chief Executive Medicare;
(i) a Departmental employee (within the meaning of the Human Services (Medicare) Act 1973).
323‑15 Authorised disclosure: sharing information about insurers other than among agencies
(1) For the purposes of subsection 323‑1(3), a person may disclose information to another person if:
(a) the information relates to any or all of the following:
(i) a private health insurer;
(ii) an applicant to become a private health insurer;
(iii) a person carrying on *health insurance business;
(iv) a *director or *officer of a person mentioned in subparagraph (i), (ii) or (iii); and
(b) the information is not information of a kind specified in the Private Health Insurance (Information Disclosure) Rules as information that must not be disclosed under this section; and
(c) the disclosure is made in accordance with any requirements in the Private Health Insurance (Information Disclosure) Rules; and
(d) the disclosure is, or is a kind of disclosure, certified by the Minister by written instrument to be in the public interest; and
(e) if there are any conditions specified in the certificate—the conditions are met.
(2) The Minister may specify conditions in a certificate under paragraph (1)(d) relating to the application of the certificate.
(3) A certificate under paragraph (1)(d) is not a legislative instrument.
323‑20 Authorised disclosure: public interest
(1) For the purposes of subsection 323‑1(3), a person may disclose information to another person if:
(a) the information does not relate to any of the following:
(i) a private health insurer;
(ii) an applicant to become a private health insurer;
(iii) a person carrying on *health insurance business;
(iv) a *director or *officer of a person mentioned in subparagraph (i), (ii) or (iii); and
(b) the information is not information of a kind specified in the Private Health Insurance (Information Disclosure) Rules as information that must not be disclosed under this section; and
(c) the disclosure is made in accordance with any requirements in the Private Health Insurance (Information Disclosure) Rules; and
(d) the disclosure is, or is a kind of disclosure, certified by the Minister by written instrument to be in the public interest; and
(e) if there are any conditions specified in the certificate—the conditions are met.
(2) The Minister may specify conditions in a certificate under paragraph (1)(d) relating to the application of the certificate.
(3) A certificate under paragraph (1)(d) is not a legislative instrument.
323‑25 Authorised disclosure: by the Secretary if authorised by affected person
For the purposes of subsection 323‑1(3), the Secretary may disclose information to a person who is expressly or impliedly authorised by the person to whom the information relates to obtain it.
323‑30 Authorised disclosure: court proceedings
For the purposes of subsection 323‑1(3), a person who has, or has at any time had, a duty, function or power under this Act may disclose to a court information that relates to another person for the purposes of an action or proceeding before the court to which that other person is a party.
323‑40 Offence: disclosure of information obtained by certain authorised disclosures
A person commits an offence if:
(a) the person obtains information; and
(b) the person does so by way of an *authorised disclosure under section 323‑10, 323‑15 or 323‑20; and
(c) the person discloses the information; and
(d) the disclosure by the person is not an authorised disclosure.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
323‑45 Offence: soliciting disclosure of information
A person commits an offence if:
(a) the person solicits the disclosure of information from another person; and
(b) the information is *protected information; and
(c) the person knows, or ought reasonably to know, that the information is protected information; and
(d) the disclosure would not be an *authorised disclosure.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
323‑50 Offence: use etc. of unauthorised information
A person commits an offence if:
(a) information is disclosed to the person; and
(b) the information is *protected information; and
(c) the disclosure to the person is not an *authorised disclosure; and
(d) the person knows, or ought reasonably to know, that the disclosure to the person is not an authorised disclosure; and
(e) any of the following apply:
(i) the person solicited the disclosure of the information;
(ii) the person discloses the information;
(iii) the person uses the information.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
323‑55 Offence: offering to supply protected information
A person commits an offence if:
(a) the person:
(i) offers; or
(ii) holds himself or herself out as being able;
to supply (whether or not to a particular person) information about another person; and
(b) the person knows that the information is *protected information; and
(c) the supply would not be an *authorised disclosure.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
Part 6‑9—Review of decisions
Division 328—Review of decisions
328‑1 What this Part is about
Several kinds of decisions made under this Act by the Chief Executive Medicare, *APRA and the Minister are reviewable by the Administrative Appeals Tribunal.
328‑5 AAT review of decisions
An application may be made to the Administrative Appeals Tribunal for the review of any of the following decisions:
Reviewable decisions |
Item | Decision | Provision under which decision is made |
1 | To reject an application for registration of a person in respect of a health insurance policy | section 23‑20 |
2 | To revoke a person’s registration in respect of a health insurance policy | section 23‑35 |
4 | To refuse to make a declaration, or to revoke a declaration, that a facility is a *hospital | subsection 121‑5(6) |
4A | To specify a condition, in relation to a particular facility, to which a declaration that a facility is a *hospital is subject | paragraph 121‑7(1)(b) |
31 | To direct a private health insurer not to make a change that it proposes to make to its *rules | subsection 169‑10(2) |
32 | To refuse a request for a longer period for a private health insurer to respond to a request for an explanation | subsection 191‑1(3) |
33 | To refuse to consent to a private health insurer withdrawing or varying an undertaking | subsection 197‑1(3) |
34 | To give a direction to a private health insurer | section 200‑1 |
35 | To revoke a private health insurer’s status as a *participating insurer | section 206‑1 |
38 | To reject an application to become a *participating insurer | section 279‑5 |
39 | On reconsideration of a decision notifying a private health insurer in relation to a claim for payment under Division 279 | section 279‑45 |
41 | To affirm an original decision by the Chief Executive Medicare that an amount is recoverable as a debt under paragraph 282‑1(1)(h) in respect of a payment made to an individual | section 282‑15 |
42 | To affirm an original decision by the Chief Executive Medicare to set off a debt against an amount otherwise payable to a person or his or her estate | section 282‑15 |
43 | Not to waive, or to waive only a part of, an amount of *late payment penalty | section 307‑20 |
Part 6‑10—Miscellaneous
Division 333—Miscellaneous
333‑1 Delegation by Minister
(1) The Minister may, by writing, delegate all or any of his or her functions or powers under this Act (other than section 66‑10) to:
(a) the Secretary of the Department; or
(b) an SES employee, or acting SES employee, in the Department.
(2) Without limiting subsection (1), the Minister may, by writing, delegate all or any of his or her functions or powers under Part 2‑2 or Part 6‑4 to:
(a) the Chief Executive Medicare; or
(b) a Departmental employee (within the meaning of the Human Services (Medicare) Act 1973); or
(c) an APS employee in the Department.
(3) In performing a function or exercising a power under a delegation, the delegate must comply with any directions of the Minister.
333‑5 Delegation by Secretary
(1) The Secretary of the Department may, by writing, delegate all or any of his or her functions or powers under this Act to an APS employee in the Department.
(2) In performing a function or exercising a power under a delegation, the delegate must comply with any directions of the Secretary.
333‑10 Approved forms
(1) A statement, notice, application or other document is in the approved form if:
(a) it is in the form approved in writing by the person specified in the table as the approver of that form; and
(b) it contains a declaration signed by a person or persons as the form requires (see section 333‑15); and
(c) it contains the information that the form requires, and any further information, statement or document required by the approver, whether in the form or otherwise; and
(d) it is given in the manner (if any) required by the approver.
Person who approves forms |
Item | This person ... | is the approver of these forms ... |
1 | the Secretary of the Department | forms for which there is no other approver specified in this table. |
2 | the Chief Executive Medicare | forms under Part 2‑2. |
(2) Despite subsection (1), a document that satisfies paragraphs (1)(a), (b) and (d) but not paragraph (1)(c) is also in the *approved form if it contains the information required by the approver. The approver must specify the requirement in writing.
(3) The approver may combine in the same *approved form more than one notice, statement, application or other document.
(4) The approver may approve a different *approved form for different kinds of private health insurers.
(5) The Chief Executive Medicare must not approve a form that requires a person to provide:
(a) the *tax file number of any person; or
(b) information about the physical, psychological or emotional health of any person.
333‑15 Signing approved forms
A person who is required to do something in an *approved form must, if the form requires it, sign a declaration, or (if allowed by the form) have a declaration signed on the person’s behalf.
333‑20 Private Health Insurance Rules made by the Minister
(1) The Minister may, by legislative instrument, make Private Health Insurance Rules, specified in the second column of the table, providing for matters:
(a) required or permitted by the corresponding Chapter, Part or section specified in the third column of the table to be provided; or
(b) necessary or convenient to be provided in order to carry out or give effect to that Chapter, Part or section.
Private Health Insurance Rules made by Minister |
Item | Private Health Insurance Rules | Chapter/Part/section |
1 | Private Health Insurance (Incentives) Rules | Part 2‑2, section 206‑1, Part 6‑4 |
2 | Private Health Insurance (Lifetime Health Cover) Rules | Part 2‑3 |
3 | Private Health Insurance (Complying Product) Rules | Chapter 3 and section 188‑1 |
3A | Private Health Insurance (Benefit Requirements) Rules | Part 3‑3 |
4 | Private Health Insurance (Prostheses) Rules | Part 3‑3 |
5 | Private Health Insurance (Accreditation) Rules | section 81‑1 |
6 | Private Health Insurance (Health Insurance Business) Rules | Part 4‑2 |
8 | Private Health Insurance (Health Benefits Fund Policy) Rules | Part 4‑4 |
9 | Private Health Insurance (Data Provision) Rules | Part 4‑5 |
14 | Private Health Insurance (Levy Administration) Rules | Part 6‑6 |
15 | Private Health Insurance (Risk Equalisation Policy) Rules | Part 6‑7 |
16 | Private Health Insurance (Information Disclosure) Rules | Part 6‑8 |
(2) If, under this Act, Private Health Insurance Rules made by the Minister may modify a provision of this Act or another Act (including by modifying the effect, or the requirements, of such a provision), the Rules may do so by adding, omitting or substituting provisions (including effects or requirements of provisions).
Note: There are consultation requirements that apply in relation to the making of Rules mentioned in items 6, 8 and 15 of the above table: see subsections 115‑5(2), 131‑5(2) and 318‑10(3).
333‑25 Private Health Insurance Rules made by APRA
(1) *APRA may, by legislative instrument, make Private Health Insurance Rules, known as Private Health Insurance (Risk Equalisation Administration) Rules, providing for matters mentioned in section 318‑15.
(2) To the extent that Private Health Insurance Rules made under this section deal with a matter that is dealt with in Private Health Insurance Rules made under section 333‑20, they must do so in a way that is not inconsistent with the Rules made under section 333‑20.
333‑30 Regulations
The Governor‑General may make regulations prescribing matters:
(a) required or permitted by this Act to be prescribed; or
(b) necessary or convenient to be prescribed for carrying out or giving effect to this Act.




