
Private Health Insurance Act 2007
No. 31, 2007
An Act to regulate private health insurance, and for related purposes

Private Health Insurance Act 2007
No. 31, 2007
An Act to regulate private health insurance, and for related purposes
Contents
Part 1‑1—Introduction
Division 1—Preliminary
1‑1.................................Short title
1‑5.............................Commencement
1‑10.......................Identifying defined terms
Division 3—Overview of this Act
3‑1..........................What this Act is about
3‑5...........................Incentives (Chapter 2)
3‑10..........Complying health insurance products (Chapter 3)
3‑15...................Private health insurers (Chapter 4)
3‑20.........................Enforcement (Chapter 5)
3‑25........................Administration (Chapter 6)
3‑30..........................Dictionary (Schedule 1)
Division 5—Constitutional matters
5‑1................................Meaning of insurance
5‑5........Act not to apply to State insurance within that State
5‑10..............Compensation for acquisition of property
Chapter 2—Incentives
Part 2‑1—Introduction
Division 15—Introduction
15‑1......................What this Chapter is about
Part 2‑2—Premiums reduction and incentive payments schemes
Division 20—Introduction
20‑1.........................What this Part is about
20‑5............Private Health Insurance (Incentives) Rules
Division 23—Premiums reduction scheme
Subdivision 23‑A—Amount of reduction
23‑1........................Reduction in premiums
23‑5...............................Meaning of incentive amount
23‑10Reduction after a person 65 years or over ceases to be covered by policy
Subdivision 23‑B—Participation in the premiums reduction scheme
23‑15 Registration as a participant in the premiums reduction scheme
23‑20...........................Refusal to register
23‑25....................................Pre‑1999 participants must keep information up to date
23‑30.........Participants who want to withdraw from scheme
23‑35......................Revocation of registration
23‑40.......................Variation of registration
23‑45.......Retention of applications by private health insurers
Division 26—The incentive payments scheme
Subdivision 26‑A—Amount of incentive payment
26‑1...................Payment in relation to premiums
26‑5Payment after a person 65 years or over ceases to be covered by policy
Subdivision 26‑B—Claiming payments under the incentive payments scheme
26‑10......Claim for payment under incentive payments scheme
26‑15.........................Withdrawal of claim
26‑20.........Determination of claim and payment of amount
26‑25...........Reconsideration of decision refusing a claim
26‑30.............Claimants to keep information up to date
Part 2‑3—Lifetime health cover
Division 31—Introduction
31‑1.........................What this Part is about
31‑5.....Private Health Insurance (Lifetime Health Cover) Rules
Division 34—General rules about lifetime health cover
34‑1Increased premiums for person who is late in taking out hospital cover
34‑5Increased premiums for person who ceases to have hospital cover after his or her lifetime health cover base day
34‑10...Increased premiums stop after 10 years’ continuous cover
34‑15..............................Meaning of hospital cover
34‑20..............................Meaning of permitted days without hospital cover
34‑25..............................Meaning of lifetime health cover base day
34‑30......................When a person is overseas
Division 37—Exceptions to the general rules about lifetime health cover
37‑1......................People born on or before 1 July 1934
37‑5..................People over 31 and overseas on 1 July 2000
37‑10.............................Hardship cases
37‑15............Increases cannot exceed 70% of base rates
37‑20..........................Joint hospital cover
Division 40—Administrative matters relating to lifetime health cover
40‑1..................Notification to insured people etc.
40‑5...Evidence of having had hospital cover, or of a person’s age
Chapter 3—Complying health insurance products
Part 3‑1—Introduction
Division 50—Introduction
50‑1......................What this Chapter is about
50‑5.....Private Health Insurance Rules relevant to this Chapter
Part 3‑2—Community rating
Division 55—Principle of community rating
55‑1.........................What this Part is about
55‑5....................Principle of community rating
55‑10............................Closed products
Part 3‑3—Requirements for complying health insurance products
Division 60—Introduction
60‑1.........................What this Part is about
Division 63—Basic rules about complying health insurance products
63‑1......Obligation to ensure products are complying products
63‑5...............................Meaning of complying health insurance product
63‑10..............................Meaning of complying health insurance policy
Division 66—Community rating requirements
66‑1...................Community rating requirements
66‑5.........................Premium requirement
66‑10..................Minister’s approval of premiums
66‑15...........Entitlement to benefits for general treatment
66‑20.Different amount of benefits depending on where people live
Division 69—Coverage requirements
69‑1........................Coverage requirements
69‑5...............................Meaning of cover
69‑10..............................Meaning of hospital‑substitute treatment
Division 72—Benefit requirements for policies that cover hospital treatment
72‑1..........................Benefit requirements
72‑5.......Rules requirement in relation to provision of benefits
72‑10..................Minimum benefits for prostheses
72‑15.................Ongoing listing fee for prostheses
72‑20.............................Other matters
Division 75—Waiting period requirements
75‑1.....................Waiting period requirements
75‑5...............................Meaning of waiting period
75‑10..............................Meaning of transfers
75‑15..............................Meaning of pre‑existing condition
Division 78—Portability requirements
78‑1........................Portability requirements
Division 81—Quality assurance requirements
81‑1...................Quality assurance requirements
Division 84—Enforcement of this Part
84‑1.......Offence: advertising, offering or insuring under non‑complying policies
84‑5Offence: directors and chief executive officers liable if systems not in place to prevent breaches
84‑10.....................Injunction in relation to non‑complying policies
84‑15...............Remedies for people affected by non‑complying policies
Part 3‑4—Obligations relating to complying health insurance products
Division 90—Introduction
90‑1.........................What this Part is about
Division 93—Giving information to consumers
93‑1.....Maintaining up to date standard information statements
93‑5...............................Meaning of standard information statement
93‑10........Making standard information statements available
93‑15...........Giving information to newly insured people
93‑20.................Keeping insured people up to date
93‑25.....Giving advance notice of detrimental changes to rules
93‑30.............Failure to give information to consumers
Division 96—Giving information to the Department, the Council and the Private Health Insurance Ombudsman
96‑1........Giving standard information statements on request
96‑5....Giving standard information statements for new products
96‑10.........Giving updated standard information statements
96‑15.............Giving additional information on request
96‑20Failure to give information to Department, Council or Private Health Insurance Ombudsman
96‑25Giving information required by the Private Health Insurance (Complying Product) Rules
Division 99—Transfer certificates
99‑1..........................Transfer certificates
Division 102—Private health insurers to offer cover for hospital treatment
102‑1..Private health insurers to offer cover for hospital treatment
Chapter 4—Private health insurers
Part 4‑1—Introduction
Division 110—Introduction
110‑1......................What this Chapter is about
Part 4‑2—Carrying on health insurance business
Division 115—Introduction
115‑1........................What this Part is about
115‑5The Private Health Insurance (Health Insurance Business) Rules
115‑10......Whether a business etc. is health insurance business
Division 118—Prohibition of carrying on health insurance business without registration
118‑1...Carrying on health insurance business without registration
118‑5...............................Injunctions
Division 121—What is health insurance business?
121‑1..............................Meaning of health insurance business
121‑5..............................Meaning of hospital treatment
121‑7..............Conditions on declarations of hospitals
121‑10.............................Meaning of general treatment
121‑15.............................Extension to employee health benefits schemes
121‑20......Exception: accident and sickness insurance business
121‑25..............Exception: liability insurance business
121‑30Exception: insurance business excluded by the Private Health Insurance (Health Insurance Business) Rules
Part 4‑3—Registration
Division 126—Registration
126‑1........................What this Part is about
126‑5........The Private Health Insurance (Registration) Rules
126‑10......................Applying for registration
126‑15..................Requesting further information
126‑20......................Deciding the application
126‑25.......................Notifying the decision
126‑30............Council can be taken to refuse application
126‑35.........Council to maintain record of registrations etc.
126‑40....................Changing registration status
126‑42...................Conversion to for profit status
126‑45....................Cancellation of registration
Part 4‑4—Health benefits funds
Division 131—Introduction
131‑1........................What this Part is about
131‑5..The Private Health Insurance (Health Benefits Fund) Rules
131‑10.............................Meaning of health benefits fund
131‑15.............................Meaning of health‑related business
Division 134—The requirement to have health benefits funds
134‑1.....Private health insurers must have health benefits funds
134‑5Notifying the Council when health benefits funds are established
134‑10..........................Inclusion of health‑related businesses in health benefits funds
Division 137—The operation of health benefits funds
137‑1...................Assets of health benefits funds
137‑5.................Payments to health benefits funds
137‑10.....Expenditure and application of health benefits funds
137‑15.............................Effect of non‑compliance with section 137‑10
137‑20................Investment of health benefits funds
137‑25Restriction on restructure, merger, acquisition or termination of health benefits funds
137‑30.........................Operation of health‑related businesses through health benefits funds
Division 140—The solvency standard for health benefits funds
140‑1..........................Purpose of Division
140‑5...............Council to establish solvency standard
140‑10...................Purpose of solvency standard
140‑15...............Compliance with solvency standard
140‑20.........................Solvency directions
Division 143—The capital adequacy standard for health benefits funds
143‑1..........................Purpose of Division
143‑5..........Council to establish capital adequacy standard
143‑10...............Purpose of capital adequacy standard
143‑15...........Compliance with capital adequacy standard
143‑20....................Capital adequacy directions
Division 146—Restructure, merger and acquisition of health benefits funds
146‑1................Restructure of health benefits funds
146‑5.........Merger and acquisition of health benefits funds
146‑10..............Consent of policy holders not required
146‑15.....................Other laws not overridden
Division 149—Termination of health benefits funds
Subdivision 149‑A—Approving the termination of health benefits funds
149‑1......................Applying for termination
149‑5...................Requesting further information
149‑10......................Deciding the application
149‑15............Council can be taken to refuse application
Subdivision 149‑B—Conducting the termination of health benefits funds
149‑20..........Conduct of funds during termination process
149‑25..............Insurers etc. to give reports to Council
149‑30.....Terminating managers displace management of funds
Subdivision 149‑C—Ending the termination of health benefits funds
149‑35......................Power to end termination
Subdivision 149‑D—Completing the termination of health benefits funds
149‑40..............Completion of the termination process
149‑45Distribution of remaining assets after completion of the termination process
149‑50..Liability of officers of insurers for loss to terminated funds
149‑55..................Report of terminating manager
149‑60......................Applying for winding up
Division 152—Duties and liabilities of directors etc.
152‑5.................Notices to remedy contraventions
152‑10..............Liability of directors in relation to non‑compliance with notices
152‑15....Council may sue in the name of private health insurers
Part 4‑5—Other obligations of private health insurers
Division 157—Introduction
157‑1........................What this Part is about
157‑5...The Private Health Insurance (Insurer Obligations) Rules
Division 160—Appointed actuaries
160‑1..............................Appointment
160‑5.....................Eligibility for appointment
160‑10..................Notification of appointment etc.
160‑15.....................Cessation of appointment
160‑20Compliance with the Private Health Insurance (Insurer Obligations) Rules
160‑25....................Powers of appointed actuary
160‑30..................Actuary’s obligations to report
160‑35.............Qualified privilege of appointed actuary
Division 163—Prudential standards
163‑1Private Health Insurance (Insurer Obligations) Rules to establish prudential standards
163‑5...............Compliance with prudential standards
163‑10.........Notice of breaches of prudential standards etc.
163‑15...............Directions to comply with standards
163‑20.................Failure to comply with directions
Division 166—Disqualified persons
166‑1Private health insurers not to allow disqualified persons to act as directors
166‑5..Disqualified persons must not act for private health insurers
166‑10.............................Effect of non‑compliance
166‑15...............................Who is a disqualified person?
166‑20..................Council may disqualify persons
166‑25...Council may determine that persons are not disqualified
Division 169—Reporting and notification requirements
169‑1.................Copies of reports to policy holders
169‑5.........Information to be given to the Council annually
169‑10.....Private health insurers to notify any changes to rules
169‑15Private health insurers to notify Department and Council about current chief executive officer
Division 172—Miscellaneous
172‑1 Private health insurers to comply with Council’s requirements
172-5 Agreements with medical practitioners
172‑10....Private health insurers to give information to Secretary
172‑15......Restrictions on payment of pecuniary penalties etc.
Chapter 5—Enforcement
Part 5‑1—Introduction
Division 180—Introduction
180‑1......................What this Chapter is about
Part 5‑2—General enforcement methods
Division 185—What this Part is about
185‑1..............................Introduction
185‑5..............................Meaning of enforceable obligation
185‑10.............................Meaning of Council‑supervised obligation
Division 188—Performance indicators
188‑1........................Performance indicators
Division 191—Explanation of private health insurer’s operations
191‑1Minister or Council may seek an explanation from a private health insurer
191‑5...........Writer must respond to insurer’s explanation
Division 194—Investigation of private health insurer’s operations
194‑1..Minister or Council may investigate a private health insurer
194‑5......................Notice to give information
194‑10...................Notice to produce documents
194‑15.......................Notice to give evidence
194‑20...........Offences in relation to investigation notices
194‑25........Authorisation to examine books and records etc.
194‑30...................Minister may consult Council
194‑35...Minister or Council must notify outcome of investigation
Division 197—Enforceable undertakings
197‑1Minister or Council may accept written undertakings given by a private health insurer
197‑5....................Enforcement of undertakings
Division 200—Ministerial and Council directions
200‑1..............Minister or Council may give directions
200‑5........................Direction requirements
Division 203—Remedies in the Federal Court
203‑1.......Minister or Council may apply to the Federal Court
203‑5....................Declarations of contravention
203‑10......................Pecuniary penalty order
203‑15.........................Compensation order
203‑20.......................Adverse publicity order
203‑25..............................Other order
203‑30..............Time limit for declarations and orders
203‑35 Civil evidence and procedure rules for declarations and orders
203‑40..........Civil proceedings after criminal proceedings
203‑45.........Criminal proceedings during civil proceedings
203‑50..........Criminal proceedings after civil proceedings
203‑55Evidence given in proceedings for penalty not admissible in criminal proceedings
203‑60........Minister or Council may require person to assist
203‑65Relief from liability for contravening an enforceable obligation
203‑70......................Powers of Federal Court
Division 206—Revoking entitlement to offer rebate as a premium reduction
206‑1...........Revocation of status of participating insurer
Part 5‑3—Enforcement of health benefits fund requirements
Division 211—Introduction
211‑1........................What this Part is about
211‑5..........................Purpose of this Part
211‑10The Private Health Insurance (Health Benefits Fund Enforcement) Rules
211‑15Limitation on external management and termination of health benefits funds
Division 214—Investigations into affairs of private health insurers
214‑1......Investigation of private health insurers by inspectors
214‑5.........................Powers of inspectors
214‑10..............Person may be represented by lawyer
214‑15..........Compliance with requirements of inspectors
214‑20.........................Access to premises
214‑25........................Reports of inspectors
214‑30......................Dissemination of reports
214‑35................Liability for publishing reports etc.
214‑40......................Delegation by inspectors
214‑45.................Records not to be concealed etc.
Division 217—External management of health benefits funds
Subdivision 217‑A—Preliminary
217‑1..........................Purpose of Division
217‑5......The basis of the law relating to external management
Subdivision 217‑B—Appointment of external managers
217‑10.............Council may appoint external managers
217‑15.........Grounds of appointment of external managers
217‑20.....External managers to displace management of funds
Subdivision 217‑C—Duties and powers of external managers
217‑25....................Duties of external managers
217‑30.............Additional powers of external managers
217‑35......Protection of property during external management
217‑40Rights of chargee, owner or lessor of property of fund under external management
Subdivision 217‑D—Procedure relating to voluntary deeds of arrangement
217‑45Matters that may be included in the Private Health Insurance (Health Benefits Fund Enforcement) Rules
Subdivision 217‑E—External managers’ reports to Council
217‑50..........External managers to give reports to Council
217‑55............Dealing with reports given to the Council
217‑60.......Court orders in respect of schemes of arrangement
Subdivision 217‑F—Miscellaneous
217‑65........When an external management begins and ends
217‑70Effect of things done during external management of health benefits funds
217‑75..................Disclaimer of onerous property
217‑80.........Application of provisions of Corporations Act
Division 220—Ordering the termination of health benefits funds
220‑1....Applications by external managers to the Federal Court
220‑5Orders made on applications for appointments of terminating managers
220‑10..................Binding nature of Court orders
220‑15.......................Notice of appointments
Chapter 6—Administration
Part 6‑1—Introduction
Division 230—Introduction
230‑1......................What this Chapter is about
Part 6‑2—Private Health Insurance Ombudsman
Division 235—Introduction
235‑1.....................Principal object of this Part
235‑5..........Private Health Insurance (Ombudsman) Rules
Division 238—Establishment and functions
238‑1Establishment of office of Private Health Insurance Ombudsman
238‑5.......Functions of Private Health Insurance Ombudsman
Division 241—Complaints
Subdivision 241‑A—Relevant complaints
241‑1.....................Who may make a complaint
241‑5.........Persons against whom complaints may be made
241‑10.......................Grounds for complaint
Subdivision 241‑B—Dealing with complaints
241‑15.....................Initial receipt of complaint
241‑20.................Ways of dealing with complaints
241‑25Referral to the Australian Competition and Consumer Commission
241‑30.......................Referral to other bodies
241‑35..............Deciding not to deal with a complaint
Subdivision 241‑C—Referral to subjects of complaints
241‑40.............Referral to the subject of the complaint
Subdivision 241‑D—Investigation of complaints
241‑45.....................Investigation of complaint
241‑50Minister may direct Private Health Insurance Ombudsman to investigate, or to continue to investigate, a complaint
Subdivision 241‑E—Recommendations and reports
241‑55...Recommendations as a result of referral or investigation
241‑60Report to Minister on outcome of investigation under Subdivision 241‑D
Subdivision 241‑F—Miscellaneous
241‑65.................Complainant to be kept informed
Division 244—Investigations
Subdivision 244‑A—Investigations
244‑1.......................Initiating investigations
244‑5................Investigations at Minister’s request
Subdivision 244‑B—Recommendations and reports
244‑10..........Recommendations as a result of investigation
244‑15Report to Minister on outcome of investigations under this Division
244‑20Consultation with Australian Competition and Consumer Commission
Division 247—Mediation
247‑1........................Conducting mediation
247‑5..........Participation in mediation may be compulsory
247‑10.......Medical practitioners may appoint representatives
247‑15................Conduct of compulsory mediation
247‑20............Admissibility of things said in mediation
247‑25.....................Appointment of mediators
Division 250—Information‑gathering
250‑1..............................Information‑gathering
250‑5........................Limits on information‑gathering
250‑10................Disclosure of personal information
Division 253—Provisions relating to the Private Health Insurance Ombudsman
253‑1...Appointment of the Private Health Insurance Ombudsman
253‑5.......................Validity of appointments
253‑10........................Acting appointments
253‑15...................Remuneration and allowances
253‑20........................Outside employment
253‑25..........................Leave of absence
253‑30..............................Resignation
253‑35....................Termination of appointment
253‑40Disclosure of interest by Private Health Insurance Ombudsman
253‑45...Statutory agency etc. for purposes of Public Service Act
253‑50............................Annual report
253‑55..............................Delegation
253‑60Private Health Insurance Ombudsman and staff not personally liable
Division 256—Miscellaneous
256‑1....................Protection from civil actions
256‑5.............................Victimisation
256‑10Giving information about the Private Health Insurance Ombudsman
Part 6‑3—Private Health Insurance Administration Council
Division 261—Introduction
261‑1........................What this Part is about
261‑5..........The Private Health Insurance (Council) Rules
Division 264—Continuation, purposes, functions and powers
264‑1.....................Continuation of the Council
264‑5......................Objectives of the Council
264‑10......................Functions of the Council
264‑15.................Report on private health insurers
264‑20................................Powers
264‑25.......................Directions by Minister
Division 267—Constitution and administration
267‑1.....................Constitution of the Council
267‑5......................Appointment of members
267‑10......................Meetings of the Council
267‑15.....................Delegation by the Council
267‑20.........................Modification of the Commonwealth Authorities and Companies Act 1997
Division 270—Members
270‑1......................Terms and conditions etc.
270‑5.......................Validity of appointments
270‑10........................Acting Commissioner
270‑15Deputy Commissioner to act as Commissioner in certain circumstances
270‑20.....Powers and duties of persons acting as Commissioner
270‑25...........Remuneration and allowances of members
270‑30..........................Leave of absence
270‑35..............................Resignation
270‑40....................Termination of appointment
270‑45.......................Disclosure of interests
Division 273—Chief Executive Officer and staff
273‑1.......................Chief Executive Officer
273‑5.................Duties of Chief Executive Officer
273‑10.........................Conflict of interests
273‑15........................Staff and consultants
273‑20..Remuneration and allowances of Chief Executive Officer
273‑25..........Leave of absence of Chief Executive Officer
Part 6‑4—Administration of premiums reduction and incentive payments schemes
Division 276—Introduction
276‑1........................What this Part is about
Division 279—Provisions applying only to premiums reduction scheme
Subdivision 279‑A—Reimbursement of private health insurers for premiums reduced under scheme
279‑1.........Participating insurers may claim reimbursement
279‑5.........................Participating insurers
279‑10......................Requirements for claims
279‑15.........Amounts payable to the private health insurer
279‑20..Notifying private health insurers if amount is not payable
279‑25..Additional payment if insurer claims less than entitlement
279‑30........Additional payment if insurer makes a late claim
279‑35.................Content and timing of application
279‑40.......................Decision on application
279‑45....................Reconsideration of decisions
Subdivision 279‑B—Powers of Medicare Australia CEO in relation to participating insurers
279‑50................Audits by Medicare Australia CEO
279‑55Medicare Australia CEO may require production of applications
Division 282—Provisions applying to premiums reduction scheme and incentive payments scheme
Subdivision 282‑A—When and how payments can be recovered
282‑1........................Recovery of payments
282‑5..................Interest on amounts recoverable
282‑10Medicare Australia CEO may set off debts against amounts payable
282‑15...Reconsideration of certain decisions under this Division
Subdivision 282‑B—Miscellaneous
282‑20.......Notification requirements—private health insurers
282‑25.......Use etc. of information relating to another person
282‑30.Information to be provided to the Commissioner of Taxation
282‑35..............................Delegation
282‑40............................Appropriation
Part 6‑5—External managers and terminating managers
Division 287—Introduction
287‑1........................What this Part is about
287‑5.......The Private Health Insurance (Management) Rules
Division 290—Powers of managers
290‑1.........................Powers of managers
290‑5Officers etc. not to perform functions etc. while fund is under management
290‑10........Managers act as agents of private health insurers
Division 293—Information concerning, and records and property of, health benefits funds
293‑1...................Directors etc. to help managers
293‑5.................Managers’ rights to certain records
293‑10Only manager can deal with property of fund under management
293‑15Order for compensation where officer involved in void transaction
Division 296—Provisions incidental to appointment of managers
296‑1.....................Remuneration of managers
296‑5.............Council may give directions to managers
296‑10............Termination of appointments of managers
296‑15....................Acts of managers valid etc.
296‑20...............................Indemnity
296‑25.........................Qualified privilege
Division 299—Miscellaneous
299‑1Time for doing act does not run while act prevented by this Division
299‑5........Continued application of other provisions of Act
299‑10Modifications of this Act in relation to health benefits funds under management
299‑15...........Order of Court to be binding on all persons
299‑20....................Jurisdiction of Federal Court
299‑25Private Health Insurance (Management) Rules dealing with various matters
Part 6‑6—Private health insurance levies
Division 304—Introduction
304‑1........................What this Part is about
304‑5.....Private Health Insurance (Levy Administration) Rules
304‑10.............................Meaning of private health insurance levy
Division 307—Collection and recovery of private health insurance levies
307‑1........When private health insurance levy must be paid
307‑5.........................Late payment penalty
307‑10............Payment of levy and late payment penalty
307‑15...........Recovery of levy and late payment penalty
307‑20Waiver of late payment penalty for levies other than collapsed insurer levy
307‑25Waiver of collapsed insurer levy and late payment penalty for that levy
307‑30.............................Other matters
Division 310—Returns, requesting information and keeping records
310‑1.....Returns must be lodged with Council and Department
310‑5......................Insurer must keep records
310‑10.........Council may request information from insurer
Division 313—Power to enter premises and search for documents
313‑1.......Authorised officer may enter premises with consent
313‑5......Authorised officer may enter premises under warrant
313‑10....................Announcement before entry
313‑15..............Executing a warrant to enter premises
313‑20.............................Identity cards
Part 6‑7—Private Health Insurance Risk Equalisation Trust Fund
Division 318—Private Health Insurance Risk Equalisation Trust Fund
318‑1.....Private Health Insurance Risk Equalisation Trust Fund
318‑5...Amounts to be paid into the Risk Equalisation Trust Fund
318‑10.........Operation of the Risk Equalisation Trust Fund
318‑15......Administration of the Risk Equalisation Trust Fund
Part 6‑8—Disclosure of information
Division 323—Disclosure of information
323‑1.............Prohibition on disclosure of information
323‑5...............Authorised disclosure: official duties
323‑10Authorised disclosure: sharing information about insurers among agencies
323‑15Authorised disclosure: sharing information about insurers other than among agencies
323‑20..............Authorised disclosure: public interest
323‑25Authorised disclosure: by the Secretary or Council if authorised by affected person
323‑30............Authorised disclosure: court proceedings
323‑35Authorised disclosure: Council’s public information and agency cooperation functions
323‑40Offence: disclosure of information obtained by certain authorised disclosures
323‑45..........Offence: soliciting disclosure of information
323‑50..........Offence: use etc. of unauthorised information
323‑55.......Offence: offering to supply protected information
Part 6‑9—Review of decisions
Division 328—Review of decisions
328‑1........................What this Part is about
328‑5......................AAT review of decisions
Part 6‑10—Miscellaneous
Division 333—Miscellaneous
333‑1........................Delegation by Minister
333‑5.......................Delegation by Secretary
333‑10...........................Approved forms
333‑15......................Signing approved forms
333‑20.....Private Health Insurance Rules made by the Minister
333‑25.....Private Health Insurance Rules made by the Council
333‑30..............................Regulations
Schedule 1—Dictionary
1 Dictionary

Private Health Insurance Act 2007
No. 31, 2007
An Act to regulate private health insurance, and for related purposes
[Assented to 30 March 2007]
The Parliament of Australia enacts:
This Act may be cited as the Private Health Insurance Act 2007.
This Act commences on 1 April 2007.
1‑10 Identifying defined terms
(1) Many of the terms in this Act are defined in the Dictionary in Schedule 1.
(2) Most of the terms that are defined in the Dictionary are identified by an asterisk appearing at the start of the term: as in “*health benefits fund”. The footnote with the asterisk contains a signpost to the Dictionary.
(3) An asterisk usually identifies the first occurrence of a term in a section (if not divided into subsections), subsection, definition, table item or diagram. Later occurrences of the term in the same provision are not usually asterisked.
(4) Terms are not asterisked in headings, notes, examples or guides.
(5) If a term is not identified by an asterisk, disregard that fact in deciding whether or not to apply to that term a definition or other interpretation provision.
(6) The following basic terms used throughout the Act are not identified with an asterisk:
Terms that are not identified with an asterisk | ||
Item | This term ... | is defined in ... |
1 | Council | the Dictionary in Schedule 1 |
2 | Federal Court | the Dictionary in Schedule 1 |
3 | insurance | section 5‑1 |
4 | Medicare Australia CEO | the Dictionary in Schedule 1 |
5 | Private Health Insurance Ombudsman | the Dictionary in Schedule 1 |
6 | private health insurer | the Dictionary in Schedule 1 |
Division 3—Overview of this Act
This Act is about private health insurance. It:
(a) provides incentives to encourage people to have private health insurance; and
(b) sets out rules governing private health insurance *products; and
(c) imposes requirements about how insurers conduct *health insurance business.
Chapter 2 provides the following incentives:
(a) reductions in premiums for *complying health insurance policies;
(b) payments by the Commonwealth in relation to premiums paid for complying health insurance policies;
(c) a lifetime health cover scheme, under which premiums may rise for people who do not maintain private health insurance from an early age.
3‑10 Complying health insurance products (Chapter 3)
Chapter 3 requires insurers who make private health insurance available to people to do so in a non‑discriminatory way, to offer *products that comply with this Act, and to meet certain other obligations imposed by this Act in relation to those products.
3‑15 Private health insurers (Chapter 4)
Chapter 4 requires registration of anyone carrying on *health insurance business, and imposes obligations aimed at ensuring health insurance businesses, and in particular *health benefits funds, are conducted appropriately.
Chapter 5 provides for a range of enforcement mechanisms aimed at monitoring and ensuring compliance with this Act and protecting the interests of *policy holders.
3‑25 Administration (Chapter 6)
Chapter 6 contains administrative and machinery provisions relating to the operation of this Act.
The Dictionary in Schedule 1 contains definitions of terms used throughout this Act.
Division 5—Constitutional matters
In this Act:
insurance means insurance to which paragraph 51(xiv) of the Constitution applies.
5‑5 Act not to apply to State insurance within that State
This Act does not apply with respect to State insurance that does not extend beyond the limits of the State concerned.
5‑10 Compensation for acquisition of property
(1) If the operation of this Act would result in an acquisition of property from a person otherwise than on just terms, the Commonwealth is liable to pay a reasonable amount of compensation to the person.
(2) If the Commonwealth and the person do not agree on the amount of the compensation, the person may institute proceedings in the Federal Court for the recovery from the Commonwealth of such reasonable amount of compensation as the court determines.
(3) In this section:
acquisition of property has the same meaning as in paragraph 51(xxxi) of the Constitution.
just terms has the same meaning as in paragraph 51(xxxi) of the Constitution.
15‑1 What this Chapter is about
This Chapter contains the following incentives to encourage people to have private health insurance:
(a) reductions in premiums (see Division 23);
(b) payments in return for payments of premiums under complying health insurance policies (see Division 26);
(c) lifetime health cover (see Part 2‑3).
Part 2‑2—Premiums reduction and incentive payments schemes
To encourage people to take out, and continue to hold, private health insurance, this Part provides that people may either:
(a) reduce the premiums payable for their complying health insurance policies by participating in the premiums reduction scheme in Division 23; or
(b) receive a payment from the Commonwealth under Division 26 in partial reimbursement for a payment of premiums under a complying health insurance policy.
Note: The premiums reduction scheme and the incentive payments scheme are complemented by the private health insurance offset provided for by Subdivision 61‑H of the Income Tax Assessment Act 1997.
20‑5 Private Health Insurance (Incentives) Rules
Matters relating to the *premiums reduction scheme and the *incentive payments scheme are also dealt with in the Private Health Insurance (Incentives) Rules. The provisions of this Part indicate when a particular matter is or might be dealt with in these Rules.
Note: The Private Health Insurance (Incentives) Rules are made by the Minister under section 333‑20.
Division 23—Premiums reduction scheme
Subdivision 23‑A—Amount of reduction
(1) The amount of premiums payable under a *complying health insurance policy in respect of a financial year is reduced in accordance with this section if a person is a *participant in the *premiums reduction scheme in respect of the policy.
(2) The amount of the reduction is the sum of:
(a) 30% of the amount of premiums payable under the policy in respect of days in the financial year on which no person covered by the policy was aged 65 years or over; and
(b) 35% of the amount of premiums payable under the policy in respect of days in the financial year on which:
(i) at least one person covered by the policy was aged 65 years or over; and
(ii) no person covered by the policy was aged 70 years or over; and
(c) 40% of the amount of premiums payable under the policy in respect of days in the financial year on which at least one person covered by the policy was aged 70 years or over.
(3) However, if, before 1 January 1999, a person was registered or eligible to be registered under the Private Health Insurance Incentives Act 1997 in respect of the policy, the amount of the reduction is the greater of:
(a) the amount worked out under subsection (2); and
(b) the *incentive amount for the policy for the financial year.
(4) If the amount of premiums is payable in respect of only part of a financial year, the amount of the reduction is worked out using this formula:
where:
part of year means the number of days in the part of the financial year.
whole year reduction means the amount that would have been the reduction if the premium had been payable in respect of the whole financial year.
23‑5 Meaning of incentive amount
(1) The incentive amount for a *complying health insurance policy for a financial year is the amount worked out under this table:
Incentive amount | ||||
Item | Number and kinds of people covered by the policy | Policy covers *hospital treatment but not *general treatment | Policy covers *general treatment but not *hospital treatment | Policy covers *hospital treatment and *general treatment |
1 | 3 or more people | $350 | $100 | $450 |
2 | One *dependent child and one other person | $350 | $100 | $450 |
3 | 2 people neither of whom is a *dependent child | $200 | $50 | $250 |
4 | One person | $100 | $25 | $125 |
(2) If the amount of premiums is payable in respect of only part of a financial year, the incentive amount is worked out using this formula:
23‑10 Reduction after a person 65 years or over ceases to be covered by policy
(1) If:
(a) at any time, premiums under an insurance policy (the original policy) were reduced by 35% or 40% because a person aged 65 years or over (the entitling person) was insured under the original policy; and
(b) at that time, another person (other than a *dependent child) was also insured under the original policy; and
(c) the entitling person subsequently ceases to be insured under the original policy;
subsections 23‑1(2) and (3) apply in relation to a *complying health insurance policy (whether or not the original policy) under which the other person is insured (other than for the purposes of working out the *incentive amount) as if:
(d) the entitling person were also insured under that policy; and
(e) the entitling person were the same age as the age at which he or she ceased to be insured under the original policy.
(2) Subsection (1) ceases to apply if a person (other than a *dependent child) who was not insured under the original policy at the time the entitling person ceased to be insured under it becomes insured under the *complying health insurance policy.
(3) Subsection (1) does not apply if its application would result in the reduction under subsection 23‑1(2) or (3) being less than it would otherwise have been.
(4) Paragraph (1)(a) applies in relation to premiums reduced by 35% or 40% whether the reduction was under this Part or under Chapter 3 of the Private Health Insurance Incentives Act 1998.
Subdivision 23‑B—Participation in the premiums reduction scheme
23‑15 Registration as a participant in the premiums reduction scheme
(1) A person may apply to a private health insurer, in the *approved form, to become a *participant in the *premiums reduction scheme in respect of a *complying health insurance policy issued by the insurer if:
(a) the insurer is a *participating insurer; and
(b) either or both of the following apply:
(i) the person has paid, or the person’s employer has paid as a *fringe benefit on the person’s behalf, a premium under the policy in respect of a financial year;
(ii) the person is insured under the policy (and is not a *dependent child); and
(c) the person meets any requirements specified in the Private Health Insurance (Incentives) Rules for the purposes of this paragraph.
(2) A private health insurer that receives an application under subsection (1) must notify the Medicare Australia CEO of the application, in the *approved form, no more than 14 days (or any other period determined by the Medicare Australia CEO) after receiving the application.
(3) If notified of an application and satisfied that paragraphs (1)(a), (b) and (c) apply, the Medicare Australia CEO must register the applicant as a *participant in respect of the policy.
(4) The Medicare Australia CEO must notify the private health insurer that issued the policy if the Medicare Australia CEO registers a person as a *participant in the *premiums reduction scheme in respect of the policy.
(1) If the Medicare Australia CEO refuses to register the applicant in respect of a policy, the Medicare Australia CEO must give the applicant, and the private health insurer that issued the policy, notice of the refusal together with reasons for the refusal.
Note: Refusals to register are reviewable under Part 6‑9.
(2) The applicant is taken to be registered as a *participant in respect of the policy if the Medicare Australia CEO does not give notice of refusal within 14 days after receiving the notice under subsection 23‑15(2) from the private health insurer to which the applicant applied for registration.
23‑25 Pre‑1999 participants must keep information up to date
(1) If, before 1 January 1999, a person was registered or eligible to be registered under the Private Health Insurance Incentives Act 1997 in respect of the policy, a *participant in respect of the policy must notify the private health insurer that issued the policy if there is a change in a detail:
(a) stated in an application under subsection 23‑15(1); or
(b) relating to the number of people insured under the policy, or to whether any of those people are *dependent children;
that the participant should reasonably expect will affect the *incentive amount for the policy for a financial year. The participant must give the notice no more than 30 days after the change occurs.
(2) A person commits an offence if:
(a) the person is required by subsection (1) to give a notice to a private health insurer if a detail mentioned in that subsection changes as mentioned in that subsection; and
(b) the person fails to comply with the requirement.
Penalty: 60 penalty units.
(3) Subsection 4K(2) of the Crimes Act 1914 does not apply to the obligation to provide information under subsection (1).
(4) A private health insurer must notify the Medicare Australia CEO of each notice the insurer receives under subsection (1), in the *approved form and no more than 14 days (or any other period determined by the Medicare Australia CEO) after receiving the notice.
23‑30 Participants who want to withdraw from scheme
(1) A *participant must notify the private health insurer that issued the policy in respect of which a person is a participant if the person no longer wishes to be registered in respect of the policy.
(2) A private health insurer must notify the Medicare Australia CEO of each notice the insurer receives under subsection (1), in the *approved form and no more than 14 days (or any other period determined by the Medicare Australia CEO) after receiving the notice.
(3) If notified under subsection (2), the Medicare Australia CEO must revoke the person’s registration in respect of the policy.
23‑35 Revocation of registration
(1) The Medicare Australia CEO must revoke a person’s registration in respect of a *complying health insurance policy if the Medicare Australia CEO is satisfied that the person is not eligible to participate in the *premiums reduction scheme in respect of the policy.
Note: Revocations of registration are reviewable under section Part 6‑9.
(2) Revocation of registration under subsection (1) does not affect a person’s right to make another application for registration under section 23‑15.
(3) The Medicare Australia CEO must give notice of the revocation of a person’s registration in respect of a *complying health insurance policy to the person, and to the private health insurer that issued the policy, within 28 days after the day on which the revocation occurs.
23‑40 Variation of registration
(1) A private health insurer must notify the Medicare Australia CEO if the treatments *covered by a *complying health insurance policy, issued by the private health insurer and in respect of which a person is a *participant, are varied.
(2) On receiving such a notice, the Medicare Australia CEO must vary the details of the registration accordingly and give notice of the variation to the private health insurer.
23‑45 Retention of applications by private health insurers
(1) A private health insurer must retain an application made to it under subsection 23‑15(1) for the period of 5 years beginning on the day on which the application was made.
(2) The private health insurer may retain the application in any form approved in writing by the Medicare Australia CEO.
(3) An application retained in such a form must be received in all courts or tribunals as evidence as if it were the original.
Division 26—The incentive payments scheme
Subdivision 26‑A—Amount of incentive payment
26‑1 Payment in relation to premiums
(1) A person is entitled to a payment under this Division if:
(a) the person has paid, or a person’s employer has paid as a *fringe benefit for the person, premiums under a *complying health insurance policy for the whole or a part of a financial year; and
(b) the amount of premiums was not reduced under Division 23; and
(c) the person meets any requirements specified in the Private Health Insurance (Incentives) Rules for the purposes of this paragraph.
(2) The amount of the payment is the sum of:
(a) 30% of the amount of the premium paid by a person, or by a person’s employer as a *fringe benefit for the person, under the policy in respect of days in the financial year on which no person covered by the policy was aged 65 years or over;
(b) 35% of the amount of the premium paid by a person, or by a person’s employer as a fringe benefit for the person, under the policy in respect of days in the financial year on which:
(i) at least one person covered by the policy was aged 65 years or over; and
(ii) no person covered by the policy was aged 70 years or over;
(c) 40% of the amount of the premium paid by a person, or by a person’s employer as a fringe benefit for the person, under the policy in respect of days in the financial year on which at least one person covered by the policy was aged 70 years or over.
(3) However, if, before 1 January 1999, a person was registered, or eligible to be registered, under the Private Health Insurance Incentives Act 1997 in respect of the policy, the amount of the payment is the greater of:
(a) the amount worked out under subsection (2); and
(b) the *incentive amount for the policy for the financial year.
(4) The total amount payable under this Division for a policy for a financial year is reduced by the amount of any tax offset received under Subdivision 61‑H of the Income Tax Assessment Act 1997 for the total amount of the premium paid by a person, or by a person’s employer as a *fringe benefit for the person, under the policy for that financial year.
(5) A private health insurer must give a person a receipt, in the *approved form, for a payment of an amount of premiums (other than an amount that has been reduced under Division 23) if the person requests it.
26‑5 Payment after a person 65 years or over ceases to be covered by policy
(1) If:
(a) at any time, a payment of an amount of 35% or 40% of the premiums payable under an insurance policy (the original policy) was made to a person because a person aged 65 years or over (the entitling person) was insured under the original policy; and
(b) at that time, another person (other than a *dependent child) was insured under the original policy; and
(c) the entitling person subsequently ceases to be insured under the original policy;
subsections 26‑1(2) and (3) apply in relation to a *complying health insurance policy (whether or not the original policy) under which the other person is insured (other than for the purposes of working out the *incentive amount) as if:
(d) the entitling person were also insured under that policy; and
(e) the entitling person were the same age as the age at which he or she ceased to be insured under the original policy.
(2) Subsection (1) ceases to apply if a person (other than a *dependent child) who was not insured under the original policy at the time the entitling person ceased to be insured under it becomes insured under the *complying health insurance policy.
(3) Subsection (1) does not apply if its application would result in the amount payable under subsection 26‑1(2) or (3) being less than it would otherwise have been.
(4) Paragraph (1)(a) applies in relation to a payment of an amount of 35% or 40% of the premiums payable under an insurance policy whether the payment was made under this Part or under Chapter 2 of the Private Health Insurance Incentives Act 1998.
Subdivision 26‑B—Claiming payments under the incentive payments scheme
26‑10 Claim for payment under incentive payments scheme
(1) To be paid an amount to which a person is entitled under section 26‑1, the person must make a claim in the *approved form.
(2) The claim must be sent to or lodged at an office of Medicare Australia, or a place approved by the Medicare Australia CEO, in:
(a) the financial year in which the payment of premiums to which the claim relates was made; or
(b) the next financial year.
A claimant may at any time, by writing sent to or lodged at an office of Medicare Australia, or a place approved by the Medicare Australia CEO, withdraw a claim.
26‑20 Determination of claim and payment of amount
(1) The Medicare Australia CEO must make a decision granting or refusing the claim within 14 days after the day on which the claim is made.
(2) If the claim is granted, the Medicare Australia CEO must pay to the claimant the amount to which the claimant is entitled.
(3) If the claim is refused, the Medicare Australia CEO must give the claimant a notice stating that the claim has been refused and setting out the reasons for the refusal.
26‑25 Reconsideration of decision refusing a claim
(1) If a claim is refused, the claimant may apply to the Medicare Australia CEO for the Medicare Australia CEO to reconsider the decision.
(2) The application must:
(a) be in writing; and
(b) set out the reasons for the application.
(3) The application must be made within:
(a) 28 days after the day on which the claimant was notified of the decision; or
(b) if, either before or after the end of that period of 28 days, the Medicare Australia CEO extends the period within which the application may be made—the extended period for making the application.
(4) The Medicare Australia CEO must:
(a) reconsider the decision; and
(b) either affirm or revoke the decision;
within 28 days after receiving the application for reconsideration.
Note: Decisions affirming original decisions are reviewable under Part 6‑9.
(5) If the Medicare Australia CEO revokes the decision, the revocation is taken to be a decision granting the claim.
(6) The Medicare Australia CEO must give the claimant a notice stating his or her decision on the reconsideration together with a statement of his or her reasons for the decision.
(7) The Medicare Australia CEO is taken, for the purposes of this Subdivision, to have made a decision affirming the original decision if the Medicare Australia CEO has not told the claimant of the decision on the reconsideration before the end of the period of 28 days.
26‑30 Claimants to keep information up to date
(1) If, after a claimant has made a claim under section 26‑10 for a payment of an amount:
(a) a matter, event or circumstance occurs that affects the claimant’s entitlement to the payment; or
(b) a change occurs in the premium, or in the amounts or frequency of the payments in respect of the premium, under the policy;
the claimant must, within 30 days after the occurrence of the matter, event, circumstance or change, notify the Medicare Australia CEO of the details of the matter, event, circumstance or change.
(2) A person commits an offence if:
(a) the person is required by subsection (1) to notify the Medicare Australia CEO of the details of a matter, event, circumstance or change mentioned in that subsection; and
(b) the person fails to comply with the requirement.
Penalty: 60 penalty units.
(3) Subsection 4K(2) of the Crimes Act 1914 does not apply to the obligation to provide information under subsection (1).
Part 2‑3—Lifetime health cover
People are encouraged to take out hospital cover by the time they turn 30. A person who is older than 30 when he or she takes out hospital cover for the first time, or who drops hospital cover for a period after having turned 30, may have to pay higher premiums for hospital cover. This scheme is known as lifetime health cover.
31‑5 Private Health Insurance (Lifetime Health Cover) Rules
Matters relating to lifetime health cover are also dealt with in the Private Health Insurance (Lifetime Health Cover) Rules. The provisions of this Part indicate when a particular matter is or might be dealt with in these Rules.
Note: The Private Health Insurance (Lifetime Health Cover) Rules are made by the Minister under section 333‑20.
Division 34—General rules about lifetime health cover
34‑1 Increased premiums for person who is late in taking out hospital cover
(1) A private health insurer must increase the amount of premiums payable for *hospital cover in respect of an *adult if the adult did not have hospital cover on his or her *lifetime health cover base day.
(2) The amount of the increase is worked out as follows:
where:
base rate, for *hospital cover, is the amount of premiums that would be payable for the cover if:
(a) the premiums were not increased under this Part; and
(b) there was no discount of the kind allowed under subsection 66‑5(2).
lifetime health cover age, in relation to an *adult who takes out *hospital cover after his or her *lifetime health cover base day, means the adult’s age on the 1 July before the day on which the adult took out the hospital cover.
(1) A private health insurer must increase the amount of premiums payable for *hospital cover in respect of an *adult if, after the adult’s *lifetime health cover base day, the adult ceases to have hospital cover.
(2) The amount of the increase is worked out as follows:
where:
base rate is the *base rate for the *hospital cover.
years without hospital cover is the number obtained by:
(a) dividing by 365 the number of days (other than *permitted days without hospital cover), after the first day on which subsection (1) applied to the *adult, on which he or she did not have *hospital cover; and
(b) rounding up the result to the nearest whole number.
(3) Any increase under this section in the amount of premiums payable for *hospital cover is in addition to any increase under section 34‑1 in the amount of premiums payable for that hospital cover.
34‑10 Increased premiums stop after 10 years’ continuous cover
(1) A private health insurer must stop increasing the amount of premiums payable for *hospital cover in respect of an *adult under this Part if the adult has had hospital cover (including under an *applicable benefits arrangement), the premiums for which have been increased under this Part or *old Schedule 2:
(a) for a continuous period of 10 years; or
(b) for a period of 10 years that has been interrupted only by *permitted days without hospital cover or periods during which the adult was taken to have had hospital cover otherwise than because of paragraph 34‑15(2)(a) (none of which count towards the 10 years).
(2) The amount must stop being increased on the day after the last day of the 10 year period.
(3) The amount of premiums payable for *hospital cover in respect of the *adult must start to be increased under this Part again if:
(a) after the end of the 10 year period, the adult ceases to have hospital cover; and
(b) the adult later takes out hospital cover again; and
(c) the days in the period between ceasing to have the cover and taking it out again are not all *permitted days without hospital cover in respect of the adult.
(4) Subsection (3) does not prevent this section applying again in respect of any later 10 year period.
(5) In subsection (1):
old Schedule 2 means Schedule 2 to the National Health Act 1953 as in force before 1 April 2007.
34‑15 Meaning of hospital cover
(1) Hospital cover is so much of a *complying health insurance policy as *covers *hospital treatment. An *adult has hospital cover if he or she is insured under a complying health insurance policy that covers hospital treatment.
(2) An *adult is taken to have *hospital cover:
(a) at any time during which the adult was covered by an *applicable benefits arrangement; or
(b) at any time during which the adult holds a *gold card; or
(c) at any time during which the adult is in a class of adults specified in the Private Health Insurance (Lifetime Health Cover) Rules for the purposes of this paragraph.
(3) In this section:
gold card means a card that evidences a person’s entitlement to be provided with treatment:
(a) in accordance with the Treatment Principles prepared under section 90 of the Veterans’ Entitlements Act 1986; or
(b) in accordance with a determination made under section 286 of the Military Rehabilitation and Compensation Act 2004 in respect of the provision of treatment.
34‑20 Meaning of permitted days without hospital cover
(1) Any of the following days that occur after an *adult ceases, for the first time after his or her *lifetime health cover base day, to have *hospital cover are permitted days without hospital cover in respect of that adult:
(a) days on which the cover was suspended by the private health insurer in accordance with the rules for suspensions set out in the Private Health Insurance (Lifetime Health Cover) Rules;
(b) days (not counting days covered by paragraph (a)) on which the adult is *overseas that form part of a continuous period overseas of more than one year;
(c) the first 1,094 days (not counting days covered by paragraph (a) or (b)) on which the adult did not have hospital cover.
(2) The Private Health Insurance (Lifetime Health Cover) Rules may specify days that, despite subsection (1), are taken not to be *permitted days without hospital cover.
34‑25 Meaning of lifetime health cover base day
(1) A person’s lifetime health cover base day is the day worked out by using this diagram:
(2) A person is a new arrival if:
(a) the person entered Australia for the first time on or after 1 July 2000; and
(b) the person was not an Australian citizen or permanent resident of Australia at the time of the entry.
(3) A person’s medicare eligibility day is the day on which the person is registered by the Medicare Australia CEO as an eligible person within the meaning of section 3 of the Health Insurance Act 1973.
(4) Despite subsection (1), if:
(a) on or before 1 April 2007, a person’s Schedule 2 application day had arrived for the purposes of the National Health Act 1953; and
(b) the person had *hospital cover on 1 April 2007; and
(c) the person has had hospital cover continuously since that day;
the person’s lifetime health cover base day is the person’s Schedule 2 application day. For this purpose, a day on which the person has hospital cover does not include a *permitted day without hospital cover or a day on which the person would otherwise be taken to have hospital cover because of subsection 34‑15(2).
34‑30 When a person is overseas
Without limiting when a person is taken to be *overseas for the purposes of this Part:
(a) a person who lives on Norfolk Island is taken, while the person is living there, to be overseas; and
(b) any period in which a person returns to Australia for less than 90 days counts as part of a continuous period overseas; and
(c) a person is taken to have returned from overseas if the person returns to Australia for a period of at least 90 days.
Division 37—Exceptions to the general rules about lifetime health cover
37‑1 People born on or before 1 July 1934
(1) The amount of premiums payable for *hospital cover in respect of an *adult does not increase under this Part if the adult was born on or before 1 July 1934.
(2) However, this section does not prevent section 37‑20 applying to the *hospital cover in respect of any *adults who were born after 1 July 1934.
37‑5 People over 31 and overseas on 1 July 2000
A person:
(a) who turned 31 on or before 1 July 2000; and
(b) who was *overseas on 1 July 2000;
is taken, for the purposes of section 34‑1, to have had *hospital cover on the person’s *lifetime health cover base day.
A person is treated for the purposes of this Part as if he or she had *hospital cover on 1 July 2000 if a determination under clause 10 of Schedule 2 to the National Health Act 1953 (as in force immediately before 1 April 2007) had effect in relation to the person immediately before 1 April 2007.
37‑15 Increases cannot exceed 70% of base rates
The maximum amount of any increase under this Part in the amount of premiums payable for *hospital cover in respect of an *adult is an amount equal to 70% of the *base rate for the hospital cover.
(1) If:
(a) more than one *adult is covered under the same *hospital cover; and
(b) the amount of premiums payable for the cover in respect of at least one of those adults is increased under this Part;
the amount of the premiums payable for the cover in respect of all of the adults is increased.
(2) The amount of the increase in the premiums payable for the cover is worked out by:
(a) dividing the *base rate for the cover by the number of *adults it covers; and
(b) using that rate to work out for each adult what the amount of the increase for that adult (if any) would be; and
(c) adding together the results of paragraph (b).
Division 40—Administrative matters relating to lifetime health cover
40‑1 Notification to insured people etc.
(1) A private health insurer must comply with any requirements specified in the Private Health Insurance (Lifetime Health Cover) Rules relating to providing information to:
(a) *adults in respect of *hospital cover with the private health insurer; and
(b) other adults who apply for, or inquire about, that hospital cover;
about increases under this Part in the amounts of premiums payable for hospital cover in respect of those adults.
(2) A private health insurer must comply with any requirements specified in the Private Health Insurance (Lifetime Health Cover) Rules relating to providing information to other private health insurers about increases under this Part in the amounts of premiums payable for *hospital cover with the private health insurer.
(3) The Private Health Insurance (Lifetime Health Cover) Rules may require or permit a private health insurer to provide information of a kind referred to in this section in the form of an age notionally attributed, to an *adult or other person, as the age from which the adult or other person will be treated as having had continuous *hospital cover.
(4) A private health insurer must keep separate records in relation to each *adult who has *hospital cover.
(5) When an *adult ceases to be *covered by *hospital cover under which more than one adult was covered, the private health insurer must notify each other adult that the adult has ceased to be covered by the cover.
40‑5 Evidence of having had hospital cover, or of a person’s age
A private health insurer must comply with any requirements specified in the Private Health Insurance (Lifetime Health Cover) Rules relating to whether, and in what circumstances, particular kinds of evidence are to be accepted, for the purposes of this Part, as conclusive evidence of:
(a) whether a person had *hospital cover at a particular time, or during a particular period; or
(b) a person’s age.
Chapter 3—Complying health insurance products
50‑1 What this Chapter is about
Broadly, health insurance that is made available to the public must meet the requirements in this Chapter. This means that:
(a) the insurance must be community‑rated (that is, made available in a way that does not discriminate between people) (see Part 3‑2); and
(b) the insurance must be in the form of a complying health insurance product (see Part 3‑3); and
(c) the private health insurers who make the products available must meet certain obligations to people insured or seeking to be insured under the products (see Part 3‑4).
50‑5 Private Health Insurance Rules relevant to this Chapter
Matters relating to *complying health insurance products are also dealt with in the Private Health Insurance (Complying Product) Rules, the Private Health Insurance (Benefit Requirements) Rules, the Private Health Insurance (Prostheses) Rules and the Private Health Insurance (Accreditation) Rules. The provisions of this Chapter indicate when a particular matter is or may be dealt with in these Rules.
Note: These Rules are all made by the Minister under section 333‑20.
Division 55—Principle of community rating
To ensure that everybody who chooses has access to health insurance, the principle of community rating prevents private health insurers from discriminating between people on the basis of their health or for any other reason described in this Part.
55‑5 Principle of community rating
(1) A private health insurer must not:
(a) take or fail to take any action; or
(b) in making a decision, have regard or fail to have regard to any matter;
that would result in the insurer *improperly discriminating between people who are or wish to be insured under a *complying health insurance policy of the insurer.
(2) Improper discrimination is discrimination that relates to:
(a) the suffering by a person from a chronic disease, illness or other medical condition or from a disease, illness or medical condition of a particular kind; or
(b) the gender, race, sexual orientation or religious belief of a person; or
(c) the age of a person, except to the extent allowed under Part 2‑3 (lifetime health cover); or
(d) where a person lives, except to the extent allowed under subsection 66‑10(2) or section 66‑20; or
(e) any other characteristic of a person (including but not just matters such as occupation or leisure pursuits) that is likely to result in an increased need for *hospital treatment or *general treatment; or
(f) the frequency with which a person needs hospital treatment or general treatment; or
(g) the amount or extent of the benefits to which a person becomes entitled during a period under a *complying health insurance policy, except to the extent allowed under section 66‑15; or
(h) any matter set out in the Private Health Insurance (Complying Product) Rules for the purposes of this paragraph.
(3) Despite subsection (2), discrimination by a *restricted access insurer is not improper discrimination to the extent to which the insurer:
(a) takes or fails to take an action; or
(b) in making a decision, has regard or fails to have regard to a matter;
only to ensure that its *complying health insurance products are not made available to persons to whom its constitution prohibits it from making the products available.
The principle of community rating in section 55‑5 does not prevent a private health insurer from refusing to make available to a person a *complying health insurance product that the insurer is no longer making available to anyone.
Part 3‑3—Requirements for complying health insurance products
Complying health insurance products (which are made up of complying health insurance policies) are the only kind of insurance that private health insurers are allowed to make available as part of their health insurance business (see section 63‑1 and Division 84). This Part sets out the requirements that an insurance policy must meet in order to be a complying health insurance policy.
Division 63—Basic rules about complying health insurance products
63‑1 Obligation to ensure products are complying products
(1) A private health insurer must ensure that the only kind of insurance that it makes available as part of its *health insurance business is insurance in the form of *complying health insurance products.
(2) However, subsection (1) does not apply in relation to *health insurance business of a kind that the Private Health Insurance (Complying Product) Rules specify is excluded from subsection (1).
63‑5 Meaning of complying health insurance product
(1) A complying health insurance product is a *product made up of *complying health insurance policies.
(2) A product is all the insurance policies issued by a private health insurer:
(a) that *cover the same treatments; and
(b) that provide benefits that are worked out in the same way; and
(c) whose other terms and conditions are the same as each other.
(2A) A product subgroup, of a *product, is all the insurance policies in the product:
(a) under which the addresses of the people insured, as known to the private health insurer, are located in the same *risk equalisation jurisdiction; and
(b) under which the same kind of insured group (within the meaning of the Private Health Insurance (Complying Product) Rules) is insured.
(2B) The Private Health Insurance (Complying Product) Rules may specify insured groups for the purposes of paragraph (2A)(b). An insured group may be specified by reference to any or all of the number of people in the group, the kind of people in the group, or any other matter. A group may consist of only one person.
(3) Different premiums may be payable under policies in the same *product.
63‑10 Meaning of complying health insurance policy
A complying health insurance policy is an insurance policy that meets:
(a) the community rating requirements in Division 66; and
(b) the coverage requirements in Division 69; and
(c) if the policy *covers *hospital treatment—the benefit requirements in Division 72; and
(d) the waiting period requirements in Division 75; and
(e) the portability requirements in Division 78; and
(f) the quality assurance requirements in Division 81; and
(g) any requirements set out in the Private Health Insurance (Complying Product) Rules for the purposes of this paragraph.
Division 66—Community rating requirements
66‑1 Community rating requirements
(1) An insurance policy meets the community rating requirements in this Division if:
(a) the policy prohibits the private health insurer that issued the policy from breaching the principle of community rating in section 55‑5 in relation to a person insured under the policy; and
(b) the policy has no terms or conditions that would allow the insurer to *improperly discriminate against a person insured under the policy; and
(c) the only discounts (if any) available under the policy are discounts allowed under subsection 66‑5(2); and
(d) unless the policy is issued under a new *product (see subsection (2))—the premiums payable under the policy meet the premium requirement in section 66‑5.
(2) For the purposes of paragraph (1)(d), an insurance policy is issued under a new *product if the amount of premiums charged under policies in the product has not changed since the first policy in the product was issued.
(1) For the purposes of paragraph 66‑1(1)(d), the premiums payable under an insurance policy for a period meet the premium requirement in this section if the amount of premiums payable under the policy for the period:
(a) is the amount specified for the *product subgroup to which the policy belongs in the most recent approval under section 66‑10; or
(b) is the proportion, for the period, of that amount; or
(c) would be the amount mentioned in paragraph (a) or (b) except that a different amount is payable:
(i) because of the application of Part 2‑3 (lifetime health cover); or
(ii) because of a discount or discounts allowed under subsection (2), if the total percentage discount (not counting discounts available for the reason in paragraph (3)(f)) does not exceed the percentage specified in the Private Health Insurance (Complying Product) Rules as the maximum percentage discount allowed; or
(iii) because of a combination of subparagraphs (i) and (ii).
(2) A discount is allowed if:
(a) it is for a reason in subsection (3); and
(b) the discount is also available for that reason under every policy in the *product; and
(c) if there are different percentage discounts available for that reason—the same percentage discount is available on the same basis under every policy in the product; and
(d) any other conditions set out in the Private Health Insurance (Complying Product) Rules are met.
(3) A discount may be for any of these reasons:
(a) because premiums are paid at least 3 months in advance;
(b) because premiums are paid by payroll deduction;
(c) because premiums are paid by pre‑arranged automatic transfer from an account at a bank or other financial institution;
(d) because the persons insured under the policy have agreed to communicate with the private health insurer, and make claims under the policy, by electronic means;
(e) because a person insured under the policy is, under the *rules of the private health insurer, treated as belonging to a contribution group;
(f) because the insurer is not required to pay a levy in relation to the policy under a law of a State or Territory;
(g) for a reason set out in the Private Health Insurance (Complying Product) Rules.
66‑10 Minister’s approval of premiums
(1) A private health insurer that proposes to change the premiums charged under a *complying health insurance product must apply to the Minister for approval of the change:
(a) in the *approved form; and
(b) at least 60 days before the day on which the insurer proposes the change to take effect.
(2) The application may propose different changes for policies in the *product, but the proposed changed amount must be the same for each policy in the product that belongs to the same *product subgroup.
(3) The Minister must, by written instrument, approve the proposed changed amount or amounts, unless the Minister is satisfied that a change that would increase the amount or amounts would be contrary to the public interest.
(4) If the Minister approves the proposed changed amount or amounts, the approval has effect:
(a) from the day specified in the approval as the day the change takes effect; and
(b) until replaced by another approval for the *product under this section.
(6) If the Minister refuses to approve the proposed changed amount or amounts, the Minister must table the Minister’s reasons for refusal in each House of the Parliament no later than 15 sitting days of that House after the refusal.
(7) An instrument made under subsection (3) is not a legislative instrument.
66‑15 Entitlement to benefits for general treatment
Neither:
(a) the community rating principle in section 55‑5; nor
(b) the community rating requirement in paragraph 66‑1(1)(b);
prevents a private health insurer from determining a person’s entitlement under a *complying health insurance policy to a benefit for *general treatment (other than *hospital‑substitute treatment) in respect of a period by having regard to the amount of benefits for that kind of treatment already claimed for the person in respect of the period.
66‑20 Different amount of benefits depending on where people live
Neither:
(a) the community rating principle in section 55‑5; nor
(b) the community rating requirements in section 66‑1;
prevents the amount of a benefit for a treatment under a *complying health insurance policy from being different from the amount of a benefit for the same treatment under another policy that is in the same *product, if the difference is only because the persons insured under the policies live in different *risk equalisation jurisdictions.
Division 69—Coverage requirements
(1) An insurance policy meets the coverage requirements in this Division if:
(a) the only treatments the policy *covers are:
(i) specified treatments that are *hospital treatment; or
(ii) specified treatments that are hospital treatment and specified treatments that are *general treatment; or
(iii) specified treatments that are general treatment but none that are hospital‑substitute treatment; and
(b) if the policy provides a benefit for anything else—the provision of the benefit is authorised by the Private Health Insurance (Complying Product) Rules.
(2) Despite paragraph (1)(a), the policy must also *cover any treatment that a policy of its kind is required by the Private Health Insurance (Complying Product) Rules to cover.
(3) Despite paragraph (1)(a), the policy must not *cover any treatment that a policy of its kind is not allowed under the Private Health Insurance (Complying Product) Rules to cover.
(1) An insurance policy covers a treatment if, under the policy, the insurer undertakes liability in respect of some or all loss arising out of a liability to pay fees or charges relating to the provision of goods or a service that is or includes that treatment.
(2) An insurance policy also covers a treatment if the insurer provides an insured person, or arranges for an insured person to be provided with, goods or a service that is or includes that treatment.
(3) If an insurance policy *covers a treatment in the way described in subsection (2), this Part applies as if the provision of the goods or service were a benefit provided under the policy.
69‑10 Meaning of hospital‑substitute treatment
Hospital‑substitute treatment means *general treatment that:
(a) substitutes for an episode of *hospital treatment; and
(b) is any of, or any combination of, nursing, medical, surgical, podiatric surgical, diagnostic, therapeutic, prosthetic, pharmacological, pathology or other services or goods intended to manage a disease, injury or condition; and
(c) is not specified in the Private Health Insurance (Complying Product) Rules as a treatment that is excluded from this definition.
Division 72—Benefit requirements for policies that cover hospital treatment
(1) An insurance policy that *covers *hospital treatment meets the benefit requirements in this Division if:
(a) the policy meets the requirements in the table in subsection (2); and
(b) the policy meets any requirements specified in the Private Health Insurance (Complying Product) Rules to be benefit requirements; and
(c) the policy does not provide benefits for:
(i) the cost of care and accommodation in an aged care service (within the meaning of the Aged Care Act 1997); or
(ii) a charge for a pharmaceutical benefit supplied under Part VII of the National Health Act 1953, unless the circumstances of the charge are covered by section 92B of that Act; or
(iii) any other treatment specified in the Private Health Insurance (Complying Product) Rules as a treatment for which benefits must not be provided; and
(d) the *rules of the private health insurer that issues the policy meet the rules requirement in section 72‑5.
(2) These are the requirements that a policy must meet for the purposes of paragraph (1)(a):
Requirements that a policy that *covers *hospital treatment must meet | ||
Item | There must be a benefit for ... | The amount of the benefit must be ... |
1 | any part of *hospital treatment that is one or more of the following: (a) psychiatric care; (b) rehabilitation; (c) palliative care; if the treatment is provided in a *hospital and no *medicare benefit is payable for that part of the treatment. | at least the amount set out, or worked out using the method set out, in the Private Health Insurance (Benefit Requirements) Rules as the minimum benefit, or method for working out the minimum benefit, for that treatment. |
2 | *hospital treatment *covered under the policy for which a *medicare benefit is payable. | (a) if the charge for the treatment is less than the *schedule fee for the treatment—so much of the charge (if any) as exceeds 75% of the schedule fee; and (b) otherwise—at least 25% of the schedule fee for the treatment. |
3 | if the policy *covers *hospital‑substitute treatment—hospital‑substitute treatment covered under the policy for which a *medicare benefit is payable. | (a) if the charge for the treatment is less than the *schedule fee for the treatment—so much of the charge (if any) as exceeds 75% of the schedule fee; and (b) otherwise—at least 25% of the schedule fee for the treatment; but the benefit must not be provided if a medicare benefit of an amount that is at least 85% of the schedule fee is claimed for the treatment. |
4 | (a) *hospital treatment *covered under the policy; and (b) if the policy covers *hospital‑substitute treatment—hospital‑substitute treatment covered under the policy; that is the provision of a prosthesis of a kind listed in the Private Health Insurance (Prostheses) Rules in circumstances: (c) in which a *medicare benefit is payable; or (d) set out in the Private Health Insurance (Prostheses) Rules for the purposes of this table item. | (a) at least the amount set out, or worked out using the method set out, in the Private Health Insurance (Prostheses) Rules as the minimum benefit, or method for working out the minimum benefit, for the prosthesis; and (b) if the Private Health Insurance (Prostheses) Rules set out an amount, or a method for working out an amount, as the maximum benefit, or method for working out the maximum benefit, for the prosthesis—no more than that amount or the amount worked out using that method. |
5 | any treatment for which the Private Health Insurance (Benefit Requirements) Rules specify there must be a benefit. | at least the amount set out, or worked out using the method set out, in the Private Health Insurance (Benefit Requirements) Rules as the minimum benefit, or method for working out the minimum benefit, for that treatment. |
Note: If a private health insurer provides an insured person with, or arranges for an insured person to be provided with, treatment, it is treated as a benefit for the purposes of this Division (see subsection 69‑5(3)).
72‑5 Rules requirement in relation to provision of benefits
(1) For the purposes of paragraph 72‑1(1)(d), the *rules of the private health insurer that issues the policy meet the rules requirement in this section if the rules have the effect required by subsection (2).
(2) The effect required is that if, under an agreement or arrangement with a private health insurer, a particular *health care provider (other than a *medical practitioner) provides particular *hospital treatment or *hospital‑substitute treatment to people insured under the same *complying health insurance product of the insurer, any charge for the treatment:
(a) that is payable by an insured person; and
(b) which is not recoverable by a benefit under the product;
must be the same for all of the people insured under the product, irrespective of:
(c) the frequency with which that provider provides that particular treatment to people insured under that product; or
(d) any other matter.
(3) The Private Health Insurance (Complying Product) Rules may modify the effect required by subsection (2) in relation to all or particular kinds of *complying health insurance products, benefits, treatments or *health care providers. To the extent the Rules do so, the rules requirement is taken to be met if the conditions in the Rules are met.
72‑10 Minimum benefits for prostheses
(1) Private Health Insurance (Prostheses) Rules made for the purposes of item 4 of the table in subsection 72‑1(2) must only list a kind of prosthesis if:
(a) an application has been made under subsection (2) in relation to that kind of prosthesis; and
(b) the Minister has granted the application.
(2) A person may apply to the Minister to have the Private Health Insurance (Prostheses) Rules list a prosthesis of the kind to which the application relates.
(3) The application must be:
(a) in the *approved form; and
(b) accompanied by any application fee imposed under the Private Health Insurance (Prostheses Application and Listing Fees) Act 2007.
(4) The Minister must inform the applicant in writing of the Minister’s decision whether or not to grant the application. If the Minister decides not to grant the application, the Minister must also inform the applicant of the reason for that decision.
(5) If:
(a) the Minister grants the application; and
(b) the applicant pays to the Commonwealth any initial listing fee imposed under the Private Health Insurance (Prostheses Application and Listing Fees) Act 2007 within 14 days of being informed of the Minister’s decision to grant the application;
the Minister must, on the next occasion when the Minister makes or varies the Private Health Insurance (Prostheses) Rules:
(c) list the kind of prosthesis to which the application relates in those Rules; and
(d) set out in those Rules a minimum benefit for the prosthesis; and
(e) if the Minister considers it appropriate—set out in those Rules a maximum benefit for the prosthesis.
72‑15 Ongoing listing fee for prostheses
(1) This section applies if the Minister lists a kind of prosthesis in the Private Health Insurance (Prostheses) Rules as a result of an application under subsection 72‑10(2).
(2) The applicant must pay to the Commonwealth the ongoing listing fee for which the applicant is liable under the Private Health Insurance (Prostheses Application and Listing Fees) Act 2007, within 28 days of each day specified under that Act as an ongoing listing fee imposition day.
(3) If the applicant fails to pay an ongoing listing fee in accordance with subsection (2), the Minister may remove the kind of prosthesis from the list in the Private Health Insurance (Prostheses) Rules.
The Private Health Insurance (Prostheses) Rules may, in relation to application fees, initial listing fees or ongoing listing fees imposed under the Private Health Insurance (Prostheses Application and Listing Fees) Act 2007, provide for, or for matters relating to, any or all of the following:
(a) methods for payment;
(b) extending the time for payment;
(c) refunding or otherwise applying overpayments.
Division 75—Waiting period requirements
75‑1 Waiting period requirements
(1) An insurance policy meets the waiting period requirements in this Division if the *waiting period that applies to a person who did not *transfer to the policy is no longer than:
(a) for a benefit for *hospital treatment or *hospital‑substitute treatment that is obstetric treatment or treatment for a *pre‑existing condition (other than treatment covered by paragraph (b))—12 months; and
(b) for a benefit for hospital treatment or hospital‑substitute treatment that is psychiatric care, rehabilitation or palliative care (whether or not for a pre‑existing condition)—2 months; and
(c) for any other benefit for hospital treatment or hospital‑substitute treatment—2 months.
(2) The Private Health Insurance (Complying Product) Rules may modify the requirements in subsection (1) in relation to all or particular kinds of private health insurers, benefits or insured persons. To the extent the Rules do so, the waiting period requirements in this Division are taken to be met if the conditions in the Rules are met.
Note: If a private health insurer provides an insured person with, or arranges for an insured person to be provided with, treatment, it is treated as a benefit for the purposes of this Division (see subsection 69‑5(3)).
75‑5 Meaning of waiting period
The waiting period that applies to a person for a benefit under an insurance policy is the period:
(a) starting at the time the person becomes insured under the policy; and
(b) ending at the time specified in the policy;
during which the person is not entitled to the benefit.
A person transfers to a policy (the new policy) from another policy (the old policy) if:
(a) either:
(i) the person is insured under the old policy at the time the person becomes insured under the new policy; or
(ii) the person ceased to be insured under the old policy no more than 7 days, or a longer number of days allowed by the new policy’s insurer for this purpose, before becoming insured under the new policy; and
(b) the old policy is a *complying health insurance policy; and
(c) the person’s premium payments under the old policy were up to date at the time the person became insured under the new policy.
Note: See section 99‑1 about transfer certificates.
75‑15 Meaning of pre‑existing condition
(1) A person insured under an insurance policy has a pre‑existing condition if:
(a) the person has an ailment, illness or condition; and
(b) in the opinion of a *medical practitioner appointed by the insurer that issued the policy, the signs or symptoms of that ailment, illness or condition existed at any time in the period of 6 months ending on the day on which the person became insured under the policy.
(2) In forming an opinion for the purposes of paragraph (1)(b), the *medical practitioner must have regard to any information in relation to the ailment, illness or condition that the medical practitioner who treated the ailment, illness or condition gives him or her.
(3) If:
(a) a private health insurer replaces a *complying health insurance product with another complying health insurance product; and
(b) a person who was insured under a policy that was in the replaced *product is *transferred by the insurer to a policy that is in the replacement product;
the reference in paragraph (1)(b) to the day on which the person became insured under the policy is taken to be a reference to the day on which the person became insured under the replaced policy.
Division 78—Portability requirements
(1) An insurance policy meets the portability requirements in this Division if the policy meets the requirements in subsections (2), (3) and (4).
(2) An insurance policy meets the requirement in this subsection if the *waiting period that applies to a person who *transferred to the policy (the new policy) from another policy (the old policy) is no longer than:
(a) for a benefit for *hospital treatment or *hospital‑substitute treatment that was not *covered under the old policy—the period allowed under section 75‑1; and
(b) for a benefit for hospital treatment or hospital‑substitute treatment that was covered under the old policy—the balance of any unexpired waiting period for that benefit that applied to the person under the old policy.
(3) An insurance policy meets the requirement in this subsection if the policy does not impose on a person who *transferred to the policy any period (other than a *waiting period allowed under subsection (2)) during which the amount of a benefit in relation to any particular *hospital treatment or *hospital‑substitute treatment is less than the amount the person would be eligible for during any other period.
(4) An insurance policy meets the requirement in this subsection if, in relation to a benefit for *hospital treatment or *hospital‑substitute treatment:
(a) that was *covered under the old policy; and
(b) in respect of which a higher excess or higher co‑payment applied under the old policy than is the case under the new policy;
any period during which the higher excess or higher co‑payment continues to apply under the new policy to a person who *transferred to the policy is no longer than the *waiting period allowed under section 75‑1 for a benefit for that treatment.
(5) In working out:
(a) for the purposes of subsection (2) or (4), whether a treatment was *covered under an old policy; or
(b) for the purposes of subsection (3), whether the amount of a benefit under a new policy during a period is less than the amount it would be during another period;
disregard the existence or otherwise of contracts between the insurer in relation to either of the policies and particular *health care providers or groups of health care providers.
(6) The Private Health Insurance (Complying Product) Rules may modify the requirements in this section in relation to all or particular kinds of private health insurers, benefits or insured persons. To the extent the Rules do so, the portability requirements in this Division are taken to be met if the conditions in the Rules are met.
Note: If a private health insurer provides an insured person with, or arranges for an insured person to be provided with, treatment, it is treated as a benefit for the purposes of this Division (see subsection 69‑5(3)).
Division 81—Quality assurance requirements
81‑1 Quality assurance requirements
An insurance policy meets the quality assurance requirements in this Division if the policy prohibits the payment of benefits for a treatment that does not meet the standards in the Private Health Insurance (Accreditation) Rules.
Note: The Private Health Insurance (Accreditation) Rules are made by the Minister under section 333‑20.
Division 84—Enforcement of this Part
84‑1 Offence: advertising, offering or insuring under non‑complying policies
(1) A person commits an offence if:
(a) the person:
(i) advertises a *product; or
(ii) offers a person insurance under a policy; or
(iii) insures a person under a policy; or
(iv) arranges for another person to do a thing mentioned in subparagraph (i), (ii) or (iii); and
(b) the policy, or a policy in the product, *covers *hospital treatment or *general treatment or both (whether or not it covers any other treatment or provides a benefit for anything else); and
(c) the policy is not a *complying health insurance policy.
Penalty: 1,000 penalty units or imprisonment for 5 years, or both.
(2) In imposing a penalty on a private health insurer for an offence under subsection (1), the court:
(a) must have regard to the possible impact of a penalty on the insurer’s capital adequacy, solvency and the level of premiums for its *complying health insurance products; and
(b) must not impose a penalty if satisfied that doing so would adversely affect the insurer’s capital adequacy or solvency, or be likely to lead to an increase in premiums for its products.
A person commits an offence if:
(a) the person is a *director or *chief executive officer of a private health insurer; and
(b) the insurer commits an offence under section 84‑1; and
(c) the person failed to exercise due diligence to ensure that adequate systems were in place to prevent the insurer from committing the offence.
Penalty: 1,000 penalty units or imprisonment for 5 years, or both.
84‑10 Injunction in relation to non‑complying policies
(1) If a private health insurer has engaged, is engaging, or is proposing to engage, in conduct:
(a) that contravenes or would contravene section 63‑1; or
(b) that is or that would be an offence against section 84‑1;
the Federal Court may, on application by a person mentioned in subsection (3), grant an injunction restraining the insurer from engaging in the conduct.
(2) If:
(a) a private health insurer has refused or failed, is refusing or failing, or is proposing to refuse or fail, to do a thing; and
(b) the refusal or failure:
(i) contravenes or would contravene section 63‑1; or
(ii) is or would be an offence against section 84‑1;
the Federal Court may, on application by a person mentioned in subsection (3), grant an injunction requiring the insurer to do the thing.
(3) For the purposes of subsections (1) and (2), an application may be made by:
(a) the Minister; or
(b) the Council; or
(c) any other person.
(4) The court may grant an interim injunction pending the determination of an application under subsection (1) or (2).
(5) The court must not require an applicant for an injunction to give an undertaking as to damages as a condition of granting an interim injunction.
(6) The court may discharge or vary an injunction granted under this section.
(7) The power of the court to grant an injunction restraining a private health insurer from engaging in conduct may be exercised:
(a) whether or not it appears to the court that the insurer intends to engage again, or to continue to engage, in conduct of that kind; and
(b) whether or not the insurer has previously engaged in conduct of that kind.
(8) The power of the court to grant an injunction requiring a private health insurer to do a thing may be exercised:
(a) whether or not it appears to the court that the insurer intends to refuse or fail again, or to continue to refuse or fail, to do that thing; and
(b) whether or not the insurer has previously refused or failed to do that thing.
84‑15 Remedies for people affected by non‑complying policies
On application by the Minister, if the Federal Court is satisfied that:
(a) a private health insurer has engaged in conduct that contravenes section 63‑1 or is an offence against section 84‑1; or
(b) both:
(i) a private health insurer has refused or failed to do a thing; and
(ii) that refusal or failure contravenes section 63‑1 or is an offence against section 84‑1;
the court may order the insurer to do either or both of the following:
(c) take specified action to ensure that an insurance policy becomes a *complying health insurance policy;
(d) take specified action to ensure that a person insured under an insurance policy is put in the position the person would have been in, had the policy always been a complying health insurance policy.
Part 3‑4—Obligations relating to complying health insurance products
Private health insurers have obligations to people insured under their complying health insurance products and people seeking to become insured under those products. Private health insurers also have to keep the Department, the Council and the Private Health Insurance Ombudsman informed about their health insurance business.
Division 93—Giving information to consumers
93‑1 Maintaining up to date standard information statements
(1) A private health insurer must ensure that it maintains at all times an *up to date *standard information statement:
(a) for each *product subgroup of each *complying health insurance product that it makes available; and
(b) for each product subgroup of each complying health insurance product under which it insures people.
(1A) A single *standard information statement may be the standard information statement for more than one *product subgroup of a *complying health insurance product if the premiums payable under policies in the subgroups the statement covers are the same.
(2) The *standard information statement for a *product subgroup of a *complying health insurance product is up to date at a particular time, if, at that time, the information in the statement is accurate.
(3) A private health insurer commits an offence if there is no *standard information statement for a *product subgroup of a *complying health insurance product of the insurer.
Penalty: 60 penalty units.
(4) A private health insurer commits an offence if:
(a) there is a *standard information statement for a *product subgroup of a *complying health insurance product of the insurer; and
(b) the standard information statement is not *up to date.
Penalty: 60 penalty units.
(5) Strict liability applies to subsections (3) and (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
93‑5 Meaning of standard information statement
(1) A standard information statement for a *product subgroup of a *complying health insurance product is a statement about the product subgroup that contains the information, and is in the form, set out in the Private Health Insurance (Complying Product) Rules.
(2) The Private Health Insurance (Complying Product) Rules may set out methods by which *standard information statements are to be made available to people who ask for information about *complying health insurance products.
93‑10 Making standard information statements available
A private health insurer must ensure that, if a person asks an *officer, employee or agent of the insurer for information about a *complying health insurance product of the insurer:
(a) the person is told about the *standard information statement for the *product subgroup that is likely to apply to the person and how to obtain a copy of the statement; and
(b) if the person asks for a copy—the person is given an *up to date copy of the statement for that subgroup.
93‑15 Giving information to newly insured people
(1) A private health insurer must ensure that, when an *adult first becomes insured under a *complying health insurance policy of the insurer, the adult is given:
(a) an *up to date copy of the *standard information statement for the *product subgroup that the policy belongs to, by a method (if any) set out in the Private Health Insurance (Complying Product) Rules; and
(b) details about what the policy *covers and how benefits provided under it are worked out; and
(c) a statement identifying the *health benefits fund to which the policy is referable.
(2) If more than one *adult becomes insured under a single *complying health insurance policy of a private health insurer, the insurer is taken to comply with subsection (1) if the insurer complies with that subsection in relation to only one of those adults.
93‑20 Keeping insured people up to date
(1) A private health insurer must ensure that an *adult insured under a *complying health insurance policy issued by the insurer is given the *standard information statement for the *product subgroup that the policy belongs to, at least once every 12 months.
(2) A private health insurer must ensure that, if a proposed change to the insurer’s *rules:
(a) is or might be detrimental to the interests of an insured person; and
(b) will require an update to the *standard information statements for a *complying health insurance product of the insurer;
an *adult insured under each *complying health insurance policy in the product:
(c) is informed about the proposed change a reasonable time before the change takes effect; and
(d) is given the updated standard information statement for the *product subgroup that the policy belongs to as soon as practicable after the statement is updated.
(3) A private health insurer must ensure that, if an *adult who is insured under a *complying health insurance policy of the insurer asks an *officer, employee or agent of the insurer for information about what the policy covers or the benefits the policy provides, the adult is given the information as soon as practicable.
(4) If a private health insurer changes the *health benefits fund to which a *complying health insurance policy of the insurer is *referable, the insurer must ensure that:
(a) before the change takes effect, an *adult insured under the policy is given a statement identifying the health benefits fund to which the policy will be referable as a result of the change; or
(b) within 2 weeks after the change takes effect, an adult insured under the policy is given a statement identifying the health benefits fund to which the policy is referable as a result of the change.
Note: The health benefits fund to which a policy is referable may change in accordance with Division 146.
(5) If more than one *adult is insured under a single *complying health insurance policy of a private health insurer, the insurer is taken to comply with subsection (1), (2) or (4) if the insurer complies with the subsection in relation to only one of those adults.
93‑25 Giving advance notice of detrimental changes to rules
(1) A private health insurer must ensure an *adult insured under a *complying health insurance policy issued by the insurer is informed about any proposed change to the insurer’s *rules (other than a change to which subsection 93‑20(2) applies), a reasonable time before the change takes effect, if the proposed change is or might be detrimental to the interests of an insured person.
(2) If more than one *adult is insured under a single *complying health insurance policy of a private health insurer, the insurer is taken to comply with subsection (1) if the insurer complies with that subsection in relation to only one of those adults.
93‑30 Failure to give information to consumers
(1) A private health insurer commits an offence if:
(a) the insurer is required under section 93‑10, 93‑15, 93‑20 or 93‑25 to ensure that a particular thing happens in relation to a particular person; and
(b) the thing does not happen in relation to the person.
Penalty: 60 penalty units.
(2) Strict liability applies to subsection (1).
Note: For strict liability, see section 6.1 of the Criminal Code.
96‑1 Giving standard information statements on request
A private health insurer must ensure that, if:
(a) the Secretary of the Department; or
(b) the Council; or
(c) the Private Health Insurance Ombudsman;
requests the private health insurer for the *standard information statements for a *complying health insurance product of the insurer, the insurer gives the person who made the request *up to date copies of the statements, as soon as practicable after being asked and by the method (if any) specified by the person.
96‑5 Giving standard information statements for new products
A private health insurer must ensure that copies of the *standard information statements for a *complying health insurance product of the insurer are given to:
(a) the Secretary of the Department; and
(b) the Council; and
(c) the Private Health Insurance Ombudsman;
no later than the first day on which the insurer first begins to make the *product available.
96‑10 Giving updated standard information statements
A private health insurer must ensure that, if the *standard information statements for a *complying health insurance product of the insurer are updated, copies of the updated statements are given to:
(a) the Secretary of the Department; and
(b) the Council; and
(c) the Private Health Insurance Ombudsman;
as soon as practicable after the statement is updated.
96‑15 Giving additional information on request
(1) Any of the following:
(a) the Secretary of the Department;
(b) the Council;
(c) the Private Health Insurance Ombudsman;
may request a private health insurer for specified information about, or in relation to, a *complying health insurance product or products, or a *complying health insurance policy, of the insurer.
(2) The request must:
(a) be in writing; and
(b) specify the time by which the information requested is to be given.
(3) The request may specify the manner and form in which the information requested is to be given.
(4) A private health insurer must ensure that the request is complied with, by the time specified in the request or any longer time allowed by the person who made the request.
96‑20 Failure to give information to Department, Council or Private Health Insurance Ombudsman
(1) A private health insurer commits an offence if:
(a) the insurer is required under section 96‑1, 96‑5, 96‑10 or 96‑15 to ensure that a particular thing is given to a particular person; and
(b) the thing is not given to the person.
Penalty: 60 penalty units.
(2) Strict liability applies to subsection (1).
Note: For strict liability, see section 6.1 of the Criminal Code.
96‑25 Giving information required by the Private Health Insurance (Complying Product) Rules
The Private Health Insurance (Complying Product) Rules may set out any or all of the following:
(a) information in relation to *complying health insurance products;
(b) persons to whom the information is to be given (who may include, but need not be limited to, the Secretary of the Department, the Council or the Private Health Insurance Ombudsman);
(c) the time within which, or the intervals at which, the information is to be given to a person;
(d) the manner and form in which the information is to be given to a person.
Division 99—Transfer certificates
Certificate for the insured person
(1) A private health insurer (the old insurer) must, if a person ceases to be insured under a *complying private health insurance policy of the insurer and does not become insured under another policy of the insurer, give the person a certificate under this subsection:
(a) in the *approved form; and
(b) within the period set out in the Private Health Insurance (Complying Product) Rules.
Certificate for the new insurer
(2) A private health insurer (the new insurer) must request a certificate from an old insurer if:
(a) a person who is or has been insured under a *complying health insurance policy of the old insurer *transfers to a complying health insurance policy of the new insurer; and
(b) the person does not give the new insurer the certificate the old insurer gave the person under subsection (1) within 7 days of becoming insured by the new insurer.
The request must be made:
(c) in the *approved form; and
(d) within the period set out in the Private Health Insurance (Complying Product) Rules.
(2A) A private health insurer must not request a certificate except in the circumstances set out in subsection (2).
(3) If a certificate is requested by the new insurer (whether or not the request is in the *approved form or made within the period mentioned in paragraph (2)(d)), the old insurer must give the new insurer a certificate:
(a) in the approved form; and
(b) within the period set out in the Private Health Insurance (Complying Product) Rules.
Offence
(4) A private health insurer commits an offence if:
(a) the insurer is required to do a thing under subsection (1), (2) or (3); and
(b) the insurer does not do the thing.
Penalty: 60 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
Division 102—Private health insurers to offer cover for hospital treatment
102‑1 Private health insurers to offer cover for hospital treatment
At any time when a private health insurer makes available a *complying health insurance product that *covers *general treatment, the insurer must also make available a complying health insurance product that covers *hospital treatment.
Chapter 4—Private health insurers
110‑1 What this Chapter is about
Entities are only permitted to carry on health insurance business if they are registered. Once registered, a number of obligations arise.
The principal obligation is to have health benefits funds, operated in accordance with the requirements of Part 4‑4, for the purpose of health insurance business. (They may, to some degree, also be used for the purpose of health‑related businesses.)
Other obligations include appointment of actuaries, compliance with prudential standards and exclusion of disqualified persons from management.
Part 4‑2—Carrying on health insurance business
Only entities that are registered under Part 4‑3 as health insurers can carry on health insurance business. Other entities can be prevented from carrying on health insurance business.
115‑5 The Private Health Insurance (Health Insurance Business) Rules
The carrying on of *health insurance business is also dealt with in the Private Health Insurance (Health Insurance Business) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Health Insurance Business) Rules are made by the Minister under section 333‑20.
115‑10 Whether a business etc. is health insurance business
The following diagram shows how to work out whether a business or arrangement is *health insurance business:
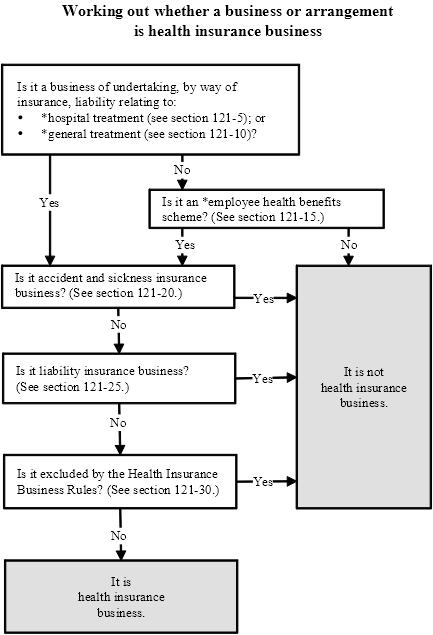
Division 118—Prohibition of carrying on health insurance business without registration
118‑1 Carrying on health insurance business without registration
(1) A person commits an offence if:
(a) the person carries on *health insurance business; and
(b) the person is not a private health insurer.
Penalty: 40 penalty units.
(2) A person commits an offence against subsection (1) in respect of each day during which the person contravenes that section, including the day of a conviction for any such offence or any later day.
Note: See also subsections 4K(3) and (4) of the Crimes Act 1914 in relation to multiple contraventions of this provision.
(1) The Federal Court may grant an injunction in such terms as it determines to be appropriate if, on the application of the Minister, the Council or any other person, the court is satisfied that a person has engaged, or is proposing to engage, in conduct that constitutes or would constitute a contravention of section 118‑1.
(2) The Federal Court may grant an interim injunction pending determination of an application under subsection (1).
(3) The court must not require an applicant for an injunction to give an undertaking as to damages as a condition of granting an interim injunction.
(4) The court may discharge or vary an injunction granted under subsection (1) or (2).
(5) The power of the court to grant an injunction restraining a person from engaging in conduct may be exercised:
(a) whether or not it appears to the court that the person intends to engage again, or to continue to engage, in conduct of that kind; and
(b) whether or not the person has previously engaged in conduct of that kind.
(6) The power of the court to grant an injunction requiring a person to do an act or thing may be exercised:
(a) whether or not it appears to the court that the person intends to refuse or fail again, or to continue to refuse or fail, to do that act or thing; and
(b) whether or not the person has previously refused or failed to do that act or thing.
Division 121—What is health insurance business?
121‑1 Meaning of health insurance business
(1) Health insurance business is:
(a) the business of undertaking liability, by way of insurance; or
(b) an *employee health benefits scheme;
that relates, in a way referred to in subsection (2), to *hospital treatment or *general treatment.
Note: The following kinds of insurance business are not health insurance business:
(a) accident and sickness insurance business (see section 121‑20);
(b) liability insurance business (see section 121‑25);
(c) insurance business excluded by the Private Health Insurance (Health Insurance Business) Rules (see section 121‑30).
(2) The liability by way of insurance, or the arrangement to make payments under the *employee health benefits scheme, must relate to:
(a) loss arising out of a liability to pay fees or charges relating to provision in Australia of such treatment; or
(b) provision in Australia of such treatment; or
(c) the happening of an occurrence connected with the provision in Australia of such treatment; or
(d) the happening of an occurrence in Australia that ordinarily requires the provision of such treatment.
(3) It does not matter for the purposes of paragraph (2)(d) whether payment of benefits to the insured is dependent upon one or more of the following:
(a) such treatment or benefit being provided to the insured;
(b) the insured requiring such treatment or benefit;
(c) fees or charges being payable by the insured in relation to the provision of such treatment or benefit.
121‑5 Meaning of hospital treatment
(1) Hospital treatment is treatment (including the provision of goods and services) that:
(a) is intended to manage a disease, injury or condition; and
(b) is provided to a person:
(i) by a person who is authorised by a *hospital to provide the treatment; or
(ii) under the management or control of such a person; and
(c) either:
(i) is provided at a hospital; or
(ii) is provided, or arranged, with the direct involvement of a hospital.
(2) Without limiting subsection (1), hospital treatment includes any other treatment, or treatment included in a class of treatments, specified in the Private Health Insurance (Health Insurance Business) Rules for the purposes of this subsection.
(3) Without limiting subsection (1) or (2), the reference to treatment in those subsections includes a reference to any of, or any combination of, accommodation, nursing, medical, surgical, podiatric surgical, diagnostic, therapeutic, prosthetic, pharmacological, pathology or other services or goods intended to manage a disease, injury or condition.
(4) Despite subsections (1) and (2), treatment is not *hospital treatment if it is specified in, or is included in a class of treatments specified in, the Private Health Insurance (Health Insurance Business) Rules for the purposes of this subsection.
(5) A hospital is a facility for which a declaration under subsection (6) is in force.
(6) The Minister may, in writing:
(a) declare that a facility is a *hospital; or
(b) revoke such a declaration.
Note: Refusals to make declarations, and revocations of declarations are reviewable under Part 6‑9.
(7) In deciding whether to declare that a facility is a *hospital, or to revoke such a declaration, the Minister must have regard to:
(a) the nature of the facility; and
(b) the range and scope of the services provided, or proposed to be provided, under the management or control of the facility and at or on behalf of the facility; and
(c) whether the necessary approvals by a State or Territory, or by an authority of a State or Territory, have been obtained in relation to the facility; and
(d) whether the accreditation requirements of an appropriate accrediting body have been met; and
(e) whether undertakings have been made, or have been complied with, relating to providing to private health insurers information, of the kind specified in the Private Health Insurance (Health Insurance Business) Rules, relating to treatment of persons insured under *complying health insurance products that are *referable to *health benefits funds; and
(ea) if the Minister is deciding whether to revoke such a declaration—any contravention of conditions to which the declaration is subject; and
(f) any other matters specified in the Private Health Insurance (Health Insurance Business) Rules.
(8) A declaration under subsection (6) that a facility is a *hospital must include either a statement that the hospital is a public hospital or a statement that the hospital is a private hospital.
121‑7 Conditions on declarations of hospitals
(1) A declaration under paragraph 121‑5(6)(a) that a facility is a hospital is subject to:
(a) any conditions specified under subsection (2); and
(b) any conditions that the Minister specifies under subsection (3) in relation to the facility.
Note: Decisions by the Minister to specify conditions in relation to particular facilities are reviewable under Part 6‑9.
(2) The Private Health Insurance (Health Insurance Business) Rules may specify conditions to which declarations under paragraph 121‑5(6)(a) are subject. Any conditions so specified apply to all such declarations, whether or not the declarations were made before the conditions were so specified.
(3) The Minister may specify:
(a) in a declaration under paragraph 121‑5(6)(a) relating to a facility; or
(b) in a written notice given to a facility for which such a declaration is already in force;
conditions, or additional conditions, to which the declaration is subject.
(4) A contravention of a condition to which a declaration under paragraph 121‑5(6)(a) is subject does not cause the declaration to cease to have effect.
Note: Contraventions are taken into consideration in deciding whether to revoke a declaration.
121‑10 Meaning of general treatment
(1) General treatment is treatment (including the provision of goods and services) that:
(a) is intended to manage or prevent a disease, injury or condition; and
(b) is not *hospital treatment.
(2) Without limiting subsection (1), general treatment includes any other treatment, or treatment included in a class of treatments, specified in the Private Health Insurance (Health Insurance Business) Rules for the purposes of this subsection.
(3) Despite subsections (1) and (2), neither of the following is *general treatment:
(a) the rendering in Australia of a service for which *medicare benefit is payable, unless the Private Health Insurance (Health Insurance Business) Rules provide otherwise;
(b) any other treatment, or treatment included in a class of treatments, specified in the Private Health Insurance (Health Insurance Business) Rules for the purposes of this paragraph.
121‑15 Extension to employee health benefits schemes
(1) An arrangement is an employee health benefits scheme if:
(a) the arrangement provides for a person (an employer) to arrange payment in respect of the whole or part of the fees and charges that an employee of, or a person providing services to, the employer incurred in relation to *hospital treatment or *general treatment; and
(b) one or more of the following applies:
(i) the employer is a *constitutional corporation;
(ii) the employer is a body corporate incorporated in a Territory;
(iii) the employer carries on business in a Territory.
(2) It does not matter for the purposes of this section whether the arrangement:
(a) constitutes a business of undertaking liability by way of insurance; or
(b) is a minor or incidental part of the employer’s business; or
(c) does not require the employee, or person providing services, to pay any contributions; or
(d) does not require the employee, or person providing services, to pay contributions that reflect the value of the benefits that the employer is providing under the arrangement; or
(e) provides for the employer to make payments in relation to *hospital treatment, or *general treatment, provided to a person other than the employee or person providing services; or
(f) confers on the employer or another person a discretion whether to make payments.
(3) However, an arrangement:
(a) is not an *employee health benefits scheme merely because, under the arrangement, the employer will pay, or will reimburse employees, or persons providing services, for payment of, one or both of the following:
(i) the premiums payable by them for *complying health insurance policies;
(ii) the difference between benefits payable to them under policies, and amounts that they are liable to pay, for health services provided to them or members of their families; and
(b) is not an employee health benefits scheme if the Private Health Insurance (Health Insurance Business) Rules provide that:
(i) it is not an employee health benefits scheme; or
(ii) arrangements of a class in which it is included are not employee health benefits schemes; and
(c) is not an employee health benefits scheme to the extent (if any) that the arrangement constitutes State insurance within the meaning of paragraph 51(xiv) of the Constitution.
121‑20 Exception: accident and sickness insurance business
(1) Despite section 121‑1, *health insurance business does not include the business of undertaking liability, by way of insurance, to pay a lump sum, or to make periodic payments, on the happening of a personal accident, disease or sickness.
(2) However, this section does not apply to:
(a) business where liability is undertaken with respect to loss arising out of a liability to pay fees or charges in relation to the provision in Australia of *hospital treatment or *general treatment; or
(b) business of a kind specified in the Private Health Insurance (Health Insurance Business) Rules for the purposes of this paragraph.
121‑25 Exception: liability insurance business
Despite section 121‑1, *health insurance business does not include the business of undertaking liability, by way of insurance, with respect to any loss arising out of a liability to pay compensation or damages, including:
(a) a liability to pay compensation or damages because of the use of a motor vehicle; or
(b) a liability to pay compensation or damages to an employee because of an event occurring in connection with the employee’s employment.
Despite section 121‑1, *health insurance business does not include a business of a kind that the Private Health Insurance (Health Insurance Business) Rules state not to be a health insurance business.
The Private Health Insurance Administration Council has the power, on application, to register as private health insurers bodies that are registered bodies for the purposes of the Corporations Law.
126‑5 The Private Health Insurance (Registration) Rules
Registration is also dealt with in the Private Health Insurance (Registration) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Registration) Rules are made by the Minister under section 333‑20.
126‑10 Applying for registration
(1) A body that is:
(a) a company within the meaning of the Corporations Act 2001, or a registered body within the meaning of that Act; and
(b) a *constitutional corporation;
may apply to the Council for registration as a private health insurer.
(2) The application:
(a) must be in the *approved form; and
(b) must be accompanied by a copy of the *rules according to which the applicant proposes to conduct the day‑to‑day operation of its *health insurance business (including any *health‑related business that it proposes to conduct through any of its *health benefits funds); and
(c) if the applicant is seeking to be *registered as a for profit insurer—must state that fact; and
(d) if the applicant is seeking to be registered as a *restricted access insurer—must state that fact.
(3) The applicant must also give a copy of its *rules to the Secretary of the Department.
126‑15 Requesting further information
The Council may, within 90 days after the application is made, give the applicant written notice requiring the applicant to give the Council such further information relating to the application as is specified in the notice.
126‑20 Deciding the application
(1) The Council may:
(a) grant the application, subject to such terms and conditions as the Council thinks fit; or
(b) refuse the application.
Note: Refusals of applications, and granting of applications subject to terms and conditions, are reviewable under Part 6‑9.
(2) In deciding the application, the Council must consider:
(a) whether the applicant will be able to comply with the obligations imposed by or under this Act on private health insurers; and
(b) such other matters as the Private Health Insurance (Registration) Rules require the Council to consider.
(3) In deciding the application, the Council may consider such other matters as it thinks fit, other than matters that the Private Health Insurance (Registration) Rules prohibit the Council from considering.
(4) The Council must refuse the application if the *rules of the applicant permit *improper discrimination. For the purposes of this subsection, the Council must consult the Secretary of the Department.
(5) If the Council grants the application:
(a) the applicant is taken to have been *registered as a private health insurer under this Part with effect from the date specified by the Council in granting the application (which may be a date that occurred before the application was made); and
(b) if the Council grants the application subject to terms and conditions—the registration is taken to be subject to those terms and conditions from the date on which the applicant is notified of the granting of the application; and
(c) if the applicant sought to be *registered as a for profit insurer—the registration is taken to be registration of the applicant as a for profit insurer; and
(d) if the applicant sought to be registered as a *restricted access insurer—subject to subsection (6), the registration is taken to be registration of the applicant as a restricted access insurer.
(6) The registration cannot be taken to be registration as a *restricted access insurer unless the insurer’s constitution:
(a) describes the *restricted access group to whom the insurer’s *complying health insurance products are, or will be, available; and
(b) prohibits the insurer from issuing a complying health insurance product to a person who does not belong to the group; and
(c) prohibits the insurer from ceasing to insure a person for the reason that the person has ceased to belong to the group.
(7) A restricted access group is a group of people who all belong to a particular group, based on whether they:
(a) are or were employed in a particular profession, trade, industry or calling; or
(b) are or were employed by a particular employer or by an employer who belongs to a particular class of employers; or
(c) are or were members of a particular profession, professional association or union; or
(d) are or were members of the Defence Force or part of the Defence Force; or
(e) are or were part of any group described in the Private Health Insurance (Registration) Rules.
The partners and *dependent children of people who belong to such a group are also taken to belong to that group.
(1) If the Council grants the application, the Council must:
(a) notify the applicant in writing of the grant, and of the terms and conditions (if any) to which the grant is subject; and
(b) within 7 days after granting the application, notify the Secretary in writing of the grant; and
(c) within one month after granting the application, publish in the Gazette a notification of the grant setting out:
(i) the applicant’s name; and
(ii) the date of effect of the applicant’s registration; and
(iii) the terms and conditions (if any) to which the grant is subject.
(2) If the Council refuses the application, the Council must:
(a) notify the applicant in writing of the refusal; and
(b) within 7 days after refusing the application, notify the Secretary in writing of the refusal; and
(c) within one month after refusing the application, publish in the Gazette a notification of the refusal.
126‑30 Council can be taken to refuse application
The Council is taken, for the purposes of Part 6‑9, to have refused the application if the Council does not notify the applicant of its decision on the application:
(a) within 90 days after the application was made; or
(b) within 90 days after a copy of the applicant’s *rules was given to the Secretary of the Department; or
(c) if the Council had given the applicant a notice under section 126‑15 requiring the applicant to give further information relating to the application—within 90 days after the applicant gives that information to the Council;
whichever is latest.
126‑35 Council to maintain record of registrations etc.
(1) The Council must maintain on its website an up to date record that contains:
(a) the names of all private health insurers; and
(b) in relation to each private health insurer:
(i) its address, telephone number and website address; and
(ii) the States and Territories in which it operates; and
(iii) if the insurer is registered as a *restricted access insurer—the *restricted access group to whom the insurer’s *complying health insurance products are, or will be, available.
(2) The Council must give to a person, in writing, such information from the record as the person requests.
126‑40 Changing registration status
(1) A private health insurer that:
(a) because of paragraph 126‑20(5)(c) or subsection (2) of this section, is *registered as a for profit insurer; and
(b) notifies the Council, in the *approved form, that it does not wish to be registered as a for profit insurer;
is taken, from the day after the day on which the Council receives the notice, not to be registered as a for profit insurer for the purposes of this Act.
(2) If:
(a) because of subsection (1) or otherwise, a private health insurer is not *registered as a for profit insurer; and
(b) the Council approves under section 126‑42 an application by the insurer for the insurer to convert to being registered as a for profit insurer;
the insurer is taken, from the day specified in the Council’s approval, to be registered as a for profit insurer for the purposes of this Act.
(3) If a private health insurer is taken under this section to be, or not to be, *registered as a for profit insurer, the Council must, as soon as practicable and in writing, notify accordingly:
(a) the Secretary of the Department; and
(b) the Private Health Insurance Ombudsman; and
(c) the Commissioner of Taxation.
(4) A private health insurer that:
(a) because of paragraph 126‑20(5)(d) or subsection (5) of this section, is *registered as a *restricted access insurer; and
(b) notifies the Council, in the *approved form, that it does not wish to be registered as a restricted access insurer;
is taken, from the day after the day on which the Council receives the notice, not to be registered as a restricted access insurer for the purposes of this Act.
(5) Subject to subsection 126‑20(6), a private health insurer that:
(a) because of subsection (4) or otherwise, is not *registered as a *restricted access insurer; and
(b) notifies the Council, in the *approved form, that it wishes to be registered as a restricted access insurer;
is taken, from the day after the day on which the Council receives the notice, to be registered as a restricted access insurer for the purposes of this Act.
(6) If a private health insurer is taken under this section to be, or not to be, *registered as a *restricted access insurer, the Council must, as soon as practicable and in writing, notify accordingly:
(a) the Secretary of the Department; and
(b) the Private Health Insurance Ombudsman.
126‑42 Conversion to for profit status
(1) A private health insurer may apply to the Council for approval to convert to being *registered as a for profit insurer.
(2) The application:
(a) must be in the *approved form; and
(b) must include a conversion scheme that is:
(i) in the approved form; and
(ii) accompanied by such further information as is specified in the Private Health Insurance (Registration) Rules; and
(c) must be given to the Council at least 90 days before the day specified in the application as the day on which the insurer proposes that it become *registered as a for profit insurer.
(3) The Council must approve the application if the Council is satisfied, within 30 days after the application was made, that the conversion scheme would not in substance involve the demutualisation of the insurer.
(4) If subsection (3) does not apply:
(a) the Council must, at least 45 days before the day specified in the application, cause a notice of the application to be published in a national newspaper, or in a newspaper circulating in each jurisdiction where the insurer has its registered office or carries on business; and
(b) the Council may, within 90 days after the application is made, give the insurer written notice requiring the insurer to give the Council such further information relating to the application as is specified in the notice.
(5) If subsection (3) does not apply, the Council must approve the application if:
(a) the insurer has complied with subsection (2) in relation to the application, and given to the Council such further information as the Council has required under paragraph (4)(b); and
(b) the Council is satisfied that the conversion scheme would not result in a financial benefit to any person who is not a *policy holder of, or another person insured through, a *health benefits fund conducted by the insurer; and
(c) the Council is satisfied that the conversion scheme would not result in financial benefits from the scheme being distributed inequitably between such policy holders and insured persons.
(6) The Private Health Insurance (Registration) Rules may provide for criteria for deciding, for the purposes of subsection (3), whether a conversion scheme would not in substance involve the demutualisation of the insurer.
(7) The Council must cause the insurer to be notified in writing of the Council’s decision on the application.
Note: Refusals of applications are reviewable under Part 6‑9.
126‑45 Cancellation of registration
(1) The Council must cancel the registration of a private health insurer if:
(a) the insurer has not conducted *health insurance business during the preceding 12 months; or
(b) the insurer’s *health benefits funds have been terminated under Division 149.
(2) The Council must:
(a) notify the insurer in writing of the cancellation; and
(b) within 7 days after the cancellation, notify the Secretary in writing of the cancellation; and
(c) within one month after the cancellation, publish in the Gazette a notification of the cancellation.
Part 4‑4—Health benefits funds
Private health insurers must have health benefits funds. These funds must be operated in accordance with the requirements of this Part, in particular the requirements relating to solvency and capital adequacy.
Directors of private health insurers may be personally liable if these requirements are contravened.
131‑5 The Private Health Insurance (Health Benefits Fund) Rules
*Health benefits funds are also dealt with in the Private Health Insurance (Health Benefits Fund Policy) Rules and the Private Health Insurance (Health Benefits Fund Administration) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Health Benefits Fund Policy) Rules are made by the Minister under section 333‑20, and the Private Health Insurance (Health Benefits Fund Administration) Rules are made by the Council under section 333‑25.
131‑10 Meaning of health benefits fund
A health benefits fund is a fund that:
(a) is established in the records of a private health insurer; and
(b) relates solely to:
(i) its *health insurance business, or a particular part of that business; or
(ii) its health insurance business, or a particular part of that business, and some or all of its *health‑related businesses, or particular parts of those businesses.
131‑15 Meaning of health‑related business
(1) Health‑related business is business that is any one or more of the following:
(a) a business of providing goods or services (or both) in order to manage or prevent diseases, injuries or conditions;
(b) a business of undertaking liability, by way of insurance, to indemnify people who are *ineligible for Medicare for costs associated with providing treatment, goods or services that:
(i) are provided to those people in Australia; and
(ii) are provided to manage or prevent diseases, injuries or conditions;
(c) a business of providing a financial service to assist people insured under *complying health insurance products to meet the costs associated with treatment, goods or services that are provided to manage or prevent diseases, injuries or conditions;
(d) any other business, or business included in a class of businesses, specified in the Private Health Insurance (Health Benefits Fund Policy) Rules for the purposes of this paragraph.
(2) Despite subsection (1), neither of the following is health‑related business:
(a) business that is *health insurance business; or
(b) any other business, or business included in a class of businesses, specified in the Private Health Insurance (Health Benefits Fund Policy) Rules for the purposes of this paragraph.
Division 134—The requirement to have health benefits funds
134‑1 Private health insurers must have health benefits funds
(1) A private health insurer must at all times have at least one *health benefits fund in respect of:
(a) its *health insurance business; or
(b) its health insurance business and some or all of its *health‑related businesses.
(2) A private health insurer may have more than one *health benefits fund, but must not have more than one in respect of a particular *risk equalisation jurisdiction.
(3) Despite subsection (2), a private health insurer may have more than one *health benefits fund in respect of a particular *risk equalisation jurisdiction if:
(a) each of those funds; or
(b) each of those funds, other than one such fund which was established in connection with a restructure of funds under Division 146;
is a fund that existed at the time this Act commenced, and that, immediately before that commencement, was conducted by a registered organization (within the meaning of the National Health Act 1953).
(4) Despite subsection (2), a private health insurer may have more than one *health benefits fund in respect of a particular *risk equalisation jurisdiction in the circumstances specified in the Private Health Insurance (Health Benefits Fund Policy) Rules for the purposes of this subsection.
134‑5 Notifying the Council when health benefits funds are established
(1) If a private health insurer establishes a *health benefits fund, the insurer must give to the Council written notice of:
(a) the establishment of the fund; and
(b) the date on which the fund was established; and
(c) such other matters as are specified in the Private Health Insurance (Health Benefits Fund Administration) Rules for the purposes of this paragraph.
(2) The notice must be given in the *approved form.
(3) This section does not apply if the fund is established under an approval given under Division 146.
134‑10 Inclusion of health‑related businesses in health benefits funds
(1) If a private health insurer has a *health benefits fund in respect of its *health insurance business and some or all of its *health‑related businesses, the dominant purpose of the fund must relate to its health insurance business.
(2) If the Council is satisfied that the insurer is contravening subsection (1):
(a) the Council may give to the insurer such directions relating to divesting the fund of *health‑related businesses as the Council thinks necessary to ensure the insurer’s compliance with subsection (1); and
(b) the insurer must comply with those directions.
Division 137—The operation of health benefits funds
137‑1 Assets of health benefits funds
(1) A private health insurer must keep *assets of a *health benefits fund distinct and separate from assets of other health benefits funds and from all other money, assets or investments of the insurer.
(2) A private health insurer must maintain a separate bank account for each *health benefits fund that it conducts.
(3) The assets of a *health benefits fund at a particular time are the following:
(a) the balance of money represented by amounts credited to the fund in accordance with section 137‑5;
(b) assets of the insurer obtained as a result of the expenditure or application of money credited to the fund;
(c) investments held by the insurer as a result of the expenditure or application of money credited to the fund;
(d) other money, assets or investments of the insurer transferred to the fund, whether under this Act or otherwise.
(4) Assets or investments obtained by the application of assets (other than money) of a *health benefits fund are themselves assets of the fund.
(4A) The assets of a *health benefits fund:
(a) include assets that, in accordance with a restructure or arrangement approved under Division 146, are to be assets of the fund; but
(b) do not include assets that, in accordance with such a restructure or arrangement, are no longer to be assets of the fund.
(5) Despite paragraphs (3)(b) and (c) and subsection (4), *assets or investments obtained by the expenditure of money of, or the application of other assets of, a *health benefits fund are not assets of the fund if:
(a) the private health insurer conducting the fund is *registered as a for profit insurer; and
(b) the expenditure or application was not done for the purposes of the fund.
(6) To avoid doubt, nothing in this Act is intended to constitute a private health insurer or its *directors a trustee or trustees of the *assets of the *health benefits funds of the insurer.
137‑5 Payments to health benefits funds
(1) A private health insurer must credit the following amounts to a *health benefits fund:
(a) premiums payable under policies of insurance that are *referable to the fund;
(b) amounts paid to the insurer in relation to a liability under Division 152 in relation to the fund;
(c) income from the investment of *assets of the fund;
(d) money paid to or by the insurer under a judgment of a court relating to any matter concerning the business of the fund or any failure to comply with this Part in relation to the fund;
(e) any other money received by the insurer in connection with its conduct of the business of the fund;
(f) any other amounts that the Private Health Insurance (Health Benefits Fund Policy) Rules specify.
(2) This Act does not prevent a private health insurer from *making a capital payment to a *health benefits fund.
(3) A private health insurer makes a capital payment to a *health benefits fund if it credits to the fund an amount that:
(a) is not required to be credited to the fund under subsection (1); and
(b) either:
(i) does not represent any part of the *assets of another health benefits fund; or
(ii) is credited to the fund with the Council’s written approval.
137‑10 Expenditure and application of health benefits funds
(1) A private health insurer must not apply, or deal with, *assets of a *health benefits fund, whether directly or indirectly, except in accordance with this Division.
(2) The *assets of a *health benefits fund must not be applied:
(a) for any purpose other than:
(i) meeting *policy liabilities and other liabilities, or expenses, incurred for the purposes of the business of the fund (including policy liabilities and other liabilities that are treated, in accordance with a restructure or arrangement approved under Division 146, as policy liabilities and other liabilities incurred for the purposes of the fund); or
(ii) making investments in accordance with section 137‑20; or
(iii) making a distribution under Division 149; or
(iv) a purpose specified in the Private Health Insurance (Health Benefits Fund Policy) Rules for the purposes of this subparagraph; or
(b) for a purpose specified in the Private Health Insurance (Health Benefits Fund Policy) Rules for the purposes of this paragraph.
(3) A private health insurer must not mortgage or charge any of the *assets of a *health benefits fund except:
(a) to secure a bank overdraft; or
(b) for such other purposes, and subject to such conditions, as are specified in the Private Health Insurance (Health Benefits Fund Administration) Rules for the purposes of this paragraph.
(4) A private health insurer must not borrow money for the purposes of the business of a *health benefits fund except in accordance with the Private Health Insurance (Health Benefits Fund Administration) Rules.
(5) Despite subsection (2), if a private health insurer is *registered as a for profit insurer, the *assets of a *health benefits fund conducted by the insurer may be applied for any purpose, except an application of the assets that is inconsistent with:
(a) the *solvency standard; or
(b) the *capital adequacy standard; or
(c) a *solvency direction or *capital adequacy direction given to the insurer.
(6) This section does not apply to the transfer of *assets:
(a) from one *health benefits fund to another in accordance with Division 146; or
(b) in accordance with a direction under subsection 134‑10(2).
137‑15 Effect of non‑compliance with section 137‑10
General principle
(1) A transaction entered into in contravention of section 137‑10 is of no effect unless:
(a) the Federal Court makes an order under subsection (2); or
(b) it is included in a class of transactions specified in the Private Health Insurance (Health Benefits Fund Administration) Rules to be transactions to which this section applies, and the Federal Court has not made an order under subsection (6).
Order declaring the transaction to be effective
(2) The Federal Court, on application by a party to the transaction, may make an order declaring that the transaction is effective, and is to be taken always to have been effective, for all purposes.
(3) The Federal Court must not make an order under subsection (2) unless it is satisfied that the applicant entered into the transaction in good faith and without knowledge of the contravention.
(4) In deciding whether to make an order under subsection (2), the Federal Court may have regard to any hardship that would be caused to the applicant if the order were not made.
(5) Subsection (4) is not intended to limit the matters to which the Federal Court may have regard on an application under subsection (2).
Order declaring the transaction to be of no effect
(6) The Federal Court, on application by the Council, may make an order declaring that a particular transaction that:
(a) was entered into in contravention of section 137‑10; and
(b) is included in a class of transactions of a kind referred to in paragraph (1)(b) of this section;
is, and is to be taken always to have been, of no effect for any purpose.
(7) The Federal Court must not make an order under subsection (6) if it is satisfied that the effect of the order (if made) would be to cause hardship to a person who entered into the transaction in good faith and without knowledge of the contravention.
137‑20 Investment of health benefits funds
(1) A private health insurer may invest *assets of a *health benefits fund in any way that is likely to further the business of the fund.
(2) However:
(a) nothing in this Act authorises a private health insurer to make an investment the insurer would otherwise be prohibited from making; and
(b) nothing in this Act authorises a private health insurer to make an investment the insurer would not otherwise have power to make; and
(c) a private health insurer must not invest *assets of a *health benefits fund, or keep such assets invested, if the investment, or the retention of the investment, as the case requires, is prohibited by the Private Health Insurance (Health Benefits Fund Administration) Rules.
(3) A transaction is not ineffective merely because it involves a contravention of paragraph (2)(c).
137‑25 Restriction on restructure, merger, acquisition or termination of health benefits funds
(1) A private health insurer must not change the *health benefits fund to which a policy of insurance is *referable unless the change is made in accordance with Division 146.
(2) A private health insurer must not terminate a *health benefits fund except in accordance with Division 149.
(3) This section does not prevent a liquidator doing anything authorised or required by or under this Act or any other law of the Commonwealth or of a State or Territory.
137‑30 Operation of health‑related businesses through health benefits funds
If a private health insurer has a *health benefits fund in respect of its *health insurance business and some or all of its *health‑related businesses, the insurer must comply with any requirements specified in the Private Health Insurance (Health Benefits Fund Policy) Rules relating to how the health‑related businesses are to be conducted.
Division 140—The solvency standard for health benefits funds
The purpose of this Division is to establish, and require private health insurers to comply with, standards of solvency in order to ensure that the *health benefits funds conducted by private health insurers remain solvent.
140‑5 Council to establish solvency standard
(1) The Private Health Insurance (Health Benefits Fund Administration) Rules may establish a solvency standard for the purposes of this Division.
(2) The *solvency standard may be expressed:
(a) to set different standards of solvency:
(i) for *health benefits funds conducted by different private health insurers; or
(ii) for different classes of health benefits funds; or
(b) to apply to a health benefits fund only in circumstances specified in the standard.
140‑10 Purpose of solvency standard
The purpose of the *solvency standard is to ensure, as far as practicable, that at any time the financial position of a *health benefits fund conducted by a private health insurer is such that the insurer will be able, out of the fund’s *assets, to meet all liabilities that are referable to the fund as those liabilities become due.
140‑15 Compliance with solvency standard
Private health insurers to comply with solvency standard
(1) Subject to subsection (2), every private health insurer must comply with the *solvency standard as it applies in respect of that insurer.
Declarations that solvency standard does not apply
(2) The Council may declare, by notice in writing, that the *solvency standard does not apply to a particular private health insurer. The declaration may be expressed to be limited to particular specified circumstances, or to a particular specified period, or both.
Note: Refusals to make declarations are reviewable under Part 6‑9.
Conditions applying to declarations
(3) The Council may:
(a) in a declaration under subsection (2); or
(b) by a separate notice in writing;
impose conditions to be complied with by any private health insurer that is to get the benefit of the declaration.
Note: Decisions to impose conditions are reviewable under Part 6‑9.
(4) If a private health insurer fails to comply with a condition referred to in subsection (3), the declaration is taken to cease to apply to the insurer.
Revoking or varying declarations and conditions
(5) If the Council is satisfied that a declaration under subsection (2), or a condition referred to in subsection (3), is no longer required or should be varied, the Council must, by notice in writing, revoke or vary the declaration or condition accordingly.
(6) If a private health insurer requests the Council, in writing, to revoke or vary a declaration under subsection (2), or a condition referred to in subsection (3), the Council must, within 28 days after receiving the request:
(a) if the Council is satisfied that the declaration or condition is no longer necessary or should be varied—revoke or vary the declaration or condition; or
(b) in any other case—refuse to revoke or vary the declaration or condition.
Note: Refusals to revoke or vary declarations or conditions are reviewable under Part 6‑9.
(7) If the Council does not, within the 28 days referred to in subsection (6), either revoke or vary or refuse to revoke or vary the declaration or condition concerned, the Council is to be taken, for the purposes of this Act, to have refused to revoke or vary the declaration or condition at the end of that period.
Note: Decisions that the Council is taken under this subsection to have made are reviewable under Part 6‑9.
(8) The Council must give to the private health insurer written notice of a decision made under subsection (6) and, if the Council refuses to revoke or vary the declaration or condition concerned, provide a statement of reasons for so refusing.
Declarations etc. are not legislative instruments
(9) A notice under subsection (2), (3), (5) or (8) is not a legislative instrument.
References to declarations etc.
(10) A reference in this section to a declaration or condition includes a reference to a declaration or condition as varied.
Council may give solvency directions
(1) The Council may give written directions (solvency directions) to a private health insurer if, having regard to:
(a) the nature and value of the *assets of a *health benefits fund conducted by the insurer; or
(b) the nature and extent of the liabilities that are referable to the business of the fund; or
(c) any other matters that the Council considers relevant;
the Council is satisfied that there are reasonable grounds for believing that the insurer might not be able to meet, out of the assets of the fund, all liabilities referable to the business of the fund as they become due.
(2) *Solvency directions are directions that, in the Council’s opinion, are reasonably necessary to ensure, as far as practicable, that a private health insurer will be able to meet the liabilities of a *health benefits fund conducted by the insurer out of the *assets of the fund as they become due.
(3) The Council may give a *solvency direction to a private health insurer even if, when the direction is given:
(a) the insurer meets the requirements of the *solvency standard applicable to that insurer in respect of the fund; and
(b) there are reasonable grounds to believe that the insurer will meet that standard at all times while the direction is in force.
Compliance with solvency directions
(4) A private health insurer must comply with a *solvency direction given to it under subsection (1).
Duration of solvency directions
(5) Subject to subsections (7) and (8), a *solvency direction remains in force for a period specified in the direction, not exceeding 3 years, commencing on the day when the direction is given.
(6) Subsection (5) does not prevent the Council from giving a further *solvency direction in the same terms to take effect immediately after the expiry of a previous direction.
Revoking or varying solvency directions
(7) If the Council is satisfied that a particular *solvency direction is no longer required or should be varied, the Council must, by written notice given to the private health insurer, revoke or vary the direction accordingly.
(8) If a private health insurer to which a *solvency direction has been given requests the Council, in writing, to revoke or vary the direction, the Council must, within 28 days after receiving the request:
(a) if the Council is satisfied that the direction is no longer necessary or should be varied—revoke or vary the direction; or
(b) in any other case—refuse to revoke or vary the direction.
Note: Refusals to revoke or vary solvency directions are reviewable under Part 6‑9.
(9) If the Council does not, within the 28 days referred to in subsection (8), either revoke or vary or refuse to revoke or vary the *solvency direction concerned, the Council is to be taken, for the purposes of this Act, to have refused to revoke or vary the direction at the end of that period.
Note: Decisions that the Council is taken under this subsection to have made are reviewable under Part 6‑9.
(10) The Council must give to the private health insurer written notice of a decision made under subsection (8) and, if the Council refuses to revoke or vary the *solvency direction concerned, provide a statement of reasons for refusing.
Division 143—The capital adequacy standard for health benefits funds
The purpose of this Division is to establish, and require private health insurers to comply with, a standard in order to maintain the capital adequacy of the *health benefits funds they conduct.
143‑5 Council to establish capital adequacy standard
(1) The Private Health Insurance (Health Benefits Fund Administration) Rules may establish a capital adequacy standard for the purposes of this Division.
(2) The *capital adequacy standard may be expressed:
(a) to set different standards of capital adequacy:
(i) for *health benefits funds conducted by different private health insurers; or
(ii) for different classes of health benefits funds; or
(b) to apply to a health benefits fund only in circumstances specified in the standard.
143‑10 Purpose of capital adequacy standard
The purpose of the *capital adequacy standard is to ensure, as far as practicable, that there are sufficient *assets in a *health benefits fund conducted by a private health insurer to provide adequate capital for the conduct of the fund:
(a) in accordance with this Act; and
(b) in the interests of the *policy holders of the fund.
143‑15 Compliance with capital adequacy standard
Private health insurers to comply with capital adequacy standard
(1) Subject to subsection (2), every private health insurer must comply with the *capital adequacy standard as it applies in respect of that insurer.
Declarations that capital adequacy standard does not apply
(2) The Council may declare, by notice in writing, that the *capital adequacy standard does not apply to a particular private health insurer. The declaration may be expressed to be limited to particular specified circumstances, or to a particular specified period, or both.
Note: Refusals to make declarations are reviewable under Part 6‑9.
Conditions applying to declarations
(3) The Council may:
(a) in a declaration under subsection (2); or
(b) by a separate notice in writing;
impose conditions to be complied with by any private health insurer that is to get the benefit of the declaration.
Note: Decisions to impose conditions are reviewable under Part 6‑9.
(4) If a private health insurer fails to comply with a condition referred to in subsection (3), the declaration is taken to cease to apply to the insurer.
Revoking or varying declarations and conditions
(5) If the Council is satisfied that a declaration under subsection (2), or a condition referred to in subsection (3), is no longer required or should be varied, the Council must, by notice in writing, revoke or vary the declaration or condition accordingly.
(6) If a private health insurer requests the Council, in writing, to revoke or vary a declaration under subsection (2), or a condition referred to in subsection (3), the Council must, within 28 days after receiving the request:
(a) if the Council is satisfied that the declaration or condition is no longer necessary or should be varied—revoke or vary the declaration or condition; or
(b) in any other case—refuse to revoke or vary the declaration or condition.
Note: Refusals to revoke or vary declarations or conditions are reviewable under Part 6‑9.
(7) If the Council does not, within the 28 days referred to in subsection (6), either revoke or vary or refuse to revoke or vary the declaration or condition concerned, the Council is to be taken, for the purposes of this Act, to have refused to revoke or vary the declaration or condition at the end of that period.
Note: Decisions that the Council is taken under this subsection to have made are reviewable under Part 6‑9.
(8) The Council must give to the private health insurer written notice of a decision made under subsection (6) and, if the Council refuses to revoke or vary the declaration or condition concerned, provide a statement of reasons for so refusing.
Declarations etc. are not legislative instruments
(9) A notice under subsection (2), (3), (5) or (8) is not a legislative instrument.
References to declarations etc.
(10) A reference in this section to a declaration or condition includes a reference to a declaration or condition as varied.
143‑20 Capital adequacy directions
Council may give capital adequacy directions
(1) The Council may give written directions (capital adequacy directions) to a private health insurer if, having regard to:
(a) the nature and value of the *assets of a *health benefits fund conducted by the insurer; or
(b) the nature and extent of the liabilities that are referable to the business of the fund; or
(c) any other matters that the Council considers relevant;
the Council is satisfied that there are reasonable grounds for believing that the assets of the fund will not provide adequate capital for the conduct of the business of the fund in accordance with this Act and in the interests of the *policy holders of the fund.
(2) *Capital adequacy directions are directions that, in the Council’s opinion, are reasonably necessary to ensure, as far as practicable, that *assets of a *health benefits fund conducted by a private health insurer will provide adequate capital for the purposes described in subsection (1).
(3) The Council may give a *capital adequacy direction to a private health insurer even if, when the direction is given:
(a) the insurer meets the requirements of the *capital adequacy standard applicable to that insurer in respect of the fund; and
(b) there are reasonable grounds to believe that the insurer will meet that standard at all times while the direction is in force.
Compliance with capital adequacy directions
(4) A private health insurer must comply with a *capital adequacy direction given to it under subsection (1).
Duration of capital adequacy directions
(5) Subject to subsections (7) and (8), a *capital adequacy direction remains in force for a period specified in the direction, not exceeding 3 years, commencing on the day when the direction is given.
(6) Subsection (5) does not prevent the Council from giving a further *capital adequacy direction in the same terms to take effect immediately after the expiry of a previous direction.
Revoking or varying capital adequacy directions
(7) If the Council is satisfied that a particular *capital adequacy direction is no longer required or should be varied, the Council must, by written notice given to the private health insurer, revoke or vary the direction accordingly.
(8) If a private health insurer to which a *capital adequacy direction has been given requests the Council, in writing, to revoke or vary the direction, the Council must, within 28 days after receiving the request:
(a) if the Council is satisfied that the direction is no longer necessary or should be varied—revoke or vary the direction; or
(b) in any other case—refuse to revoke or vary the direction.
Note: Refusals to revoke or vary capital adequacy directions are reviewable under Part 6‑9.
(9) If the Council does not, within the 28 days referred to in subsection (8), either revoke or vary or refuse to revoke or vary the *capital adequacy direction concerned, the Council is to be taken, for the purposes of this Act, to have refused to revoke or vary the direction at the end of that period.
Note: Decisions that the Council is taken under this subsection to have made are reviewable under Part 6‑9.
(10) The Council must give to the private health insurer written notice of a decision made under subsection (8) and, if the Council refuses to revoke or vary the *capital adequacy direction concerned, provide a statement of reasons for so refusing.
Division 146—Restructure, merger and acquisition of health benefits funds
146‑1 Restructure of health benefits funds
(1) A private health insurer may restructure its *health benefits funds so that insurance policies that are *referable to a health benefits fund (a transferring fund) of the insurer become referable to one or more other health benefits funds (receiving funds) of the insurer (whether existing or proposed) if:
(a) the insurance policies concerned are all of the policies that, immediately before the restructure, were referable to the transferring fund and belonged to one or more *policy groups of that fund; and
(b) the insurer applies to the Council, in the *approved form, for approval of the restructure; and
(c) the Council approves the restructure in writing; and
(d) the insurer complies with any requirements that the Private Health Insurance (Health Benefits Fund Administration) Rules impose on the insurer in relation to the restructure.
(2) Subject to subsection (3), the Council must approve the restructure if, and only if, it is satisfied that:
(a) the *assets and liabilities that would be transferred to the receiving fund or funds represent a reasonable estimate of what would, immediately before the restructure, be the *net asset position of the transferring fund; and
(aa) if there is more than one receiving fund—those assets and liabilities would be fairly distributed between the receiving funds; and
(b) the restructure will not result in any breach of the *solvency standard or the *capital adequacy standard.
(2A) For the purposes of paragraph (2)(a), in working out the *net asset position of the transferring fund, disregard the net asset position of the fund to the extent that it relates to insurance policies that do not belong to a *policy group referred to in paragraph (1)(a).
(3) The Council must not approve the application if:
(a) it considers that the restructure will result in unfairness to the *policy holders of a *health benefits fund of the insurer as that fund exists immediately before the restructure, when those policy holders are viewed as a group; or
(b) it considers that the restructure will result in unfairness to the persons who would be policy holders of a health benefits fund of the insurer as that fund would exist immediately after the restructure, when those persons are viewed as a group; or
(c) the insurer is being wound up when the application is made.
Note: Refusals to approve restructures are reviewable under Part 6‑9.
(4) The Private Health Insurance (Health Benefits Fund Administration) Rules may provide for the following:
(a) criteria for approving or refusing to approve applications under subsection (1);
(aa) how to work out reasonable estimates of the kind referred to in paragraph (2)(a);
(ab) criteria for deciding, for the purposes of paragraph (2)(aa), whether assets and liabilities would be fairly distributed;
(b) requirements to notify interested persons of the outcomes of such applications;
(c) matters connected with how restructures take place, including the following:
(i) insurance policies becoming *referable to a receiving fund or funds;
(ii) *policy liabilities and other liabilities incurred for the purposes of a transferring fund becoming treated as policy liabilities and other liabilities incurred for the purposes of a receiving fund or funds;
(iii) *assets of a transferring fund becoming assets of a receiving fund or funds;
(iv) the timing of restructures;
(v) if a receiving fund is a proposed new *health benefits fund—the establishment of that fund;
(d) requirements for private health insurers to give the Council information following restructures.
(5) A policy group, of a *health benefits fund, is all of the insurance policies:
(a) that are *referable to the fund; and
(b) the addresses of the *holders of which, as known to the private health insurer conducting the fund, are located in the same *risk equalisation jurisdiction.
The Private Health Insurance (Health Benefits Fund Administration) Rules may provide for how to work out the policy group for a policy that has 2 or more holders whose addresses are not all located in the same risk equalisation jurisdiction.
(6) An area is a risk equalisation jurisdiction if the Private Health Insurance (Health Benefits Fund Administration) Rules so provide.
146‑5 Merger and acquisition of health benefits funds
(1) A private health insurer (the transferee insurer) may enter into an arrangement with one or more other private health insurers (transferor insurers) under which:
(a) insurance policies that are *referable to a *health benefits fund or funds (transferring funds) of the transferor insurer or transferor insurers become referable to a health benefits fund or funds (receiving funds) of the transferee insurer; and
(b) in relation to each of the transferring funds, the insurance policies concerned are:
(i) all of the insurance policies that are referable to the transferring fund; or
(ii) all of the insurance policies that are referable to the transferring fund and that belong to one or more *policy groups of the fund.
(2) However, the arrangement must not take effect unless:
(a) the insurers referred to in subsection (1) apply jointly to the Council, in the *approved form, for approval of the arrangement; and
(b) the Council approves the arrangement in writing; and
(c) the insurers comply with any requirements that the Private Health Insurance (Health Benefits Fund Administration) Rules impose on the insurers in relation to the arrangement.
(3) The Council must approve the arrangement if, and only if, it is satisfied that:
(a) the *assets and liabilities that would be transferred, under the arrangement, to the receiving fund or funds represent a reasonable estimate of what would, immediately before the restructure, be:
(i) if there is only one transferring fund—the *net asset position of the fund; or
(ii) if there is more than one transferring fund—the sum of the net asset positions of each of the funds; and
(b) if, under the arrangement, there would be more than one receiving fund—those assets and liabilities would be fairly distributed between the receiving funds; and
(c) if subparagraph (1)(b)(i) applies to any transferring fund—the net asset position of the fund immediately after the arrangement takes effect will not be greater than zero; and
(d) the arrangement will not result in any breach of the *solvency standard or the *capital adequacy standard if it takes effect.
Note: Refusals to approve transfers are reviewable under Part 6‑9.
(4) For the purposes of paragraph (3)(a), in working out the *net asset position of a transferring fund to which subparagraph (1)(b)(ii) applies, disregard the net asset position of the fund to the extent that it relates to insurance policies that do not belong to a *policy group referred to in that subparagraph.
(5) The Private Health Insurance (Health Benefits Fund Administration) Rules may provide for the following:
(a) criteria for approving or refusing to approve applications under this section;
(b) how to work out reasonable estimates of the kind referred to in paragraph (3)(a);
(c) criteria for deciding, for the purposes of paragraph (3)(b), whether assets and liabilities would be fairly distributed;
(d) requirements to notify interested persons of the outcomes of such applications;
(e) matters connected with how arrangements take effect, including the following:
(i) insurance policies becoming *referable to a *health benefits fund or funds of the transferee insurer;
(ii) *policy liabilities and other liabilities incurred for the purposes of a health benefits fund or funds of a transferor insurer becoming treated as policy liabilities and other liabilities incurred for the purposes of a health benefits fund or funds of the transferee insurer;
(iii) *assets of a health benefits fund or funds of a transferor insurer becoming assets of a health benefits fund or funds of the transferee insurer;
(iv) the timing of arrangements;
(f) requirements for private health insurers to give the Council information following arrangements taking effect.
(6) The transferee insurer must, within 28 days after the arrangement takes effect, notify the Council of the arrangement. The notice must comply with any requirements specified in the Private Health Insurance (Health Benefits Fund Administration) Rules.
(7) For the purposes of this Act, an insurance policy that becomes *referable to a *health benefits fund of the transferee insurer as a result of the arrangement is treated, after the arrangement takes effect, as if it were an insurance policy issued by the transferee insurer.
146‑10 Consent of policy holders not required
The consent of the *policy holders of a *health benefits fund is not required for any:
(a) restructuring health benefits funds as provided for in section 146‑1; or
(b) entering into arrangements of a kind referred to in section 146‑5, or implementing such arrangements;
unless the constitution of the private health insurer conducting the fund provides otherwise.
146‑15 Other laws not overridden
This Division does not affect the operation of any other law of the Commonwealth, a State or a Territory in relation to:
(a) restructuring *health benefits funds as provided for in section 146‑1; or
(b) entering into arrangements of a kind referred to in section 146‑5, or implementing such arrangements.
Division 149—Termination of health benefits funds
Subdivision 149‑A—Approving the termination of health benefits funds
149‑1 Applying for termination
A private health insurer may apply to the Council, in the *approved form, for approval of the termination of each of its *health benefits funds.
149‑5 Requesting further information
The Council may, within 28 days after the application is made, give the applicant written notice requiring the applicant to give the Council such further information relating to the application as is specified in the notice.
149‑10 Deciding the application
(1) The Council must approve the termination if it is satisfied that:
(a) the insurer is not in the process of being wound up; and
(b) each of its *health benefits funds meets the *solvency standard; and
(c) in relation to each of the funds, termination of the fund will not result in unfairness to the *policy holders of the fund, when those policy holders are viewed as a group;
and is satisfied as to such other matters as are specified in the Private Health Insurance (Health Benefits Fund Policy) Rules.
(2) If the Council grants the application, the Council:
(a) may appoint a person other than the applicant as the *terminating manager of the funds; and
(b) must notify the insurer in writing:
(i) that it approves the termination; and
(ii) if paragraph (a) applies—of the appointment of the terminating manager.
(3) If the Council refuses the application, the Council must notify the insurer in writing of the refusal.
Note: Refusals to approve terminations are reviewable under Part 6‑9.
149‑15 Council can be taken to refuse application
The Council is taken, for the purposes of Part 6‑9, to have refused the application if the Council does not notify the applicant of its decision on the application:
(a) within 90 days after the application was made; or
(b) if the Council had given the applicant a notice under section 149‑5 requiring the applicant to give further information relating to the application—within 90 days after the applicant gives that information to the Council;
whichever is later.
Subdivision 149‑B—Conducting the termination of health benefits funds
149‑20 Conduct of funds during termination process
(1) A private health insurer must not, after being notified under subsection 149‑10(2) that termination of its *health benefits funds has been approved:
(a) enter into an insurance policy that is *referable to any of its funds with a person who is not already a *holder of such a policy; or
(b) if the insurer is *registered as a for profit insurer—apply the *assets of any of the funds except in accordance with subsection 137‑10(2) (unless this paragraph has ceased to apply to the insurer because of section 149‑45); or
(c) if the insurer is not registered as a for profit insurer—become registered as a for profit insurer.
(2) The insurer must, within 60 days after being notified under subsection 149‑10(2) that termination of its *health benefits funds has been approved:
(a) give a written notice, stating the day (the termination day) from which it will not renew insurance policies that are *referable to any of its funds, to:
(i) each *policy holder of any of its funds; and
(ii) the Council; and
(b) notify the termination day in a national newspaper, or in a newspaper circulating in each jurisdiction where the insurer has its registered office or carries on business.
The termination day must not be earlier than 90 days after the insurer finishes giving notices under this subsection.
(3) The insurer must not, on or after the *termination day, renew any insurance policies that are *referable to any of those funds.
(4) The insurer must accept any valid claim for benefits under an insurance policy that is or was *referable to any of those funds if the claim is made before the end of the period of 12 months following the expiry of the last policy that was referable to any of those funds.
149‑25 Insurers etc. to give reports to Council
If the Council has approved the termination of the *health benefits funds of a private health insurer:
(a) the insurer; or
(b) if a *terminating manager of the funds has been appointed—the terminating manager;
must, within 28 days after the end of the *termination day, make a written report to the Council setting out details of the *assets and liabilities of each of the funds as at that day.
149‑30 Terminating managers displace management of funds
If a *terminating manager of the *health benefits funds of a private health insurer has been appointed, then, for so long as the appointment is in force and until the termination is completed:
(a) the management of the fund vests in the terminating manager; and
(b) any *officer of the *responsible insurer for the fund who was vested with the management of the fund immediately before the appointment is, by force of this section, divested of that management.
Subdivision 149‑C—Ending the termination of health benefits funds
149‑35 Power to end termination
(1) At any time during the termination of the *health benefits funds of a private health insurer, the Federal Court may, on application, make an order ending the termination on a day specified in the order.
(2) An application may be made by:
(a) the Council; or
(b) the *terminating manager.
(3) On such an application, the Federal Court may, before making an order, direct the *terminating manager to give a report with respect to a relevant fact or matter.
(4) If the Federal Court has made an order ending the termination, the Court may give such directions as it thinks fit for the resumption of the management and control of the *health benefits funds of the private health insurer by its *officers.
Subdivision 149‑D—Completing the termination of health benefits funds
149‑40 Completion of the termination process
The termination of the *health benefits funds of a private health insurer is completed if:
(a) the period of 12 months referred to in subsection 149‑20(4) has come to an end; and
(b) so far as possible having regard to the extent of the *assets of the funds:
(i) the liabilities of the funds to the *policy holders of the funds have been discharged; and
(ii) any amounts of *collapsed insurer levy that the Council has paid, for the purposes of any of the funds, to the insurer or to the person appointed to administer the termination of the funds have been repaid to the Council; and
(iii) any other liabilities of the funds have been discharged.
149‑45 Distribution of remaining assets after completion of the termination process
If the termination of the funds is completed and, on the completion, there are *assets of those funds, then:
(a) if the insurer is *registered as a for profit insurer—paragraph 149‑20(1)(b) ceases to apply to the insurer; or
(b) if the insurer is not registered as a for profit insurer—the insurer is liable to pay to the Council an amount equal to the value of those assets.
149‑50 Liability of officers of insurers for loss to terminated funds
(1) If:
(a) a private health insurer contravenes this Act in relation to a *health benefits fund that it conducts; and
(b) the contravention results in a loss to the fund; and
(c) the termination of the fund is completed;
the persons who were *officers of the insurer when the contravention occurred are jointly and severally liable to pay to the Council, for payment to the *Risk Equalisation Trust Fund, an amount equal to the amount of the loss.
(2) A person is not liable under subsection (1) if the person proves that he or she used due diligence to prevent the occurrence of such a contravention.
(3) On application by the Council, the Federal Court may order any person liable under subsection (1) to pay to the Council, for payment to the *Risk Equalisation Trust Fund, the whole or any part of the loss.
149‑55 Report of terminating manager
(1) The *terminating manager may, at any time, make a written report to the Council on the termination of the *health benefits funds of a private health insurer, and must make such a report as soon as practicable after the termination of the funds.
(2) The report may include a recommendation that an application be made under section 149‑60 for the winding up of the insurer.
149‑60 Applying for winding up
(1) If the *terminating manager’s report under section 149‑55 includes a recommendation that an application be made under this section for the winding up of a private health insurer, the Council, or the terminating manager, may apply to the Federal Court for an order that the insurer be wound up.
(2) However, the *terminating manager must not apply unless directed by the Council to apply.
(2A) On an application under subsection (1), the Federal Court may make an order that the insurer be wound up if the Court is satisfied that it is in the financial interests of the *policy holders of the *health benefits funds conducted by the insurer that such an order be made.
(3) The winding up of the insurer is to be conducted in accordance with the Corporations Act 2001.
Division 152—Duties and liabilities of directors etc.
152‑5 Notices to remedy contraventions
(1) If a private health insurer has contravened this Part, the Council may give the insurer a written notice requiring the insurer, within a specified period, to take such action as is specified in the notice to remedy the contravention.
(2) The period specified in the notice must be a period ending not earlier than one month after the giving of the notice.
(3) The action to be specified in the notice is such action as the Council thinks appropriate and reasonable to overcome the effects of the contravention.
(4) At any time before the end of the period specified in the notice, the Council may extend the period by such further period as the Council thinks fit.
(5) The insurer must comply with the notice.
152‑10 Liability of directors in relation to non‑compliance with notices
(1) If:
(a) the Council has given a notice to a private health insurer under section 152‑5 in respect of a contravention of this Part; and
(b) the contravention has resulted in a loss to a *health benefits fund; and
(c) the insurer has failed to comply with the notice within the period specified in it or within that period as extended under subsection 152‑5(4);
the persons who were the *directors of the insurer when the contravention occurred are jointly and severally liable to pay the insurer an amount equal to the amount of the loss.
(2) A person is not liable under subsection (1) if the person proves that he or she used due diligence to ensure that the insurer complied with the notice.
(3) An action to recover an amount for which a person is liable under subsection (1) may be brought:
(a) by the insurer; or
(b) with the written approval of the Council, by a *policy holder of the *health benefits fund involved.
(4) An approval under subsection (3) may be given subject to conditions relating to the persons, or the number of persons, who may join in the action as plaintiffs.
152‑15 Council may sue in the name of private health insurers
If the Council thinks that it is in the interests of the *policy holders of a *health benefits fund to do so, the Council may bring an action against a person in the name, and for the benefit, of a private health insurer for the recovery of an amount that the insurer is entitled to recover under this Division.
Part 4‑5—Other obligations of private health insurers
In addition to the obligations about health benefits funds, private health insurers have several other obligations relating to the conduct of their businesses. These include the following:
(a) having appointed actuaries;
(b) complying with prudential standards;
(c) exclusion of disqualified persons from management;
(d) reporting and notification obligations.
157‑5 The Private Health Insurance (Insurer Obligations) Rules
Obligations of private health insurers are also dealt with in the Private Health Insurance (Insurer Obligations) Rules and the Private Health Insurance (Data Provision) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Insurer Obligations) Rules are made by the Council under section 333‑25. The Private Health Insurance (Data Provision) Rules are made by the Minister under section 333‑20.
Division 160—Appointed actuaries
(1) Subject to subsection (2), a private health insurer must have an actuary appointed by the insurer.
(2) Within 6 weeks after a person ceases to be the *appointed actuary of a private health insurer, the insurer must appoint another person to be the insurer’s actuary.
(3) A person must not hold an appointment as actuary of a private health insurer unless the person is eligible for such an appointment.
(4) A private health insurer may, in writing, ask the Council to approve the appointment of a specified person as the insurer’s actuary.
(5) The Council may, in writing, approve the appointment of a person as actuary of a private health insurer if the Council is satisfied that the person has actuarial qualifications and experience that fit him or her to perform the functions of the insurer’s *appointed actuary.
Note: Refusals to give approval are reviewable under Part 6‑9.
(6) An appointment of a person as actuary of a private health insurer cannot take effect while there is in force an appointment of another person as the insurer’s actuary.
160‑5 Eligibility for appointment
(1) A person is eligible for appointment as a private health insurer’s actuary if the person meets the eligibility requirements specified in the Private Health Insurance (Insurer Obligations) Rules.
(2) However, a person who, apart from this subsection, would be eligible for appointment as a private health insurer’s actuary is not so eligible if there is in force a declaration by the Council in accordance with the Private Health Insurance (Insurer Obligations) Rules.
160‑10 Notification of appointment etc.
A private health insurer must give the Council written notice in accordance with the Private Health Insurance (Insurer Obligations) Rules if:
(a) the insurer appoints a person under section 160‑1; or
(b) a person ceases to be the *appointed actuary of the insurer.
160‑15 Cessation of appointment
A person ceases to hold an appointment as the actuary of a private health insurer in the circumstances set out in the Private Health Insurance (Insurer Obligations) Rules.
160‑20 Compliance with the Private Health Insurance (Insurer Obligations) Rules
The *appointed actuary of a private health insurer, in the performance of his or her duties and the exercise of his or her powers, must comply with the Private Health Insurance (Insurer Obligations) Rules.
160‑25 Powers of appointed actuary
(1) The *appointed actuary of a private health insurer is entitled to have access to any information or document in the possession, or under the control, of the insurer if the access is reasonably necessary for the proper performance of the actuary’s functions and duties.
(2) The *appointed actuary of a private health insurer may require any *officer or employee of the insurer to answer questions or produce documents for the purpose of enabling the actuary to have the access to information and documents provided for by subsection (1).
(3) A private health insurer commits an offence if the insurer refuses or fails to allow access to information or a document under subsection (1).
Penalty: 30 penalty units.
(4) An *officer or employee of a private health insurer commits an offence if he or she refuses or fails to comply with a requirement under subsection (2).
Penalty: 30 penalty units.
(5) The *appointed actuary of a private health insurer is entitled to attend a meeting of the *directors of the insurer and to speak on any matter being considered at the meeting:
(a) that relates to, or may affect:
(i) the solvency of a *health benefits fund conducted by the insurer; or
(ii) the adequacy of the capital of a health benefits fund conducted by the insurer; or
(b) that relates to advice given by the actuary to the directors; or
(c) that concerns a matter in relation to which the actuary will be required to give advice.
(6) The *appointed actuary of a private health insurer is entitled to attend:
(a) any annual general meeting of members of the insurer; and
(b) any other meeting of members of the insurer at which:
(i) the insurer’s annual accounts or financial statements are to be considered; or
(ii) any matter in connection with which the actuary is or has been subject to a duty under this Act is to be considered.
160‑30 Actuary’s obligations to report
(1) The *appointed actuary of a private health insurer must draw to the attention of the insurer, or of the *directors or an *officer of the insurer, any matter that comes to the attention of the actuary and that the actuary thinks requires action to be taken by the company or its directors to avoid a contravention of this Act.
(2) If the *appointed actuary of a private health insurer thinks:
(a) that there are reasonable grounds for believing that the insurer or a *director of the insurer may have contravened this Act or any other law; and
(b) that the contravention is of such a nature that it may affect significantly the interests of *policy holders of any *health benefits funds conducted by the insurer;
the actuary must inform the Council in writing of his or her opinion and of the information on which it is based.
(3) If:
(a) the *appointed actuary of a private health insurer has drawn to the attention of the insurer, or of the *directors or an *officer of the insurer, a matter that the actuary thinks requires action to be taken by the insurer or its directors to avoid a contravention of this Act; and
(b) the actuary is satisfied that there has been reasonable time for the taking of the action but the action has not been taken;
the actuary must inform the Council in writing of the matter.
(4) If the *appointed actuary of a private health insurer thinks that:
(a) the *directors of the insurer have failed to take such action as is reasonably necessary to enable the actuary to exercise his or her right under subsection 160‑25(5) or (6); or
(b) an *officer or employee of the insurer has engaged in conduct calculated to prevent the actuary exercising his or her right under subsection 160‑25(5) or (6);
the actuary may inform the Council of his or her opinion and of the information on which it is based.
(5) If:
(a) a person becomes subject to an obligation under subsection (2) or (3) to inform the Council of anything; and
(b) before the person informs the Council, the person ceases to be the *appointed actuary of the private health insurer concerned;
the person remains subject to the obligation as if he or she were still the appointed actuary of the insurer.
160‑35 Qualified privilege of appointed actuary
(1) A person who is, or has been, the *appointed actuary of a private health insurer has qualified privilege in respect of any statement, whether written or oral, made by him or her for the purpose of the performance of his or her functions as appointed actuary of the insurer.
(2) In particular (and without limiting subsection (1)), a person who is or has been the *appointed actuary of a private health insurer has qualified privilege in respect of:
(a) any statement, written or oral, made by him or her under, or for the purposes of, a provision of this Act; and
(b) the answer to any question he or she is required by the insurer to answer.
(3) The privilege conferred by this section is in addition to any privilege conferred on a person by any other law.
Division 163—Prudential standards
163‑1 Private Health Insurance (Insurer Obligations) Rules to establish prudential standards
(1) The Private Health Insurance (Insurer Obligations) Rules may establish prudential standards relating to *prudential matters for private health insurers.
(2) Prudential matters are matters relating to:
(a) the conduct by private health insurers of any of their affairs in such a way as:
(i) to keep themselves in a sound financial position; or
(ii) not to cause or promote instability in the Australian private health insurance system; or
(b) the conduct by private health insurers of any of their affairs with integrity, prudence and professional skill;
but does not include matters relating to the solvency or capital adequacy of *health benefits funds.
(3) A *prudential standard may impose different requirements to be complied with:
(a) by different classes of private health insurers; or
(b) in different situations; or
(c) in respect of different activities.
(4) A *prudential standard may provide for the Council to exercise powers and discretions under the standard, including but not limited to discretions to approve, impose, adjust or exclude specific prudential requirements in relation to a particular private health insurer or a particular class of private health insurers.
(5) A *prudential standard takes effect on the day on which it is established in the Private Health Insurance (Insurer Obligations) Rules, or on such later day as is specified in the Private Health Insurance (Insurer Obligations) Rules.
163‑5 Compliance with prudential standards
Every private health insurer must comply with the *prudential standards as they apply in respect of that insurer.
163‑10 Notice of breaches of prudential standards etc.
(1) A private health insurer commits an offence if:
(a) it becomes aware of:
(i) a breach by it of a *prudential standard; or
(ii) any other matter or occurrence that materially affects its financial position; and
(b) it fails to notify the Council, as soon as practicable, in writing of the breach or of the other matter or occurrence.
Penalty: 200 penalty units.
(2) If an individual:
(a) commits an offence against subsection (1) because of Part 2.4 of the Criminal Code (extensions of criminal responsibility); or
(b) commits an offence under Part 2.4 of the Criminal Code in relation to an offence against subsection (1);
he or she is punishable, on conviction, by a fine not exceeding 40 penalty units.
(3) A notification given to the Council of a matter referred to in paragraph (1)(a) must not include *personal information relating to a person insured under a *complying health insurance product that is *referable to a *health benefits fund conducted by the insurer, unless the information relates to *prudential matters relating to the insurer.
163‑15 Directions to comply with standards
(1) If the Council is satisfied that a private health insurer:
(a) has breached a *prudential standard; or
(b) is likely to breach a prudential standard in a way that is likely to give rise to a prudential risk;
the Council may (in writing) direct the insurer to comply with all or a part of the standard, or to take specified action, within a specified time.
Note: Decisions to give directions are reviewable under Part 6‑9.
(2) The insurer must comply with the direction despite anything in its constitution or in any contract or arrangement to which it is a party.
(3) The Council may revoke a direction that the Council considers is no longer necessary or appropriate by giving written notice to the insurer.
Note: Refusals to revoke directions are reviewable under Part 6‑9.
163‑20 Failure to comply with directions
(1) A private health insurer commits an offence if the insurer contravenes a direction given to it under section 163‑15.
Penalty: 300 penalty units.
(2) If an individual:
(a) commits an offence against subsection (1) because of Part 2.4 of the Criminal Code (extensions of criminal responsibility); or
(b) commits an offence under Part 2.4 of the Criminal Code in relation to an offence against subsection (1);
he or she is punishable, on conviction, by a fine not exceeding 60 penalty units.
Division 166—Disqualified persons
166‑1 Private health insurers not to allow disqualified persons to act as directors
(1) A private health insurer commits an offence if the insurer allows a *disqualified person to be or to act as a *director or *senior manager of the insurer.
Penalty: 250 penalty units.
(2) Subsection (1) does not apply if the insurer:
(a) contacted the Council within a reasonable period before allowing the person to be to or act as a *director or *senior manager, as the case may be; and
(b) was advised by the Council that the person was not a *disqualified person.
Note: A defendant bears an evidential burden in relation to the matters in this subsection. See subsection 13.3(3) of the Criminal Code.
166‑5 Disqualified persons must not act for private health insurers
A *disqualified person commits an offence if he or she is, or acts as, a *director or *senior manager of a private health insurer.
Penalty: 120 penalty units or imprisonment for 2 years, or both.
166‑10 Effect of non‑compliance
A failure to comply with section 166‑1 or 166‑5 does not affect the validity of an appointment or transaction.
166‑15 Who is a disqualified person?
(1) A person is a disqualified person if, at any time:
(a) the person has been convicted of an offence against or arising out of:
(i) this Act; or
(ii) the Corporations Act 2001, the Corporations Law that was previously in force, or any law of a foreign country that corresponds to that Act or to that Corporations Law; or
(b) the person has been convicted of an offence against or arising out of a law in force in Australia, or the law of a foreign country, if the offence concerns dishonest conduct or conduct relating to a financial sector company (within the meaning of the Financial Sector (Shareholdings) Act 1998); or
(c) the person has been or becomes bankrupt; or
(d) the person has applied to take the benefit of a law for the relief of bankrupt or insolvent debtors; or
(e) the person has compounded with his or her creditors; or
(f) the Council has disqualified the person under section 166‑20.
Note: The Council may determine that a person is not a disqualified person (see section 166‑25).
(2) A reference in subsection (1) to a person who has been convicted of an offence includes a reference to a person in respect of whom an order has been made relating to the offence under:
(a) section 19B of the Crimes Act 1914; or
(b) a corresponding provision of a law of a State, a Territory or a foreign country.
(3) Nothing in this section affects the operation of Part VIIC of the Crimes Act 1914 (which includes provisions that, in certain circumstances, relieve persons from the requirement to disclose spent convictions and require persons aware of such convictions to disregard them).
166‑20 Council may disqualify persons
(1) The Council may disqualify a person if it is satisfied that the person is not a fit and proper person to be or to act as a *director or *senior manager of a private health insurer.
Note: Disqualifications are reviewable under Part 6‑9.
(2) A disqualification takes effect on the day on which it is made.
(3) The Council may revoke a disqualification on application by the *disqualified person or on its own initiative. A revocation takes effect on the day on which it is made.
Note: Refusals to revoke disqualifications are reviewable under Part 6‑9.
(4) The Council must give the person written notice of a disqualification, revocation of a disqualification or a refusal to revoke a disqualification.
(5) As soon as practicable after a notice is given to a person under subsection (4), the Council must cause particulars of the disqualification, revocation or refusal to which the notice relates:
(a) if the person is, or is acting as, a *director or *senior manager of a private health insurer—to be given to the insurer; and
(b) to be published in the Gazette.
166‑25 Council may determine that persons are not disqualified
(1) Despite section 166‑15, the Council may determine (in writing) that a person is not a *disqualified person. The Council may do so on its own initiative or on the application of the person.
(2) However, the Council must not make the determination unless it is satisfied that the person is highly unlikely to be a prudential risk to any private health insurer.
(3) If a person applies for a determination under this section, the Council must:
(a) either make, or refuse to make, the determination; and
(b) in the case of a refusal, give the person written notice of the refusal.
Note: Refusals to make determinations are reviewable under Part 6‑9.
(4) The Council may do any of the following:
(a) when making a determination under subsection (1), specify in the determination conditions to which the determination is to be subject;
(b) at any later time while a determination under subsection (1) is in force, make a further determination specifying conditions or additional conditions to which the determination under subsection (1) is to be subject;
(c) at any time make a determination varying or revoking conditions that have been specified under paragraph (a) or (b).
Note: Decisions to specify, or to vary, conditions are reviewable under Part 6‑9.
(5) A determination takes effect on the day on which it is made.
(6) The Council must, as soon as practicable after a determination is made, give written notice of the making of the determination, and a copy of the determination, to the person concerned and to any affected private health insurer.
(7) A notice of a refusal to make a determination, or a notice of the making of a determination that specifies or varies conditions, must state the reasons for the refusal or for the specifying or variation of the conditions, as the case may be.
(8) The Council may revoke a determination under this section by giving written notice to the person concerned and must give a copy of the notice to any affected private health insurer.
Note: Revocations of determinations are reviewable under Part 6‑9.
Division 169—Reporting and notification requirements
169‑1 Copies of reports to policy holders
A private health insurer that makes any report to all or any of the *policy holders of a *health benefits fund conducted by the insurer must, if the Private Health Insurance (Insurer Obligations) Rules so require, give a copy of the report to the Council:
(a) within one month after making the report; or
(b) within such further time as the Council allows.
169‑5 Information to be given to the Council annually
(1) A private health insurer must, within 3 months after the end of each financial year, or within such further time as the Council allows, give to the Council:
(a) such financial accounts and statements in respect of that year as the Council requires to be given for use in preparing the report referred to in section 264‑15; and
(b) such other statements in respect of that year as are required by the Private Health Insurance (Insurer Obligations) Rules.
(2) Any such accounts or statements must be certified on behalf of the insurer, in accordance with the Private Health Insurance (Insurer Obligations) Rules, to be true and correct.
(3) A private health insurer commits an offence if the insurer fails to comply with this section.
Penalty: 30 penalty units.
(4) Strict liability applies to subsection (3).
Note: For strict liability, see section 6.1 of the Criminal Code.
169‑10 Private health insurers to notify any changes to rules
(1) A private health insurer that proposes to change its *rules (other than a change to which section 66‑10 applies) must notify the Secretary of the Department of the proposed change:
(a) in the *approved form; and
(b) before the day on which the insurer proposes the change to take effect.
Note: See section 93‑25 for a private health insurer’s obligation to notify insured persons of changes to its rules.
(2) The Minister may, in writing, direct the insurer not to make the change if the Minister is satisfied that the change might or would result in a breach of the Act.
Note: Directions are reviewable under Part 6‑9.
(3) The Minister must give the Secretary and the Council a copy of a direction under subsection (2).
(1) An applicant for registration under Division 126 must, before starting to operate its *health insurance business, notify the name and contact details of its *chief executive officer to the Secretary of the Department, and to the Council, in the *approved form.
(2) A private health insurer must ensure that, if the name or contact details of its *chief executive officer change, the change is notified, not more than 28 days after the change takes effect, to the Secretary of the Department, and to the Council, in the *approved form.
(3) A private health insurer commits an offence if:
(a) the insurer is required under subsection (2) to ensure that a particular thing happens; and
(b) the thing does not happen.
Penalty: 60 penalty units.
(4) Strict liability applies to subsection (3).
Note: For strict liability, see section 6.1 of the Criminal Code.
172‑1 Private health insurers to comply with Council’s requirements
A private health insurer must comply, within a reasonable time, with such requirements as the Council, in the performance of its functions, imposes on the insurer.
172-5 Agreements with medical practitioners
Medical purchaser-provider agreements
(1) If a private health insurer enters into an agreement with a *medical practitioner for the provision of treatment to persons insured by the insurer, the agreement must not limit the medical practitioner’s professional freedom, within the scope of accepted clinical practice, to identify and provide appropriate treatments.
Practitioner agreements
(2) If a hospital or day hospital facility enters into an agreement with a *medical practitioner, under which treatment is provided to persons insured by the insurer, the agreement must not limit the medical practitioner’s professional freedom, within the scope of accepted clinical practice, to identify and provide appropriate treatments.
Note: Medical practitioners may, in dealings with private health insurers, be able to take advantage of the collective bargaining provisions of Subdivision B of Division 2 of Part VII of the Trade Practices Act 1974.
172‑10 Private health insurers to give information to Secretary
(1) The Private Health Insurance (Data Provision) Rules may specify kinds of information, relating to treatment of persons insured under *complying health insurance products that are *referable to *health benefits funds, that private health insurers are to give to the Secretary of the Department.
(2) A private health insurer must, in accordance with the Private Health Insurance (Data Provision) Rules, give to the Secretary of the Department any information of that kind that the insurer receives from a *hospital.
172‑15 Restrictions on payment of pecuniary penalties etc.
A private health insurer must not:
(a) use its money, or permit the use of its money, for:
(i) the payment of a pecuniary penalty imposed on a *director or *officer of the insurer because of an offence under this Act; or
(ii) the payment of an amount that a director or officer of the insurer, or a person who has been such a director or officer, is liable to pay under Division 149, 152, 203 or 293; or
(b) reimburse:
(i) a director or officer of the insurer in respect of a pecuniary penalty imposed on the director or officer because of an offence under this Act; or
(ii) a director or officer of the insurer, or a person who has been such a director or officer, in respect of a liability imposed on the director under Division 149, 152, 203 or 293.
180‑1 What this Chapter is about
Private health insurers who do not comply with this Act may have action taken against them under this Chapter. Both the Minister and the Council have powers under this Chapter.
Note: The methods set out in this Chapter are not the only enforcement methods available (see for example Division 84).
Part 5‑2—General enforcement methods
Division 185—What this Part is about
This Part gives the Minister and the Council powers that enable them to find out whether a private health insurer is complying with its enforceable obligations or (in the case of the Council) its Council‑supervised obligations, and to encourage or compel an insurer to comply with those obligations.
The Minister can:
(a) set performance indicators for insurers;
(b) seek explanations from insurers;
(c) investigate insurers;
(d) obtain enforceable undertakings from insurers;
(e) direct insurers to do particular things;
(f) seek remedies in the Federal Court;
(g) revoke an insurer’s entitlement to offer tax rebates as premium reductions.
The Council can also do these things (except those mentioned in paragraphs (a) and (g)), as well as take action under Part 5‑3 in relation to an insurer’s health benefits fund.
185‑5 Meaning of enforceable obligation
All of the following provisions are enforceable obligations:
(a) a provision of this Act;
(b) a provision of any Private Health Insurance Rules made under section 333‑20 or 333‑25;
(c) a provision of the regulations;
(d) a direction given to a private health insurer under this Act;
(e) if the insurer is a *restricted access insurer—a provision included in the insurer’s constitution in order to comply with subsection 126‑20(6).
185‑10 Meaning of Council‑supervised obligation
All of the following *enforceable obligations are Council‑supervised obligations, to the extent to which they relate to risk equalisation, *health benefits funds or Division 163 (*prudential standards):
(a) a provision of this Act;
(b) a provision of any Private Health Insurance Rules made under section 333‑20 or 333‑25;
(c) a provision of the regulations;
(d) a direction given to a private health insurer under this Act.
Division 188—Performance indicators
(1) The Private Health Insurance (Complying Product) Rules may set out performance indicators to be used by the Minister in monitoring private health insurers’ compliance with the principle of community rating in section 55‑5 and the community rating requirements in Division 66.
(2) The performance indicators are to be framed:
(a) to assist the Minister in detecting breaches of the principle of community rating in section 55‑5 or the community rating requirements in Division 66; and
(b) to alert the Minister to any practices of a private health insurer in relation to community rating that may require investigation; and
(c) to alert the Minister to any practices of one or more private health insurers in relation to community rating that may be contrary to government health policy and may require a regulatory response.
Division 191—Explanation of private health insurer’s operations
191‑1 Minister or Council may seek an explanation from a private health insurer
(1) If:
(a) the Minister believes that, having regard to information available to the Minister or to any performance indicators under the Private Health Insurance (Complying Product) Rules, a private health insurer may have contravened an *enforceable obligation; or
(b) the Council believes that, having regard to information available to the Council, a private health insurer may have contravened a *Council‑supervised obligation;
the Minister (if paragraph (a) applies) or the Council (if paragraph (b) applies) may write to the private health insurer:
(c) explaining the writer’s concerns; and
(d) asking the insurer to explain its operations in relation to those concerns; and
(e) specifying the period within which the writer requires the insurer’s response.
(2) The private health insurer must respond within the specified period, or any longer period that the writer, in writing before the end of the specified period, allows.
(3) If the writer refuses a request by the private health insurer for a longer period to respond, the writer must state the writer’s reasons for refusing.
Note: Refusals of requests for longer periods to respond are reviewable under Part 6‑9.
191‑5 Writer must respond to insurer’s explanation
The writer under subsection 191‑1(1) must, after receiving an explanation from a private health insurer in response, inform the insurer in writing:
(a) whether the writer is or is not satisfied with the explanation; and
(b) if the writer is not satisfied with the explanation—what steps the writer intends to take.
Division 194—Investigation of private health insurer’s operations
194‑1 Minister or Council may investigate a private health insurer
(1) The Minister may, at any time and for any reason, begin an investigation of the operations of a private health insurer by doing either or both of the following:
(a) giving a notice under any one or more sections of this Division;
(b) authorising a person under section 194‑25.
(2) The Council may, at any time, if for any reason it considers that a private health insurer might have contravened a *Council‑supervised obligation or it otherwise has concerns about the insurer’s compliance with a Council‑supervised obligation, begin an investigation of the operations of a private health insurer by doing either or both of the following:
(a) giving a notice under any one or more sections of this Division;
(b) authorising a person under section 194‑25.
194‑5 Notice to give information
(1) The Minister, or, if subsection 194‑1(2) applies, the Council, may give a written notice to a person who is or who has been an *officer, employee or agent of:
(a) a private health insurer; or
(b) an entity that was a private health insurer at any time in the year ending on the day on which the notice is given;
requiring the person to give the notice‑giver or the person specified in the notice, within the period specified in the notice, information about the area of the insurer’s operations specified in the notice.
(2) The notice‑giver may require the person to give the information orally or in writing.
(3) The notice‑giver may require the person to give the information on oath or affirmation. For that purpose, the notice‑giver or the person specified in the notice may administer an oath or affirmation.
(4) The person is not excused from giving information on the ground that giving the information might tend to incriminate the person or make the person liable to a penalty. However, the information, or anything obtained as a direct or indirect consequence of the information, is not admissible in evidence against the person in any proceedings, other than proceedings for an offence against section 137.1 or 137.2 of the Criminal Code.
194‑10 Notice to produce documents
(1) The Minister, or, if subsection 194‑1(2) applies, the Council, may give a written notice to a person who is or who has been an *officer, employee or agent of:
(a) a private health insurer; or
(b) an entity that was a private health insurer at any time in the year ending on the day on which the notice is given;
requiring the person to produce, at the time and place specified in the notice, records, books, accounts and other documents of the insurer that are in the person’s custody or under the person’s control and that relate to the area of the insurer’s operations specified in the notice.
(2) The person is not excused from producing a document on the ground that the production of the document might tend to incriminate the person or make the person liable to a penalty. However, the production of the document, or anything obtained as a direct or indirect consequence of the production, is not admissible in evidence against the person in any proceedings, other than proceedings for an offence against section 137.1 or 137.2 of the Criminal Code.
194‑15 Notice to give evidence
(1) The Minister, or, if subsection 194‑1(2) applies, the Council, may give a written notice to a person who is or who has been an *officer, employee or agent of:
(a) a private health insurer; or
(b) an entity that was a private health insurer at any time in the year ending on the day on which the notice is given;
requiring the person to attend, at the time and place specified in the notice, before the notice‑giver or the person specified in the notice and give evidence relating to an area of the insurer’s operations specified in the notice.
(2) The notice‑giver may require the person to give the evidence orally or in writing.
(3) The notice‑giver may require the person to give the evidence on oath or affirmation. For that purpose, the notice‑giver or the person specified in the notice may administer an oath or affirmation.
(4) The person is not excused from answering a question on the ground that the answer to the question might tend to incriminate the person or make the person liable to a penalty. However, the answer, or anything obtained as a direct or indirect consequence of the answer, is not admissible in evidence against the person in any proceedings, other than proceedings for an offence against section 137.1 or 137.2 of the Criminal Code.
194‑20 Offences in relation to investigation notices
(1) A person must not fail to comply with a requirement contained in a notice given to the person:
(a) under section 194‑5 (notice to give information); or
(b) under section 194‑10 (notice to produce documents); or
(c) under section 194‑15 (notice to give evidence).
Penalty: 10 penalty units.
(2) A person must not fail to be sworn or to make an affirmation when required to do so:
(a) under section 194‑5 (notice to give information); or
(b) under section 194‑15 (notice to give evidence).
Penalty: 10 penalty units.
(3) An offence under subsection (1) or (2) is an offence of strict liability.
Note: For strict liability, see section 6.1 of the Criminal Code.
194‑25 Authorisation to examine books and records etc.
(1) The Minister, or, if subsection 194‑1(2) applies, the Council, may, in writing, authorise a person to examine and report on the records, books, accounts and other documents of:
(a) a private health insurer; or
(b) an entity that was a private health insurer at any time in the year ending on the day on which the authorisation is given.
(2) A person authorised under subsection (1) must, at all reasonable times, have full and free access to any *premises at which the records, books, accounts and other documents are kept and may take extracts from, or copies of, the records, books, accounts and other documents.
194‑30 Minister may consult Council
If, in the course of an investigation conducted by the Minister, the Minister believes that there are issues concerning a *Council‑supervised obligation, the Minister may:
(a) consult the Council on that matter; and
(b) if the Minister considers it appropriate—request the Council to take over any part of the investigation that relates to those issues.
194‑35 Minister or Council must notify outcome of investigation
After completing an investigation under this Division of a private health insurer or former private health insurer, the Minister or the Council (whichever was the investigator) must inform the insurer in writing:
(a) whether the investigator is or is not satisfied with the performance of the insurer; and
(b) if the investigator is not satisfied with the performance of the insurer—what steps the investigator intends to take.
Division 197—Enforceable undertakings
197‑1 Minister or Council may accept written undertakings given by a private health insurer
(1) The Minister may accept a written undertaking, given by a private health insurer at the Minister’s request, if the Minister considers that compliance with the undertaking will:
(a) be likely to improve the performance of the insurer; or
(b) if the Minister is satisfied that the insurer has contravened an *enforceable obligation—be likely to ensure that the insurer will cease to be in contravention of the enforceable obligation.
(2) The Council may accept a written undertaking, given by a private health insurer at the Council’s request, if the Council considers that compliance with the undertaking will be likely to improve the insurer’s operations in relation to its *Council‑supervised obligations.
(3) The private health insurer may withdraw or vary the undertaking at any time with the consent of the acceptor of the undertaking.
197‑5 Enforcement of undertakings
(1) If the acceptor of an undertaking under this Division considers that a private health insurer that gave an undertaking under this Division has contravened any of its terms, the acceptor may apply to the Federal Court for an order under subsection (2).
(2) If the Federal Court is satisfied that the private health insurer has contravened a term of the undertaking, the court may make one or more of the following orders:
(a) an order directing the insurer to comply with the terms of the undertaking;
(b) if there is a contravention of an *enforceable obligation—any other order of a kind set out in Division 203 that the court considers appropriate.
Division 200—Ministerial and Council directions
200‑1 Minister or Council may give directions
(1) If, at any time and for any reason:
(a) the Minister considers that it will assist in the prevention of *improper discrimination to do so; or
(b) the Council considers that it will assist in the prevention of contraventions of *Council‑supervised obligations to do so;
the Minister (if paragraph (a) applies) or Council (if paragraph (b) applies) may give a direction to a private health insurer requiring it:
(c) to modify its day‑to‑day operations in a particular respect; or
(d) to modify its *rules in a particular respect; or
(e) if the insurer is a *restricted access insurer and the Minister gives the direction—to modify the provisions included in its constitution in order to comply with subsection 126‑20(6) in a particular respect.
Note: A decision to give a direction is reviewable under Part 6‑9.
(2) If, at any time and for any reason:
(a) the Minister considers that there appears to be a contravention of an *enforceable obligation involving *improper discrimination by a private health insurer; or
(b) the Council considers that there appears to be a contravention of a *Council‑supervised obligation;
the Minister (if paragraph (a) applies) or Council (if paragraph (b) applies) may give a direction to the insurer:
(c) requiring it to modify its day‑to‑day operations; or
(d) requiring it to modify its *rules; or
(e) if the insurer is a *restricted access insurer and the Minister gives the direction—requiring it to modify the provisions included in its constitution in order to comply with subsection 126‑20(6);
so as to address that contravention.
Note: A decision to give a direction is reviewable under Part 6‑9.
(3) A direction mentioned in subsection (1) or (2) may, if the person who gives the direction considers it proper to do so, include requirements with respect to the reconsideration by the private health insurer of an application or claim made to the insurer and dealt with by it before the direction takes effect.
(4) A private health insurer must, in reconsidering an application or claim in accordance with subsection (3), deal with the application or claim as if the direction had been in force at the time when the application or claim was first considered.
(5) A direction given under this section must be published:
(a) if given by the Minister—on the Department’s website; and
(b) if given by the Council—on the Council’s website;
not later than 5 working days after the direction is given.
A direction given under this Division to a private health insurer:
(a) must be in writing; and
(b) must be signed by the person giving the direction; and
(c) may be served on the insurer by serving a copy on the insurer’s *chief executive officer.
Note: Private health insurers must keep the Department and Council informed about who the current chief executive officer is (see section 169‑15).
Division 203—Remedies in the Federal Court
203‑1 Minister or Council may apply to the Federal Court
(1) If the Minister is satisfied that a private health insurer has contravened an *enforceable obligation, the Minister may apply to the Federal Court for:
(a) a *declaration of contravention; and
(b) any one or more of the following orders:
(i) a pecuniary penalty order under section 203‑10;
(ii) a compensation order under section 203‑15;
(iii) an adverse publicity order under section 203‑20;
(iv) any other order that the Minister considers to be appropriate to redress the contravention.
(2) If the Council is satisfied that a private health insurer has contravened a *Council‑supervised obligation, the Council may apply to the Federal Court for:
(a) a *declaration of contravention; and
(b) either or both of the following orders:
(i) a pecuniary penalty order under section 203‑10;
(ii) any order that the Council considers to be appropriate to redress the contravention, other than an order under section 203‑15 or 203‑20.
203‑5 Declarations of contravention
(1) If the Federal Court is satisfied that a private health insurer has contravened an *enforceable obligation, it must make a declaration of contravention.
(2) The declaration must specify:
(a) the *enforceable obligation that was contravened; and
(b) the private health insurer that contravened the provision; and
(c) the conduct that constituted the contravention; and
(d) if the court is satisfied that an *officer of the private health insurer failed to take reasonable steps to prevent the insurer contravening the enforceable obligation—the officer.
(3) A *declaration of contravention is conclusive evidence of the matters mentioned in subsection (2).
203‑10 Pecuniary penalty order
(1) If the Federal Court has made a *declaration of contravention (whether on application by the Minister or the Council) that specifies an *officer of a private health insurer (see paragraph 203‑5(2)(d)), the court may order the officer to pay the Commonwealth a pecuniary penalty of up to 1,000 penalty units.
(2) The court must not make an order under subsection (1) if it is satisfied that a court has ordered the *officer to pay damages in the nature of punitive damages in respect of:
(a) the contravention of the *enforceable obligation; or
(b) the officer’s failure to take reasonable steps to prevent the insurer contravening the enforceable obligation.
(3) The penalty is a civil debt payable to the Commonwealth. The Commonwealth may enforce the order as if it were an order made in civil proceedings against the *officer to recover a debt due by the officer. The debt arising from the order is taken to be a judgment debt.
(1) If the Federal Court has made a *declaration of contravention on application by the Minister, the court may order the private health insurer specified in the declaration to compensate an individual for any injury or loss suffered by the individual as a result of the contravention.
(2) The order must specify the amount of compensation.
(3) The order may be enforced as if it were a judgment of the court.
203‑20 Adverse publicity order
(1) If the Federal Court has made a *declaration of contravention on application by the Minister, the court may make an order requiring the private health insurer specified in the declaration to do either or both of the following:
(a) disclose in a way, and to the person or persons, specified in the order, the information specified in the notice to correct or counter the effect of the contravention;
(b) publish, in the way specified in the order, an advertisement to correct or counter the effect of the contravention in the terms specified in, or determined in accordance with, the order.
(2) The order may be enforced as if it were a judgment of the court.
(1) If the Federal Court has made a *declaration of contravention (whether on application by the Minister or the Council), the court may make any order that the applicant applies for.
(2) The order may be enforced as if it were a judgment of the court.
203‑30 Time limit for declarations and orders
Proceedings under this Division may be started no later than 6 years after the contravention.
203‑35 Civil evidence and procedure rules for declarations and orders
The Federal Court must apply the rules of evidence and procedure for civil matters in proceedings under this Division.
Note: The standard of proof in civil proceedings is the balance of probabilities (see section 140 of the Evidence Act 1995).
203‑40 Civil proceedings after criminal proceedings
The Federal Court must not make a pecuniary penalty order against an *officer of a private health insurer under section 203‑10 if the officer has been convicted of an offence constituted by conduct that is substantially the same as the conduct to which the court had regard in satisfying itself that the officer failed to take reasonable steps to prevent the insurer contravening the *enforceable obligation.
203‑45 Criminal proceedings during civil proceedings
(1) Proceedings for a pecuniary penalty order against an *officer of a private health insurer are stayed if:
(a) criminal proceedings are started or have already been started against the officer for an offence; and
(b) the offence is constituted by conduct that is substantially the same as the conduct to which the court had regard in satisfying itself that the officer failed to take reasonable steps to prevent the insurer contravening the *enforceable obligation.
(2) The proceedings for the order may be resumed if the *officer is not convicted of the offence. Otherwise, the proceedings for the order are dismissed.
203‑50 Criminal proceedings after civil proceedings
Criminal proceedings may be started against a person for conduct that is substantially the same as conduct constituting a contravention of an *enforceable obligation regardless of whether:
(a) a *declaration of contravention has been made that specifies the person; or
(b) an order has been made against the person under this Division.
203‑55 Evidence given in proceedings for penalty not admissible in criminal proceedings
Evidence of information given or evidence of production of documents by an *officer of a private health insurer is not admissible in criminal proceedings against the officer if:
(a) the officer previously gave the evidence or produced the documents in proceedings for a pecuniary penalty order against the officer under section 203‑10 (whether or not the order was made); and
(b) the conduct alleged to constitute the offence is substantially the same as the conduct to which the court had regard in satisfying itself that the officer failed to take reasonable steps to prevent the insurer contravening the *enforceable obligation.
However, this does not apply to a criminal proceeding in respect of the falsity of the evidence given by the officer in the proceedings for the pecuniary penalty order.
203‑60 Minister or Council may require person to assist
(1) The Minister may, in writing, require a person to give all reasonable assistance in connection with:
(a) an application by the Minister:
(i) for a *declaration of contravention in relation to a private health insurer; or
(ii) for a declaration of contravention that specifies an *officer of a private health insurer; or
(iii) for a pecuniary penalty order under section 203‑10 in relation to an officer of a private health insurer; or
(b) criminal proceedings against a private health insurer, or an officer of a private health insurer, for an offence against this Act.
The person must comply with the request.
Penalty: 5 penalty units.
(2) The Council may, in writing, require a person to give all reasonable assistance in connection with an application by the Council:
(a) for a *declaration of contravention in relation to a private health insurer; or
(b) for a declaration of contravention that specifies an *officer of a private health insurer; or
(c) for a pecuniary penalty order under section 203‑10 in relation to an officer of a private health insurer.
The person must comply with the request.
Penalty: 5 penalty units.
(3) The Minister or Council must not require the person to assist in connection with an application for a declaration or order unless:
(a) it appears to the Minister or Council that someone other than the person required to assist may have contravened an *enforceable obligation; and
(b) the Minister or Council suspects or believes that the person required to assist can give information relevant to the application.
(4) The Minister must not require the person to assist in connection with criminal proceedings unless:
(a) it appears to the Minister that the person required to assist is unlikely to be a defendant in the proceedings; and
(b) the person required to assist is an employee or agent (including a banker or auditor) of the private health insurer concerned.
(5) The Minister or Council may require the person to assist regardless of whether:
(a) an application for the declaration or order has actually been made; or
(b) criminal proceedings for the offence have actually begun.
(6) The person cannot be required to assist if the person is or has been a lawyer for:
(a) in an application for a declaration or order—the person suspected of the contravention; or
(b) in criminal proceedings—a defendant or likely defendant in the proceedings.
(7) The Federal Court may order the person to comply with the requirement in a specified way. Only the Minister and the Council may apply to the court for an order under this subsection.
203‑65 Relief from liability for contravening an enforceable obligation
(1) If, in proceedings brought against a person under this Division, it appears to the Federal Court that:
(a) the person has, or may have:
(i) contravened an *enforceable obligation; or
(ii) if the person is an *officer of a private health insurer—failed to take reasonable steps to prevent the insurer from contravening an enforceable obligation; but
(b) the person has acted honestly and, having regard to all the circumstances of the case, the person ought fairly to be excused for the contravention;
the court may relieve the person either wholly or partly from a liability to which the person would otherwise be subject, or that might otherwise be imposed on the person, because of the contravention.
(2) A person who thinks that proceedings will or may be begun against the person under this Division may apply to the Federal Court for relief.
(3) On an application under subsection (2), the court may grant relief under subsection (1) as if the proceedings had been begun in the court.
(4) For the purposes of subsection (1) as applying for the purposes of a case tried by a judge with a jury:
(a) a reference in that subsection to the court is a reference to the judge; and
(b) the relief that may be granted includes withdrawing the case in whole or in part from the jury and directing judgment to be entered for the defendant on such terms as to costs as the judge thinks appropriate.
203‑70 Powers of Federal Court
A provision of this Act conferring a power on the Federal Court does not affect any other power of the court conferred by this Act or otherwise.
Division 206—Revoking entitlement to offer rebate as a premium reduction
206‑1 Revocation of status of participating insurer
(1) If a *participating insurer:
(a) has repeatedly failed to comply with subsection 26‑1(5) (receipt for payment of premiums); or
(b) has failed to comply with a condition specified in the Private Health Insurance (Incentives) Rules as a condition of participation in the *premiums reduction scheme; or
(c) refuses or fails to comply with:
(i) a direction given by the Minister under section 200‑1; or
(ii) the principle of community rating in section 55‑5;
the Minister may, by notice given to the insurer, revoke the insurer’s status as a participating insurer.
(2) Upon the giving of the notice, the insurer ceases to be a *participating insurer.
Note: Decisions to revoke an insurer’s status as a participating insurer are reviewable under Part 6‑9.
Part 5‑3—Enforcement of health benefits fund requirements
In order to protect the interests of the policy holders, and to ensure that health benefits funds are operated in accordance with Part 4‑4, specific powers and processes are required in addition to the general powers and processes in Part 5‑2.
Inspectors may be appointed to investigate the affairs of private health insurers, and external managers may be appointed to manage health benefits funds. These processes may lead to terminating managers of funds being appointed.
The purpose of this Part is:
(a) to provide for the supervision of the business, affairs and property of *health benefits funds, so as to ensure that the business and affairs are carried on, and the property is managed:
(i) in the interests of the *policy holders of the funds; and
(ii) in accordance with Part 4‑4; and
(b) to provide for the *external management of health benefits funds in a way consistent with the interests of those policy holders; and
(c) to provide, as a consequence either of that supervision or external management, for the orderly termination of health benefits funds in a way that is consistent with the interests of those policy holders.
211‑10 The Private Health Insurance (Health Benefits Fund Enforcement) Rules
Enforcement of the requirements for *health benefits funds is also dealt with in the Private Health Insurance (Health Benefits Fund Enforcement) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Health Benefits Fund Enforcement) Rules are made by the Minister under section 333‑20.
211‑15 Limitation on external management and termination of health benefits funds
(1) Despite the provisions of any other law of the Commonwealth or of any law of a State or Territory, a *health benefits fund can only be placed under *external management, or dealt with as a fund under external management, in accordance with Division 217.
(2) Despite the provisions of any other law of the Commonwealth or any other law of a State or Territory, a *health benefits fund can only be terminated in accordance with Division 149.
Division 214—Investigations into affairs of private health insurers
214‑1 Investigation of private health insurers by inspectors
(1) The Council may, in writing, appoint an *inspector to investigate the affairs of a private health insurer if the Council has reason to suspect that:
(a) the affairs of the insurer are being, or are about to be, carried on in a way that is not in the interests of the *policy holders of a *health benefits fund conducted by the insurer; or
(b) the insurer has contravened a provision of Part 4‑4.
(2) The instrument of appointment must specify:
(a) the matter referred to in paragraph (1)(a) or (b) that the Council suspects; and
(b) the ground on which the Council suspects the matter; and
(c) the matters into which the investigation is to be made, being the whole or some part of the affairs of the insurer.
(3) An *inspector so appointed may be a person engaged or appointed under the Public Service Act 1999 or by an authority of the Commonwealth.
(1) An *inspector may, by notice in writing given to a person whom the inspector believes to have some knowledge of the affairs of the private health insurer that the inspector is investigating, require that person:
(a) to produce to the inspector all or any of the records relating to the affairs of the insurer that are in the custody, or under the control, of that person; or
(b) to give to the inspector all reasonable assistance within the person’s power in connection with the investigation; or
(c) to appear before the inspector for examination concerning matters that are relevant to the investigation and are within the knowledge of the person;
within the period (that must not be less than 14 days) specified in the notice.
(2) If records are produced to an *inspector under subsection (1), the inspector may:
(a) take possession of them for such period as the inspector thinks necessary for the purposes of the investigation; and
(b) make copies of, and take extracts from, them.
(3) An *inspector is not entitled to refuse to permit a person to inspect records that are in the possession of the inspector under subsection (2) if the person would be entitled to inspect those records if the inspector had not taken possession of them.
(4) A person who complies with a requirement of an *inspector under subsection (1) does not incur any liability to any other person merely because of that compliance.
214‑10 Person may be represented by lawyer
A lawyer acting for a person being examined by an *inspector:
(a) may attend the examination; and
(b) may, to the extent that the inspector allows:
(i) address the inspector; and
(ii) examine the person;
in relation to matters in respect of which the inspector has questioned the person.
214‑15 Compliance with requirements of inspectors
(1) A person is guilty of an offence if the person refuses or fails to comply with a requirement of an *inspector under section 214‑5 that is applicable to the person.
Penalty: 30 penalty units or imprisonment for 6 months, or both.
(2) However, the person is only required to comply with the requirement to the extent that the person is capable of doing so.
Note: The defendant bears an evidential burden in relation to the matter in subsection (2). See subsection 13.3(3) of the Criminal Code.
(3) A person being examined by an *inspector is not excused from answering a question put to the person by the inspector on the ground that the answer might tend to incriminate the person.
(4) However, if the person informs the *inspector before answering the question that the answer might tend to incriminate the person, neither the question nor the answer is admissible in evidence against the person in criminal proceedings (other than proceedings in relation to an offence under subsection (1)).
(1) An *inspector who:
(a) is empowered to investigate the whole or a part of the affairs of a private health insurer; and
(b) enters any *premises under subsection (3) or in accordance with a warrant granted under subsection (5);
may exercise the functions of an inspector under this section in relation to the insurer.
(2) The functions of an *inspector under this section in relation to the insurer are to exercise *search powers in relation to any records that relate, or that the inspector believes, on reasonable grounds, to relate, to the affairs of the insurer.
(3) An *inspector may, with the consent of the *occupier of any *premises, enter the premises for the purpose of exercising the functions of an inspector under this section in relation to the private health insurer whose affairs the inspector is empowered to investigate.
(4) An *inspector who has reason to believe that there are on any *premises records relating to the affairs of the private health insurer whose affairs the inspector is empowered to investigate may apply to a Magistrate for a warrant authorising the inspector to enter the premises for the purpose of exercising the functions of an inspector under this section in relation to the insurer.
(5) The Magistrate may grant a warrant if satisfied by information on oath or affirmation:
(a) that there is reasonable ground for believing that there are on the *premises to which the application relates any records relating to the affairs of the insurer concerned; and
(b) that the issue of a warrant is reasonably required for the purposes of this Act.
The warrant may be in the form set out in the Private Health Insurance (Health Benefits Fund Enforcement) Rules.
(6) The warrant authorises the *inspector, with such assistance as the inspector thinks necessary, to enter the *premises, using such force as is necessary and reasonable in the circumstances:
(a) during such hours of the day or night as the warrant specifies; or
(b) if the warrant so specifies, at any time;
for the purpose of exercising the functions of an inspector under this section in relation to the insurer concerned.
(7) A person is guilty of an offence if the person obstructs or hinders an *inspector exercising the functions of an inspector under this section.
Penalty: 30 penalty units or imprisonment for 6 months, or both.
(8) Subsection (7) does not apply if the person has a reasonable excuse.
Note: The defendant bears an evidential burden in relation to the matter in subsection (8). See subsection 13.3(3) of the Criminal Code.
(1) An *inspector:
(a) must, on the completion or termination of an investigation of the whole or a part of the affairs of a private health insurer, report in writing to the Council on the result of the investigation; and
(b) if so directed in writing by the Council, must make such written reports during the investigation as are specified in the direction; and
(c) may make one or more other written reports to the Council during the investigation.
(2) The report made on the completion of the investigation must include the *inspector’s recommendations with respect to:
(a) the question whether the insurer should be permitted to continue to conduct a particular *health benefits fund; and
(b) the question whether the insurer’s affairs should be reorganised to enable it better to conduct the fund and, if so, the way in which they should be reorganised; and
(c) such other matters affecting the insurer, or the interests of the *policy holders of the fund, as the inspector thinks fit.
(3) If the matters investigated included:
(a) the question whether the insurer is, or is about to become, unable to meet its liabilities relating to a *health benefits fund; or
(b) the question whether the insurer’s affairs are being, or are about to be, carried on in a way that is not in the interests of the *policy holders of the fund;
the report made on the completion of the investigation must include a statement of the *inspector’s opinion in relation to that question and the facts on which that opinion is based.
(4) An *inspector must not include in a report under this section:
(a) a recommendation relating to the institution of criminal proceedings; or
(b) a statement to the effect that, in the inspector’s opinion, a specified person has committed a criminal offence.
(5) However, if an *inspector is of the opinion that criminal proceedings ought to be instituted or that a person has committed a criminal offence, the inspector must state that opinion in writing given to the Council.
214‑30 Dissemination of reports
(1) The Council must give a copy of a report made to the Council under paragraph 214‑25(1)(a) to the private health insurer to which the report relates.
(2) However, subsection (1) does not apply if the Council thinks that, having regard to proceedings that have been or might be instituted, a copy of the report should not be given to the insurer.
(3) If the Council has given a copy of the report to the insurer under subsection (1), the Council may, if it thinks it is in the public interest to do so, cause the whole or a part of the report to be published.
(4) A court before which proceedings under this Act are brought against a private health insurer or other person in respect of matters dealt with in a report under section 214‑25 may order that a copy of the report be given to that insurer or other person.
214‑35 Liability for publishing reports etc.
(1) An action or proceeding, civil or criminal, does not lie against a person for publishing in good faith a copy of, or a fair extract from or of, a publication made under subsection 214‑30(3).
(2) An action or proceeding, civil or criminal, does not lie against an *inspector:
(a) in respect of the publication to the Council of a report under section 214‑25; or
(b) in respect of the inspector’s opinion given to the Council in accordance with subsection 214‑25(5);
if the inspector has acted in good faith.
(3) For the purposes of this section, a publication or other action is taken to be made in good faith if the person by whom it is made is not actuated by ill will to a person affected by the publication or other action, or by any other improper motive.
214‑40 Delegation by inspectors
(1) An *inspector may, by writing signed by the inspector, delegate any of the inspector’s powers under this Act to a person engaged or appointed under the Public Service Act 1999 or by an authority of the Commonwealth.
(2) A delegate who proposes to exercise his or her delegated powers must, at the request of any person who may be affected by the proposed exercise, produce for the inspection of that person the instrument of delegation or a copy of that instrument.
Note: See also sections 34AA, 34AB and 34A of the Acts Interpretation Act 1901 relating to delegations.
214‑45 Records not to be concealed etc.
(1) A person is guilty of an offence if:
(a) the person engages in conduct; and
(b) the conduct results in the concealment, destruction, mutilation or alteration of records relating to the affairs of a private health insurer; and
(c) those affairs are being investigated under this Act.
Penalty: 30 penalty units or imprisonment for 6 months, or both.
(2) Subsection (1) does not apply if the person did not act with intent to defeat the purposes of this Act and did not act with intent to delay or obstruct the carrying out of the investigation under this Act.
Note: The defendant bears an evidential burden in relation to the matters in subsection (2). See subsection 13.3(3) of the Criminal Code.
Division 217—External management of health benefits funds
The purpose of this Division is to permit the business, affairs and property of a *health benefits fund under *external management to be managed in a way:
(a) that maximises the chance that the *policy holders of the fund continue to be *covered for health insurance either by that fund or by another fund to which the business of that fund is transferred; or
(b) if it is not possible for that coverage to be maintained—that, to the extent possible, safeguards the financial interests of those policy holders if the fund is terminated.
217‑5 The basis of the law relating to external management
(1) The *external management of a *health benefits fund is regulated:
(a) by the provisions of this Division; and
(b) by the provisions of Divisions 6, 7, 8, 10, 11, 13 and 16 of Part 5.3A of Chapter 5 of the Corporations Act 2001 and of Division 7A of Part 5.6 of that Chapter, all applying, so far as they are capable of so doing, subject to such modifications as are set out in:
(i) this Act; or
(ii) the Private Health Insurance (Health Benefits Fund Enforcement) Rules.
(2) Subject to this section, any provisions of a law of the Commonwealth, or a State or Territory, that, but for this section, would relate to the *external management of such a fund cease, by force of this section, to apply in relation to the fund.
(3) In the application of the provisions of the Corporations Act 2001 referred to in subsection (1) in relation to the *external management of a *health benefits fund, those provisions apply as if:
(a) a reference to the company were a reference to the fund; and
(b) a reference to the administrator were a reference to the *external manager of the fund appointed under this Act; and
(c) a reference to the Court were a reference to the Federal Court.
(4) The Private Health Insurance (Health Benefits Fund Enforcement) Rules may provide for different modifications according to the nature of the *health benefits fund that is to be, or that is being, administered.
Subdivision 217‑B—Appointment of external managers
217‑10 Council may appoint external managers
(1) The Council may, in writing, appoint a person as the *external manager of a *health benefits fund if the requirements of subsections 217‑15(1) and (2) are satisfied.
(2) However, the person:
(a) must be registered, or taken to be registered, as an official liquidator under the Corporations Act 2001; and
(b) must not be a person who is:
(i) a *policy holder of the fund; or
(ii) an auditor of the fund; or
(iii) a chargee of property of the fund; or
(iv) an officer of a body corporate that is a chargee of property of the fund; or
(v) a person who is otherwise related to the fund.
(3) The appointment takes effect from the date specified in the instrument of appointment.
217‑15 Grounds of appointment of external managers
(1) The Council must not appoint an *external manager to a *health benefits fund unless the Council believes that the appointment of an external manager to the fund is, in the circumstances, in the interests of the *policy holders of the fund.
(2) The Council must not appoint an *external manager to a *health benefits fund unless:
(a) the Council is satisfied, on reasonable grounds, that the private health insurer conducting the fund has contravened section 140‑15 (compliance with the *solvency standard) in its conduct of the fund; or
(b) the Council is satisfied, on reasonable grounds, that the insurer has, in its conduct of the fund, contravened a *solvency direction, a *capital adequacy direction or *prudential direction that the Council has given to the insurer; or
(c) a request for *external management of the fund is made to the Council by a resolution of the board of *directors of the insurer; or
(d) a ground specified in the Private Health Insurance (Health Benefits Fund Enforcement) Rules made for the purposes of this paragraph applies in respect of the fund.
(3) In forming the requisite state of mind for the purpose of subsection (1), or of any Private Health Insurance (Health Benefits Fund Enforcement) Rules made for the purposes of paragraph(2)(d) that require a particular state of mind, the Council may have regard:
(a) to any information in its own records; and
(b) to any report or return made to it, including any report received from an *inspector under section 214‑25.
217‑20 External managers to displace management of funds
If a person is appointed as *external manager of a *health benefits fund, then, for so long as the fund is under *external management:
(a) the management of the fund vests in the external manager; and
(b) any *officer of the *responsible insurer for the fund who was vested with the management of the fund immediately before the appointment of the external manager is, by force of this section, divested of that management.
Subdivision 217‑C—Duties and powers of external managers
217‑25 Duties of external managers
(1) The main duties of the *external manager of a *health benefits fund are:
(a) to examine the business, affairs and property of the fund; and
(b) to ascertain the *assets and liabilities of the fund; and
(c) if the business of the fund has been mixed with other business of the private health insurer concerned—to apportion the assets and liabilities as between the fund and that other business; and
(d) to form an opinion as to which course of action maximises the chance that the *policy holders of the fund continue to be *covered for health insurance either by that fund or by another fund to which the business of that fund is transferred; and
(e) to make a final written report to the Council, in accordance with Subdivision 217‑E, recommending that course of action.
(2) In the day‑to‑day administration of a *health benefits fund, it is the duty of the *external manager to administer the fund as efficiently and economically as possible.
217‑30 Additional powers of external managers
(1) In the application of the provisions of Division 8 of Part 5.3A of Chapter 5 of the Corporations Act 2001, for the purpose of:
(a) conferring further powers on the *external manager of a *health benefits fund; and
(b) where appropriate, qualifying the exercise of those powers;
the provisions of that Division are taken not to include section 442A or subsection 442D(1).
(2) For the purposes of section 442F of the Corporations Act 2001 as so applying, sections 128 and 129 of that Act are also taken to apply, subject to such modifications as are specified in the Private Health Insurance (Health Benefits Fund Enforcement) Rules.
217‑35 Protection of property during external management
(1) In the application of the provisions of Division 6 of Part 5.3A of Chapter 5 of the Corporations Act 2001 in relation to the protection, during the *external management of a *health benefits fund, of the property of the fund, the provisions of that Division are taken not to include section 440A.
(2) In determining, for the purposes of section 440D of the Corporations Act 2001 as so applying, whether the *external manager should consent to, or the court should give leave for, a person’s beginning or continuing legal proceedings, the external manager or the court must have regard to whether:
(a) the proceedings do, or do not, relate to any property of the fund under *external management; and
(b) the proceedings would, or would not, be materially detrimental to the interests of the *policy holders of the fund.
217‑40 Rights of chargee, owner or lessor of property of fund under external management
(1) In the application of the provisions of Division 7 of Part 5.3A of Chapter 5 of the Corporations Act 2001 in relation to the property of a *health benefits fund under *external management:
(a) the provisions of that Division are taken not to include section 441A; and
(b) subsection 441D(1) is taken not to include the words following paragraph 441D(1)(b).
(2) Nothing in that Division as so applying prevents:
(a) the *external manager of a *health benefits fund giving written consent; or
(b) the court giving leave;
for the enforcement of a charge, subject to any condition specified by the external manager or by the court, as the case requires, if the external manager or the court is satisfied:
(c) that the charge does not relate to the property of the fund under *external management; and
(d) that the enforcement of the charge will not be materially detrimental to the interests of the *policy holders of the fund.
Subdivision 217‑D—Procedure relating to voluntary deeds of arrangement
(1) The Private Health Insurance (Health Benefits Fund Enforcement) Rules may provide for all or any of the following:
(a) the convening by *external managers of *health benefits funds of meetings of creditors of those funds, and the *policy holders of the funds, to consider the possibility of the *responsible insurers for those funds executing *voluntary deeds of arrangement;
(b) the procedure for convening such meetings (including the giving of notices);
(c) the conduct of such meetings;
(d) the matters that may be decided at such meetings;
(e) the circumstances in which the external managers must include in their reports to the Council under section 217‑50, recommendations arising out of decisions taken at such meetings;
(f) the kinds of such recommendations that may be included in those reports;
(g) the actions that the Council may take if such recommendations are included in those reports.
(2) This section does not limit the matters that may be included in the Private Health Insurance (Health Benefits Fund Enforcement) Rules for the purposes of any other provision of this Part.
Subdivision 217‑E—External managers’ reports to Council
217‑50 External managers to give reports to Council
(1) As soon as practicable after being appointed as *external manager of a *health benefits fund, and in any case within the period under subsection (2), the external manager must:
(a) conclude the examination of the business, affairs and property of the fund; and
(b) make a final written report to the Council.
(2) The period is:
(a) the 3 months after being appointed as *external manager; or
(b) such longer period as the Council notifies to the external manager.
(3) The *external manager must, in the report to the Council:
(a) recommend a course of action that, in the external manager’s opinion, maximises, in the circumstances, the chance that the *policy holders of the fund continue to be *covered for health insurance either by that fund or by another fund to which the business of that fund is transferred; and
(b) set out the reasons for that recommendation.
(4) Without limiting subsection (3), the *external manager may recommend:
(a) subject to the Federal Court’s making an order or orders in relation to the matter, that the *responsible insurer for the fund implement a scheme of arrangement concerning the business of the fund; or
(b) subject to the Federal Court’s making an order or orders in relation to the matter, that a *terminating manager of the *health benefits funds of the responsible insurer be appointed; or
(c) that the *external management cease and that the business of the fund be resumed by the responsible insurer for the fund.
(5) However, if the Private Health Insurance (Health Benefits Fund Enforcement) Rules so provide, the *external manager must recommend that the Council approve the execution of a *voluntary deed of arrangement.
(6) Without limiting the matters that may be dealt with in a scheme of arrangement referred to in paragraph (4)(a), such a scheme may provide for:
(a) the continuance, on terms or conditions set out in the scheme, of the business of the fund; or
(b) the transfer of the fund, on terms set out in the scheme, to a private health insurer other than the *responsible insurer for the fund; or
(c) the execution of a deed in the same terms as a proposed *voluntary deed of arrangement rejected at a meeting of a kind referred to in section 217‑45.
217‑55 Dealing with reports given to the Council
(1) In deciding whether or not to approve a course of action recommended under subsection 217‑50(3), the Council may:
(a) request the *external manager to provide further information on any matter; and
(b) engage any person to assist it in evaluating assessments made, or projections relied on, by the external manager in relation to matters dealt with in the report.
The Council must have regard to the external manager’s report, and to any additional information provided by the external manager or by any person engaged to assist the Council, in reaching its decision.
(2) If the Council is satisfied that a course of action recommended by the *external manager under subsection 217‑50(3) will, in the circumstances, be in the interests of the *policy holders of the fund, the Council must, by written notice, inform the external manager to that effect and either:
(a) if the course of action is of a kind specified in paragraph 217‑50(4)(a)—direct the external manager to apply under subsection 217‑60(1) to give effect to the course of action; or
(b) if the course of action is termination of the funds of the private health insurer in question—direct the external manager to apply under subsection 220‑1(1) for the appointment of a *terminating manager of the funds.
(3) If the Council is not satisfied as mentioned in subsection (2), the Council may take a different course of action that the Council is satisfied will, in the circumstances, be in the interests of *policy holders of the fund.
(4) The courses of action that the Council may take under subsection (3) include:
(a) the Council applying to the Federal Court for an order or orders in relation to the *responsible insurer for the fund implementing a scheme of arrangement concerning the business of the fund; and
(b) the Council applying to the Federal Court for an order or orders for the appointment of a *terminating manager of the *health benefits funds of the responsible insurer.
217‑60 Court orders in respect of schemes of arrangement
(1) If, under paragraph 217‑55(2)(a), the Council directs the *external manager to apply under this subsection to give effect to a course of action of a kind specified in paragraph 217‑50(4)(a), the external manager must apply to the Federal Court for an order or orders to give effect to the course of action.
Note: For what is to happen if the course of action is to be termination of a fund, see subsection 220‑1(1).
(2) On an application under subsection (1) of this section, or under paragraph 217‑55(4)(a), for such an order or orders:
(a) the Council and any other person interested are entitled to be heard; and
(b) the Federal Court may make such order or orders in respect of the course of action the subject of the application as it considers to be, in all the circumstances, in the interests of the *policy holders of the *health benefits fund concerned.
(3) An order under this section:
(a) is binding on all persons; and
(b) takes effect despite anything in the constitution or other *rules of the *responsible insurer for the fund concerned.
(4) To avoid doubt, an order of the Federal Court is not required:
(a) in order to give effect to a *voluntary deed of arrangement—if the Council approves the execution of the deed; or
(b) in order to effect a termination of an *external management.
Subdivision 217‑F—Miscellaneous
217‑65 When an external management begins and ends
(1) The *external management of a *health benefits fund begins when an *external manager is appointed under section 217‑10 to administer the fund.
(2) The *external management of a *health benefits fund ends when:
(a) the Council terminates the appointment of the *external manager and does not appoint a replacement external manager; or
(b) a *voluntary deed of arrangement relating to the fund is executed; or
(c) the Council notifies the external manager, under subsection 217‑55(2), that it has accepted the external manager’s recommendation, made under subsection 217‑50(4), that the external management cease; or
(d) the Federal Court makes an order or orders under section 217‑60 for a course of action approved by the Council and incorporated in a scheme of arrangement; or
(e) a *terminating manager of the fund is appointed.
217‑70 Effect of things done during external management of health benefits funds
A payment made, transaction entered into, or other act or thing done, in good faith, by, or with the consent of, the *external manager of a *health benefits fund:
(a) is valid and effectual for the purposes of this Act and for the purposes of the Corporations Act 2001 as it applies in relation to the fund; and
(b) is not liable to be set aside in a termination of the fund.
217‑75 Disclaimer of onerous property
(1) In the application of the provisions of Division 7A of Part 5.6 of Chapter 5 of the Corporations Act 2001 for the purpose of determining the power of an *external manager of a *health benefits fund to disclaim property of the fund, those provisions have effect as if:
(a) the external manager were the liquidator of the company that the fund is taken to constitute; and
(b) the references in subsections 568B(3) and 568E(5) of that Act to the company’s creditors were references to the *policy holders of the fund.
(2) A disclaimer by an *external manager of a *health benefits fund has the same effect, and the external manager is under the same obligations, for the purposes of this Act, as if the disclaimer had been made under Division 7A of Part 5.6 of Chapter 5 of the Corporations Act 2001.
217‑80 Application of provisions of Corporations Act
Regulations etc. under the Corporations Act
(1) A reference in an *application provision to an *applied Corporations Act provision includes (unless the contrary intention appears) a reference to any regulations or other instruments in force for the purposes of that provision, or any of those provisions, of the Corporations Act 2001.
Note: So, for example, a provision of this Act that applies a particular provision of the Corporations Act 2001 also applies any regulations that have effect for the purposes of that provision (unless a contrary intention appears).
(2) An application provision is a provision of this Division that:
(a) provides for the application of a provision, or a group of provisions (including a Chapter, Part, Division or Subdivision), of the Corporations Act 2001; or
(b) refers to a provision, or group of provisions, of the Corporations Act 2001 as so applied.
(3) An applied Corporations Act provision is a provision, or a provision in a group of provisions, of the Corporations Act 2001 that is applied as mentioned in paragraph (2)(a).
Modifications under the Private Health Insurance (Health Benefits Fund Enforcement) Rules
(4) If an *application provision contains a power for the Private Health Insurance (Health Benefits Fund Enforcement) Rules to modify an *applied Corporations Act provision:
(a) the power extends to modifying any regulations or other instruments, in force for the purposes of that provision of the Corporations Act 2001, that are applied as a result of subsection (1); and
(b) the modifications (whether of the applied Corporations Act provision or of regulations or instruments referred to in paragraph (a)) that may be made include omissions, additions and substitutions.
(5) The fact that provision is made in this Act for a specific modification of one or more *applied Corporations Act provisions does not imply that further modifications of that provision, or any of those provisions, consistent with that specific modification, should not be made by the Private Health Insurance (Health Benefits Fund Enforcement) Rules.
Corporations Act definitions and interpretation principles
(6) The definitions and interpretation principles that have effect in or under the Corporations Act 2001 have the same effect in relation to:
(a) an *applied Corporations Act provision; or
(b) a provision of regulations or another instrument that is applied as a result of subsection (1);
as that provision applies for the purposes of a provision of this Division, unless a contrary intention appears in an *application provision or in a modification made by the Private Health Insurance (Health Benefits Fund Enforcement) Rules.
Things that may be done under regulations under the Corporations Act
(7) If an *applied Corporations Act provision allows something to be done in or by regulations, then:
(a) the Private Health Insurance (Health Benefits Fund Enforcement) Rules may do that thing for the purposes of the applied Corporations Act provision; and
(b) if they do, any regulations or instruments that are applied as a result of subsection (1) are ineffective, for the purposes of this Division, to the extent that they are inconsistent with the provisions of the Private Health Insurance (Health Benefits Fund Enforcement) Rules that do that thing.
Division 220—Ordering the termination of health benefits funds
220‑1 Applications by external managers to the Federal Court
(1) If, under paragraph 217‑55(2)(b), the Council directs the *external manager to apply under this subsection for the appointment of a *terminating manager of the *health benefits funds of a private health insurer, the external manager must apply to the Federal Court for an order or orders to give effect to such an appointment.
(2) The Council and any other person likely to be affected by the termination of the funds are entitled to be heard on the application.
220‑5 Orders made on applications for appointments of terminating managers
(1) On an application under subsection 220‑1(1), or under paragraph 217‑55(4)(b), the Federal Court may make an order for the appointment of a *terminating manager of the *health benefits funds of a private health insurer, and any related orders.
(2) However, the Federal Court must not do so unless it considers the orders to be, in the circumstances, in the interests of the *policy holders of the funds.
220‑10 Binding nature of Court orders
Any orders made by the Federal Court under section 220‑5:
(a) are binding on all persons; and
(b) take effect despite anything in the constitution or *rules of the *responsible insurer of the funds concerned.
If the Federal Court orders the appointment of a *terminating manager of the *health benefits funds of a private health insurer, the Council must notify the insurer in writing of the person appointed as the terminating manager.
230‑1 What this Chapter is about
This Chapter:
(a) provides for the Private Health Insurance Ombudsman to deal with complaints and conduct investigations;
(b) provides for the powers, functions and duties of the Private Health Insurance Administration Council;
(c) deals with some general administrative matters relating to the incentives schemes in Part 2‑2;
(d) deals with some general aspects of external and terminating managers (relevant to Divisions 149 and 217);
(e) deals with administration and collection of private health insurance levies;
(f) provides for the Private Health Insurance Risk Equalisation Trust Fund;
(g) protects information obtained for the purposes of this Act and sets out the circumstances in which such information may be used;
(h) provides for review by the Administrative Appeals Tribunal of certain decisions made under this Act;
(i) provides for miscellaneous other matters such as delegations, the approval of forms and the making of Private Health Insurance Rules and regulations.
Part 6‑2—Private Health Insurance Ombudsman
235‑1 Principal object of this Part
The principal object of this Part is to establish the office of, and set out the powers and functions of, the Private Health Insurance Ombudsman so that he or she may protect the interests of people who are covered by private health insurance by:
(a) assisting people who have made complaints relating to private health insurance to resolve those complaints; and
(b) investigating the practices and procedures of private health insurers, *private health insurance brokers and *health care providers; and
(c) mediating between private health insurers and health care providers; and
(d) disseminating information about private health insurance and the rights and obligations of privately insured people.
235‑5 Private Health Insurance (Ombudsman) Rules
Matters relevant to this Part are also dealt with in the Private Health Insurance (Ombudsman) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Ombudsman) Rules are made by the Minister under section 333‑20.
Division 238—Establishment and functions
238‑1 Establishment of office of Private Health Insurance Ombudsman
For the purposes of this Act, there is to be a Private Health Insurance Ombudsman.
Note: See Division 253 for matters relating to the office of Private Health Insurance Ombudsman.
238‑5 Functions of Private Health Insurance Ombudsman
The Private Health Insurance Ombudsman has the following functions:
(a) dealing with complaints under Division 241;
(b) conducting investigations under Division 244;
(c) publishing (in written form and on the Private Health Insurance Ombudsman’s website) a report, called the State of the Health Funds Report, as soon as practicable after the end of each financial year providing comparative information on the performance and service delivery of all private health insurers during that financial year;
(d) collecting and publishing (in written form and on the Internet) information about the *complying health insurance products available to people, in order to assist people to understand the entitlements and benefits available under those products;
(e) publishing, in aggregate form, information (not *personal information) about complaints under Division 241;
(f) reporting and making recommendations to the Minister under sections 241‑60 and 244‑15;
(g) reporting to the Minister or to the Department about the practices of particular private health insurers or *private health insurance brokers;
(h) reporting (as part of reports mentioned in paragraph (g)) to the Minister or to the Department about the practices of particular *health care providers, to the extent to which those practices relate to:
(i) the application of *private health insurance arrangements or classes of private health insurance arrangements to services or goods provided, or to goods manufactured or supplied, by the health care providers; or
(ii) private health insurance arrangements or classes of private health insurance arrangements to which those kinds of health care providers may be party;
(i) making recommendations to the Minister or the Department about regulatory practices or industry practices relating to private health insurers or private health insurance brokers;
(j) making recommendations (as part of recommendations mentioned in paragraph (i)) to the Minister or to the Department about regulatory practices or industry practices relating to health care providers, to the extent to which those practices relate to:
(i) the application of private health insurance arrangements or classes of private health insurance arrangements to services or goods provided, or to goods manufactured or supplied, by the health care providers; or
(ii) private health insurance arrangements or classes of private health insurance arrangements to which those kinds of health care providers may be party;
(k) promoting a knowledge and understanding of the Private Health Insurance Ombudsman’s functions;
(l) any other functions that are incidental to the performance of any of the preceding functions.
Subdivision 241‑A—Relevant complaints
241‑1 Who may make a complaint
(1) A complaint may be made to the Private Health Insurance Ombudsman by any of the following:
(a) a person who is, or was at the time of the incident to which the complaint relates, insured or seeking to be insured under a *private health insurance policy;
(b) a private health insurer;
(c) a *health care provider;
(d) a *private health insurance broker.
(2) A complaint may be made by a person on behalf of a person mentioned in subsection (1).
241‑5 Persons against whom complaints may be made
A complaint may be made to the Private Health Insurance Ombudsman against any of the following:
(a) a private health insurer;
(b) a *health care provider;
(c) a *private health insurance broker.
(1) The complaint may be about:
(a) any matter arising out of or connected with a *private health insurance arrangement; or
(b) any matter arising out of or connected with Chapter 2.
(2) A complaint against a *health care provider must, in addition to being about a matter in subsection (1), also:
(a) be about either or both of the following:
(i) the application of a *private health insurance arrangement to goods or a service provided, or goods manufactured or supplied, by the health care provider;
(ii) a private health insurance arrangement to which the health care provider is, or was at the time of the incident to which the complaint relates, a party; and
(b) satisfy at least one of the following:
(i) the complaint must also be made against a private health insurer;
(ii) the complainant must be a private health insurer or a person insured under a *private health insurance policy;
(iii) if the complainant is another health care provider or a *private health insurance broker—a private health insurer or a person insured under a private health insurance policy must also be a complainant in relation to the complaint.
(3) The Private Health Insurance (Ombudsman) Rules may specify matters about which complaints cannot be made.
Subdivision 241‑B—Dealing with complaints
241‑15 Initial receipt of complaint
On receiving a complaint, the Private Health Insurance Ombudsman may:
(a) inform the subject of the complaint of the nature of the complaint; and
(b) request information from the subject under Division 250.
241‑20 Ways of dealing with complaints
(1) The Private Health Insurance Ombudsman may deal with a complaint by:
(a) conducting mediation under Division 247; or
(b) referring the complaint to the subject of the complaint under Subdivision 241‑C; or
(c) if section 241‑45 applies—investigating the complaint under Subdivision 241‑D.
(2) The Private Health Insurance Ombudsman must not take any action mentioned in subsection (1) unless the complainant agrees to the action being taken.
(3) The Private Health Insurance Ombudsman must not take, or continue to take, any action mentioned in paragraph (1)(a) or (c) if the complainant withdraws the complaint.
(4) The Private Health Insurance Ombudsman must not take any action mentioned in subsection (1) if the complaint is about a matter specified in the Private Health Insurance (Ombudsman) Rules for the purposes of subsection 241‑10(3).
241‑25 Referral to the Australian Competition and Consumer Commission
(1) If, in the Private Health Insurance Ombudsman’s opinion, a complaint raises a matter that could be dealt with more effectively or conveniently by the Australian Competition and Consumer Commission, the Private Health Insurance Ombudsman must, subject to subsections (2) and (3), refer the matter to the Australian Competition and Consumer Commission.
(2) The Private Health Insurance Ombudsman must not refer the matter to the Australian Competition and Consumer Commission unless the complainant agrees to the referral.
(3) The Private Health Insurance Ombudsman must not refer the matter to the Australian Competition and Consumer Commission if the complainant withdraws the complaint.
(4) If the Private Health Insurance Ombudsman refers the matter to the Australian Competition and Consumer Commission, the Private Health Insurance Ombudsman must:
(a) tell the complainant of the matter’s referral; and
(b) give the Australian Competition and Consumer Commission any information or documents that relate to the complaint and that are in the Private Health Insurance Ombudsman’s possession or under his or her control.
(5) The Australian Competition and Consumer Commission may investigate the matter. If it does, it must, within 30 days after the referral, report to the Private Health Insurance Ombudsman on:
(a) the conduct of the investigation; and
(b) any findings that it has made as a result of the investigation.
(6) If the Australian Competition and Consumer Commission decides not to investigate the matter, it must, within 30 days after the referral, give the Private Health Insurance Ombudsman a written notice informing the Private Health Insurance Ombudsman of its decision and of the reasons for its decision.
241‑30 Referral to other bodies
(1) If, in the Private Health Insurance Ombudsman’s opinion, a complaint raises a matter that could be dealt with more effectively or conveniently by another body, the Private Health Insurance Ombudsman must, subject to this section, refer the matter to that body.
(2) The Private Health Insurance Ombudsman must not refer the matter to the other body unless the complainant agrees to the referral.
(3) The Private Health Insurance Ombudsman must not refer the matter to the other body if the complainant withdraws the complaint.
241‑35 Deciding not to deal with a complaint
(1) The Private Health Insurance Ombudsman may decide not to deal, or not to continue to deal, with a complaint in accordance with this section. If the Private Health Insurance Ombudsman so decides, he or she must:
(a) tell the complainant of the decision and the reasons for the decision; and
(b) if requested by the complainant—give the complainant written notice of the decision and the reasons for the decision.
(2) The Private Health Insurance Ombudsman may decide not to take any action in relation to a complaint if the incident to which the complaint relates occurred more than 12 months before the complaint is made.
(3) The Private Health Insurance Ombudsman may decide not to deal with a complaint if he or she is satisfied that the complainant has not taken reasonable steps to negotiate a settlement of the complaint with the subject of the complaint.
(4) The Private Health Insurance Ombudsman may decide not to deal, or not to continue to deal, with a complaint if the complainant does not agree to a matter relating to the complaint being referred to another body under section 241‑30.
(5) The Private Health Insurance Ombudsman may decide not to deal, or not to continue to deal, with a complaint, if he or she believes that:
(a) the subject of the complaint has dealt, or is dealing, adequately with the complaint, or has not yet had an adequate opportunity to do so; or
(b) the Private Health Insurance Ombudsman has dealt adequately with the complaint; or
(c) the complainant is capable of assisting the Private Health Insurance Ombudsman in dealing with the complaint but does not do so on request; or
(d) the complainant does not have a sufficient interest in the subject matter of the complaint; or
(e) the matter is trivial; or
(f) the complaint is frivolous or vexatious or was not made in good faith; or
(g) the complaint is mainly about commercial negotiations and, having regard to the object of this Part, it is not appropriate to deal, or to continue to deal, with the complaint; or
(h) the complaint is mainly about clinical matters and, having regard to the object of this Part, it is not appropriate to deal, or continue to deal, with the complaint; or
(i) the complainant has exercised, or exercises, a right to have the matter to which the complaint relates reviewed by a court or tribunal constituted by or under a law of the Commonwealth or of a State or Territory; or
(j) both:
(i) the complainant has, or had, a right to have the matter to which the complaint relates reviewed by a court or by a tribunal constituted by or under a law of the Commonwealth or of a State or Territory, but has not exercised that right; and
(ii) it is, or would have been, reasonable for the complainant to exercise that right.
Subdivision 241‑C—Referral to subjects of complaints
241‑40 Referral to the subject of the complaint
(1) The Private Health Insurance Ombudsman may, at any time and whether or not mediation has been conducted under Division 247, refer a complaint to the subject of the complaint and request the subject:
(a) to investigate the complaint; and
(b) to report to the Private Health Insurance Ombudsman on the outcome of the investigation and any action that the subject proposes to take as a result, before the end of the period specified in the request.
Note: The Private Health Insurance Ombudsman must have the complainant’s agreement to act under this section (see subsection 241‑20(2)).
(2) The subject may, before the end of the period specified in the request, ask the Private Health Insurance Ombudsman to extend that period.
(3) If the Private Health Insurance Ombudsman refuses the request, the Private Health Insurance Ombudsman must give his or her reasons for refusing.
Note: A refusal to extend the period is reviewable under Part 6‑9.
Subdivision 241‑D—Investigation of complaints
241‑45 Investigation of complaint
The Private Health Insurance Ombudsman may investigate a complaint if:
(a) the complaint is not resolved to the complainant’s satisfaction by mediation under Division 247; or
(b) the Private Health Insurance Ombudsman is not satisfied with the outcome of a referral under Subdivision 241‑C.
Note: The Private Health Insurance Ombudsman must have the complainant’s agreement to act under this section and cannot continue if the complaint is withdrawn (see subsections 241‑20(2) and (3)).
(1) If the Private Health Insurance Ombudsman decides under section 241‑35 not to investigate, or not to continue to investigate, a complaint made by a person, the person may apply, in writing, to the Minister for a direction by the Minister to the Private Health Insurance Ombudsman to investigate, or to continue to investigate, the complaint.
(2) If the Minister directs the Private Health Insurance Ombudsman to do so, the Private Health Insurance Ombudsman must:
(a) investigate, or continue to investigate, the complaint; and
(b) report to the Minister under section 241‑60 on the findings of his or her investigation.
Subdivision 241‑E—Recommendations and reports
241‑55 Recommendations as a result of referral or investigation
(1) The Private Health Insurance Ombudsman may make recommendations under this section after:
(a) receiving a report from the subject of a complaint after referral under Subdivision 241‑C; or
(b) investigating a complaint under Subdivision 241‑D.
(2) The Private Health Insurance Ombudsman may recommend any or all of the following:
(a) to a private health insurer, that the insurer take a specific course of action in relation to the complaint or make changes to its *rules, or both;
(b) to a private health insurer, that the insurer request a *health care provider or *private health insurance broker to take a specific course of action in relation to the complaint;
(c) to a health care provider or private health insurance broker, that the provider or broker take a specific course of action in relation to the complaint.
(3) The Private Health Insurance Ombudsman may request the person to whom the recommendation was made, or an *officer of that person, to report to the Private Health Insurance Ombudsman, before action is taken to give effect to the recommendation, on the action proposed to be taken. The request must specify the period within which the report is to be given.
(4) A person commits an offence if:
(a) a request is made of the person under subsection (3); and
(c) the person does not comply with the request.
Penalty: 30 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
241‑60 Report to Minister on outcome of investigation under Subdivision 241‑D
(1) The Private Health Insurance Ombudsman may report and make recommendations under this section after completing an investigation of a complaint against a particular subject under Subdivision 241‑D.
(2) The Private Health Insurance Ombudsman may report to the Minister on the outcome of the investigation (including any recommendations made to the subject of the complaint and any responses to those recommendations).
(3) The Private Health Insurance Ombudsman may recommend to the Minister either or both of the following:
(a) general changes in regulatory practice or industry practices relating to the kind of subject of complaint;
(b) possible means of dealing with specific problems arising in relation to the particular subject of the complaint.
(4) The Private Health Insurance Ombudsman may make recommendations under paragraph (3)(b) concerning *health care providers or a particular health care provider only to the extent to which the recommendations relate to:
(a) the application of a *private health insurance arrangement or a class of private health insurance arrangements to services or goods provided, or goods manufactured or supplied, by that kind of health care provider; or
(b) a private health insurance arrangement or a class of private health insurance arrangements to which that kind of health care provider may be party.
(5) Before reporting to the Minister under this section, the Private Health Insurance Ombudsman must:
(a) inform the subject of the complaint that the Private Health Insurance Ombudsman proposes to make the report and of the nature of any criticism of the subject’s conduct that will appear in the report; and
(b) invite the subject to comment on such criticism, before the end of the period specified in the invitation.
The Private Health Insurance Ombudsman must include in the report any comments made by the subject.
Subdivision 241‑F—Miscellaneous
241‑65 Complainant to be kept informed
(1) The Private Health Insurance Ombudsman must keep the complainant informed about the Private Health Insurance Ombudsman’s handling of the complaint.
(2) The Private Health Insurance Ombudsman must inform the complainant in writing of:
(a) any action taken by a private health insurer, a *health care provider or *private health insurance broker as a result of the Private Health Insurance Ombudsman’s handling of the complaint; and
(b) any recommendations made by the Private Health Insurance Ombudsman under section 241‑55;
and the reasons for the action or recommendation.
Subdivision 244‑A—Investigations
244‑1 Initiating investigations
(1) The Private Health Insurance Ombudsman may, on his or her own initiative, investigate the practices and procedures of a private health insurer or a *private health insurance broker.
(2) The Private Health Insurance Ombudsman may, on his or her own initiative, investigate the practices and procedures of a *health care provider together with an investigation of a private health insurer under subsection (1), if:
(a) the investigation relates to a matter arising out of or connected with a *private health insurance arrangement; and
(b) the practices and procedures relate to either or both of the following:
(i) the application of a private health insurance arrangement to services or goods provided, or to goods manufactured or supplied, by the health care provider;
(ii) a private health insurance arrangement to which the health care provider is, or was in the period to be investigated, a party; and
(c) the Private Health Insurance Ombudsman considers, having regard to the object of this Part, that investigation of the health care provider together with the private health insurer is necessary or appropriate in order to consider the matter effectively.
Note: An investigation may include mediation (see section 247‑1).
244‑5 Investigations at Minister’s request
(1) The Minister may request the Private Health Insurance Ombudsman to investigate the practices and procedures of a private health insurer or a *private health insurance broker.
(2) The Minister may request the Private Health Insurance Ombudsman to investigate the practices and procedures of a *health care provider together with an investigation of a private health insurer under subsection (1), if:
(a) the investigation relates to a matter arising out of or connected with a *private health insurance arrangement; and
(b) the practices and procedures relate to either or both of the following:
(i) the application of a private health insurance arrangement to services or goods provided, or to goods manufactured or supplied, by the health care provider;
(ii) a private health insurance arrangement to which the health care provider is, or was in the period to be investigated, a party; and
(c) the Minister considers, having regard to the object of this Part, that investigation of the health care provider together with the private health insurer is necessary or appropriate in order to consider the matter effectively.
(3) If the Minister makes a request under this section, the Private Health Insurance Ombudsman must conduct an investigation.
Note: An investigation may include mediation (see section 247‑1).
Subdivision 244‑B—Recommendations and reports
244‑10 Recommendations as a result of investigation
(1) The Private Health Insurance Ombudsman may make recommendations under this section after conducting an investigation under this Division.
(2) The Private Health Insurance Ombudsman may recommend either or both of the following:
(a) to a private health insurer, that the insurer take a specific course of action or make changes to its *rules, or both;
(b) to a *health care provider or *private health insurance broker, that the provider or broker take a specific course of action.
(3) The Private Health Insurance Ombudsman may request the person to whom the recommendation was made, or an *officer of that person, to report to the Private Health Insurance Ombudsman, before action is taken to give effect to the recommendation, on the action proposed to be taken. The request must specify the period within which the report is to be given.
(4) A person commits an offence if:
(a) a request is made of the person under subsection (3); and
(b) the person does not comply with the request.
Penalty: 30 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
244‑15 Report to Minister on outcome of investigations under this Division
(1) The Private Health Insurance Ombudsman may, after completing an investigation under section 244‑1, and must after completing an investigation under section 244‑5:
(a) report to the Minister on the outcome of the investigation and any mediation conducted as part of the investigation (including any recommendations made to the subject of the investigation); and
(b) make recommendations to the Minister:
(i) concerning general changes in regulatory practice or industry practices relating to that kind of subject of investigation; or
(ii) concerning possible means of dealing with specific problems arising in relation to the particular subject of the investigation.
(2) The Private Health Insurance Ombudsman may make recommendations under paragraph (1)(b) concerning *health care providers or a particular health care provider only to the extent to which the recommendations relate to:
(a) the application of a *private health insurance arrangement or a class of private health insurance arrangements to services or goods provided, or to goods manufactured or supplied, by that kind of health care provider; or
(b) a private health insurance arrangement or a class of private health insurance arrangements to which that kind of health care provider may be party.
(3) Before reporting to the Minister under this section, the Private Health Insurance Ombudsman must:
(a) inform the subject of the investigation that the Private Health Insurance Ombudsman proposes to make the report and of the nature of any criticism of the conduct of the subject that will appear in the report; and
(b) invite the subject to comment on such criticism, before the end of the period specified in the invitation.
The Private Health Insurance Ombudsman must include in the report any comments made by the subject.
244‑20 Consultation with Australian Competition and Consumer Commission
If the Private Health Insurance Ombudsman considers, as a result of an investigation under this Division, that there might have been conduct in the nature of a restrictive trade practice for the purposes of the Trade Practices Act 1974, the Private Health Insurance Ombudsman must consult with the Australian Competition and Consumer Commission and have regard to the advice of the Australian Competition and Consumer Commission on the matter before reporting on it under section 244‑15.
(1) The Private Health Insurance Ombudsman may, at any time, try to settle a complaint made under Division 241 by mediating between the complainant and the subject of the complaint.
(2) The Private Health Insurance Ombudsman may, if he or she considers it appropriate and consistent with the object of this Part, try to resolve a matter being investigated under Division 244 by mediating between a private health insurer and a *health care provider.
(3) A party’s participation in the mediation may be:
(a) voluntary; or
(b) required by a direction given to the party by the Private Health Insurance Ombudsman under section 247‑5.
Note: If mediating a complaint, the Private Health Insurance Ombudsman must have the complainant’s agreement to act under this section and cannot continue if the complaint is withdrawn (see subsections 241‑20(2) and (3)).
247‑5 Participation in mediation may be compulsory
(1) The Private Health Insurance Ombudsman may direct:
(a) the subject of a complaint made under Division 241; or
(b) a private health insurer that is the subject of an investigation under Division 244; or
(c) a *health care provider that is the subject of an investigation under Division 244;
to participate in mediation under section 247‑1.
(2) The Private Health Insurance (Ombudsman) Rules may set out matters to which the Private Health Insurance Ombudsman is to have regard when deciding whether or not to give a direction under subsection (1).
(3) The direction must:
(a) be in writing; and
(b) name either or both of the following:
(i) the subject of the complaint or investigation;
(ii) an *officer, or officers, of that subject; and
(c) be given to those named in it; and
(d) specify the time of the mediation, which must not be earlier than 14 days after the day on which the direction is given; and
(e) specify the place of the mediation.
Note: Subsection 33(3) of the Acts Interpretation Act 1901 has the effect that the direction may be varied or revoked.
(4) A person commits an offence if:
(a) the person is named in a direction under subsection (1); and
(b) the other party to the mediation attends, or was willing to attend, the mediation; and
(c) the person, or, if the person is a *medical practitioner who has appointed a representative in relation to the mediation under section 247‑10, the person’s representative, fails to participate in part or all of the mediation.
Penalty: 30 penalty units.
247‑10 Medical practitioners may appoint representatives
(1) If the Private Health Insurance Ombudsman directs a *medical practitioner under subsection 247‑5(1) to participate in mediation, the medical practitioner may appoint an individual to participate in the mediation on the practitioner’s behalf.
(2) The appointment must be:
(a) in writing; and
(b) signed by the *medical practitioner; and
(c) made before the mediation starts.
247‑15 Conduct of compulsory mediation
(1) If the Private Health Insurance Ombudsman directs a party to participate in mediation, the mediation may be conducted by:
(a) the Private Health Insurance Ombudsman; or
(b) a person appointed by the Private Health Insurance Ombudsman under section 247‑25.
(2) Mediation in which a party is directed to participate ceases:
(a) if the parties agree to settle the matter; or
(b) if the Private Health Insurance Ombudsman concludes that the matter cannot be settled by mediation.
(3) The Private Health Insurance (Ombudsman) Rules may set out matters to which the Private Health Insurance Ombudsman is to have regard before concluding that a matter cannot be settled by mediation.
(4) A person appointed by the Private Health Insurance Ombudsman under section 247‑25 to conduct mediation must, as soon as practicable after the mediation is conducted or should have been conducted, report to the Private Health Insurance Ombudsman about:
(a) whether the mediation was conducted; and
(b) if the mediation failed—the reasons for the failure; and
(c) if the parties agreed to settle the complaint—the terms of the settlement, including any action to be taken.
247‑20 Admissibility of things said in mediation
(1) Evidence of anything said, or any admission made, during participation in mediation under section 247‑1 is not admissible:
(a) in any court (whether exercising federal jurisdiction or not); or
(b) in any proceedings before a person authorised by a law of the Commonwealth or of a State or Territory, or by the consent of the parties, to hear evidence.
(2) This section applies whether or not a party is directed to participate in the mediation.
247‑25 Appointment of mediators
(1) The Private Health Insurance Ombudsman may appoint a person to conduct mediation in which a person is or will be directed to participate under section 247‑5.
(2) The Private Health Insurance (Ombudsman) Rules may set out matters to which the Private Health Insurance Ombudsman is to have regard when appointing a person under this section.
(3) The person is appointed for the period specified by the Private Health Insurance Ombudsman in the instrument of appointment.
(4) Subject to Division 323 (disclosure of information), the person is not personally liable to an action or other proceeding for damages in relation to anything done or omitted to be done, reasonably and in good faith, in or in relation to the conduct of the mediation.
Division 250—Information‑gathering
Information‑gathering for Division 241 complaints
(1) The Private Health Insurance Ombudsman may, for the purposes of:
(a) deciding if, and how, to deal with a complaint made under Division 241; or
(b) mediating a complaint made under Division 241; or
(c) investigating a complaint made under Division 241; or
(d) evaluating action proposed by the subject of a complaint after referral of the complaint to the subject under Subdivision 241‑C;
request the subject of the complaint, or an *officer of the subject, to give the Private Health Insurance Ombudsman the *records of the subject (relating to the complaint) that are specified in the request, before the end of the period specified in the request.
Information‑gathering for Division 244 investigations
(2) The Private Health Insurance Ombudsman may, for the purposes of an investigation under Division 244 (including mediating as part of the investigation under Division 247), request the subject of the investigation, or an *officer of the subject:
(a) to give the Private Health Insurance Ombudsman the information (relating to the practices and procedures being investigated) that is specified in the request; or
(b) to give the Private Health Insurance Ombudsman the *records of the subject (relating to the practices and procedures being investigated) that are specified in the request;
before the end of the period specified in the request.
General provisions about information‑gathering
(3) The Private Health Insurance Ombudsman may make one or more requests under subsection (1) or (2) in relation to a complaint or investigation, at any time while the Private Health Insurance Ombudsman is dealing with the complaint or investigation.
(4) A person to whom a request is made under subsection (1) or (2) may, before the end of the period specified in the request, ask the Private Health Insurance Ombudsman to extend the period specified in the request.
(5) If the Private Health Insurance Ombudsman refuses to extend the period, the Private Health Insurance Ombudsman must give his or her reasons for refusing.
Note: A refusal to extend the period is reviewable under Part 6‑9.
(6) A person is not excused from giving information or producing a *record when required to do so under subsection (1) or (2) on the ground that the giving of the information, or the production of the record, might tend to incriminate the person or make the person liable to a penalty. However, the giving of the information, or the production of the record, or anything obtained as a direct or indirect consequence of the giving or production, is not admissible in evidence against the person in any proceedings, other than proceedings for an offence against section 137.1 or 137.2 of the Criminal Code.
(7) A person commits an offence if:
(a) a request is made to the person under subsection (1) or (2); and
(b) the person fails to comply with the request by the end of the period specified in the request or, if that period has been extended, by the end of the extended period.
Penalty: 30 penalty units.
(8) Strict liability applies to subsection (7).
Note: For strict liability, see section 6.1 of the Criminal Code.
250‑5 Limits on information‑gathering
(1) A request made to the subject of a complaint, or an *officer of the subject of a complaint, under subsection 250‑1(1) must not request *records that relate to the subject’s dealings with the complainant unless the complainant consents to the records being given.
(2) A request made to a private health insurer, or an *officer of a private health insurer, under subsection 250‑1(2) must not request information or *records that relate to a particular individual who is or was insured, or is or was seeking to be insured, under a *private health insurance policy of the insurer, unless the individual consents to the records or information being given.
(3) A request made to a *health care provider, or an *officer of a health care provider, under subsection 250‑1(2) must not request information or *records that relate to a particular individual who is or was a patient of the health care provider, unless the individual consents to the information or records being given.
(4) A request made to a *private health insurance broker, or an *officer of a private health insurance broker, under subsection 250‑1(2) must not request information or *records that relate to a particular individual who is or was a client of the broker unless the individual consents to the information or records being given.
250‑10 Disclosure of personal information
(1) This section applies if a person gives a *record, information or a document to the Private Health Insurance Ombudsman, reasonably believing that this would assist the Private Health Insurance Ombudsman in:
(a) mediating a complaint under Division 247 or otherwise dealing with it under Subdivision 241‑B or 241‑D; or
(b) referring a complaint under section 241‑25 or 241‑30; or
(c) making a decision under section 241‑35 not to deal, or not to continue to deal, with a complaint; or
(d) investigating a matter under section 244‑1 or 244‑5.
(2) For the purposes of:
(a) the Privacy Act 1988; and
(b) any provision of a law of a State or Territory that provides that *personal information contained in a *record, information or document may be disclosed if the disclosure is authorised by law;
the giving of the record, information or document to the Private Health Insurance Ombudsman is taken to be authorised by law.
Division 253—Provisions relating to the Private Health Insurance Ombudsman
253‑1 Appointment of the Private Health Insurance Ombudsman
(1) The Private Health Insurance Ombudsman is to be appointed by the Minister, by written instrument, in accordance with any Private Health Insurance (Ombudsman) Rules.
(2) The Private Health Insurance Ombudsman may be appointed on a full‑time or a part‑time basis.
(3) The Private Health Insurance Ombudsman holds office on the terms and conditions (if any) in relation to matters not covered by this Act that are determined by the Minister.
253‑5 Validity of appointments
The appointment of a person as Private Health Insurance Ombudsman is not invalid merely because there was a defect or irregularity in connection with the appointment.
(1) The Minister may appoint a person to act as the Private Health Insurance Ombudsman:
(a) during a vacancy in the office of Private Health Insurance Ombudsman (whether or not an appointment has previously been made to the office); or
(b) during any period, or during all periods, when the Private Health Insurance Ombudsman is absent from duty or from Australia or is, for any other reason, unable to perform the duties of the office.
(2) Anything done by or in relation to a person purporting to act under an appointment under this section is not invalid merely because:
(a) the occasion for the appointment had not arisen; or
(b) there was a defect or irregularity in connection with the appointment; or
(c) the appointment had ceased to have effect; or
(d) the occasion to act had not arisen or had ceased.
253‑15 Remuneration and allowances
(1) The Private Health Insurance Ombudsman is to be paid the remuneration that is determined by the Remuneration Tribunal. If no determination of that remuneration by the Tribunal is in operation, the Private Health Insurance Ombudsman is to be paid the remuneration that is specified in the Private Health Insurance (Ombudsman) Rules.
(2) The Private Health Insurance Ombudsman is to be paid such allowances as are set out in the Private Health Insurance (Ombudsman) Rules.
(3) This section has effect subject to the Remuneration Tribunal Act 1973.
(1) A person who holds the office of Private Health Insurance Ombudsman on a full‑time basis must not engage in any paid employment outside the duties of that office without the Minister’s written approval.
(2) A person who holds the office of Private Health Insurance Ombudsman on a part‑time basis must not engage in any paid employment that, in the Minister’s opinion, conflicts with the proper performance of the Private Health Insurance Ombudsman’s functions.
(1) If the Private Health Insurance Ombudsman holds office on a full‑time basis, he or she has such recreation leave entitlements as are determined by the Remuneration Tribunal.
(2) The Minister may grant the Private Health Insurance Ombudsman leave of absence, other than recreational leave, on such terms and conditions as to remuneration or otherwise as the Minister determines in writing.
The Private Health Insurance Ombudsman may resign his or her appointment by giving the Minister a written resignation.
253‑35 Termination of appointment
(1) The Minister may terminate the Private Health Insurance Ombudsman’s appointment for misbehaviour or physical or mental incapacity.
(2) The Minister must terminate the Private Health Insurance Ombudsman’s appointment if the Private Health Insurance Ombudsman:
(a) becomes bankrupt, applies to take the benefit of any law for the relief of bankrupt or insolvent debtors, compounds with creditors or makes an assignment of remuneration for their benefit; or
(b) is appointed on a full‑time basis and is absent from duty, except on leave of absence, for 14 consecutive days or for 28 days in any 12 months; or
(c) is appointed on a full‑time basis and engages, except with the Minister’s approval, in paid employment outside the duties of his or her office; or
(d) is appointed on a part‑time basis and engages in paid employment that, in the Minister’s opinion, conflicts with the proper performance of his or her duties; or
(e) fails, without reasonable excuse, to comply with section 253‑40.
253‑40 Disclosure of interest by Private Health Insurance Ombudsman
If the Private Health Insurance Ombudsman has a material personal interest in a matter that the Private Health Insurance Ombudsman is considering or about to consider, the Private Health Insurance Ombudsman must give written notice of the interest to the Minister.
253‑45 Statutory agency etc. for purposes of Public Service Act
(1) The staff required to assist the Private Health Insurance Ombudsman are to be persons engaged under the Public Service Act 1999.
(2) For the purposes of the Public Service Act 1999:
(a) the Private Health Insurance Ombudsman and the APS employees assisting him or her together constitute a Statutory Agency; and
(b) the Private Health Insurance Ombudsman is the Head of that Statutory Agency.
(1) The Private Health Insurance Ombudsman must, as soon as practicable after the end of each financial year, prepare and give to the Minister, for presentation to the Parliament, a report on the operations during that year of the office of the Private Health Insurance Ombudsman.
Note: See also section 34C of the Acts Interpretation Act 1901, which contains extra rules about annual reports.
(2) The Private Health Insurance Ombudsman must include in the report:
(a) the number and nature of complaints received under section 241‑1; and
(b) the outcomes of any actions taken, recommendations made or investigations conducted in relation to such complaints; and
(c) the outcomes in relation to complaints referred to another body under section 241‑30; and
(d) investigations (if any) conducted by the Private Health Insurance Ombudsman under section 244‑1; and
(e) requests (if any) by the Minister under section 244‑5 that the Private Health Insurance Ombudsman conduct an investigation; and
(f) the outcomes of investigations conducted under sections 244‑1 and 244‑5.
The Private Health Insurance Ombudsman may, by writing, delegate to a member of staff referred to in section 253‑45 all or any of the Private Health Insurance Ombudsman’s powers and functions under this Act.
253‑60 Private Health Insurance Ombudsman and staff not personally liable
Subject to Division 323 (disclosure of information), neither the Private Health Insurance Ombudsman nor a member of staff referred to in section 253‑45 is personally liable to an action or other proceeding for damages in relation to anything done or omitted to be done reasonably and in good faith:
(a) in the performance or purported performance of any function of the Private Health Insurance Ombudsman; or
(b) in the exercise or purported exercise of any power of the Private Health Insurance Ombudsman.
256‑1 Protection from civil actions
Civil proceedings do not lie against a person in respect of loss, damage or injury of any kind suffered by another person because a statement was made, or information or a document given, in good faith to the Private Health Insurance Ombudsman in connection with:
(a) the making of a complaint under Division 241; or
(b) the Private Health Insurance Ombudsman’s handling of such a complaint; or
(c) an investigation under Division 244.
A person commits an offence if:
(a) the person subjects, or threatens to subject, another person to detriment; and
(b) the person does so because the other person has made, or proposes to make, a complaint under this Part.
Penalty: Imprisonment for 6 months.
256‑10 Giving information about the Private Health Insurance Ombudsman
(1) The Private Health Insurance Ombudsman may direct private health insurers:
(a) to give *adults insured under the insurers’ *products the information specified in the direction, in the manner specified in the direction; or
(b) to publish the information specified in the direction, in the manner specified in the direction.
(2) A direction must only specify information that relates to the functions of the Private Health Insurance Ombudsman.
(3) If more than one *adult is insured under a single *complying health insurance policy of a private health insurer, the insurer is taken to comply with a direction if the insurer complies with the direction in relation to only one of those adults.
(4) A private health insurer commits an offence if:
(a) the Private Health Insurance Ombudsman gives private health insurers a direction under subsection (1); and
(b) the insurer does not comply with the direction.
Penalty: 60 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
Part 6‑3—Private Health Insurance Administration Council
The Private Health Insurance Administration Council continues in existence with functions and powers relating largely to the regulation of private health insurers through the administration of Chapter 4 and Part 5‑3.
261‑5 The Private Health Insurance (Council) Rules
The Private Health Insurance Administration Council is also dealt with in the Private Health Insurance (Council) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Council) Rules are made by the Minister under section 333‑20.
Division 264—Continuation, purposes, functions and powers
264‑1 Continuation of the Council
(1) The Private Health Insurance Administration Council established under section 82B of the National Health Act 1953 continues in existence by force of this section, under and subject to the provisions of this Act.
(2) The Council:
(a) is a body corporate with perpetual succession; and
(b) must have a common seal; and
(c) may acquire, hold and dispose of real and personal property; and
(d) may sue and be sued in its corporate name.
Note: The Commonwealth Authorities and Companies Act 1997 applies to the Council (subject to section 267‑20). That Act deals with matters relating to Commonwealth authorities, including reporting and accountability, banking and investment, and conduct of officers.
(3) The common seal of the Council must be kept in such custody as the Council directs and must not be used except as authorised by the Council.
(4) All courts, judges and persons acting judicially must:
(a) take judicial notice of the imprint of the common seal of the Council appearing on a document; and
(b) presume that the document was duly sealed.
264‑5 Objectives of the Council
In performing its functions and exercising its powers, the Council must take all reasonable steps to achieve an appropriate balance between the following objectives:
(a) fostering an efficient and competitive health insurance industry;
(b) protecting the interests of consumers;
(c) ensuring the prudential safety of individual private health insurers.
264‑10 Functions of the Council
General
(1) The functions of the Council are:
(a) to administer the *Risk Equalisation Trust Fund; and
(b) to administer the registration of private health insurers under Part 4‑3; and
(c) the information collection function under subsection (2); and
(d) the compliance functions under subsection (3); and
(e) the enforcement functions under subsection (4); and
(f) the public information functions under subsection (5); and
(g) the agency cooperation functions under subsection (6); and
(h) to advise the Minister about the financial operations and affairs of private health insurers; and
(i) functions incidental to any other functions of the Council; and
(j) any other functions conferred on the Council by this, or any other, Act.
Information collection function
(2) The information collection function of the Council is to obtain from each private health insurer regular reports about the insurer’s operations, including reports supported by actuarial certification.
Compliance functions
(3) The compliance functions of the Council are:
(a) to establish a *solvency standard and a *capital adequacy standard to be complied with by private health insurers, and to give *solvency directions and *capital adequacy directions to private health insurers; and
Note: The solvency standard and the capital adequacy standard are established by the Private Health Insurance (Health Benefits Administration) Rules.
(b) to exercise powers and discretions under the *prudential standards, and to give directions to private health insurers relating to compliance with the prudential standards; and
Note: The prudential standards are established by the Private Health Insurance (Insurer Obligations) Rules.
(c) to consider, in accordance with Division 160, whether persons should, or should not, be *appointed actuaries; and
(d) to consider, in accordance with Division 166, whether persons should, or should not, be *disqualified persons; and
(e) to examine, from time to time, the financial affairs of private health insurers, by the inspection and analysis of the records, books and accounts of the insurers and any other relevant information; and
(f) to review, by carrying out independent actuarial assessment, the value of the assets and liabilities of each *health benefits fund; and
(g) if it is necessary, for the purpose of making a proper examination of the financial affairs of a private health insurer, for the Council to incur unusually high costs—to impose an appropriate fee on the private health insurer concerned.
Enforcement functions
(4) The enforcement functions of the Council are:
(a) to take action under Part 5‑2 to monitor compliance with, and to encourage or compel compliance with, *Council‑supervised obligations; and
(b) to appoint, under section 214‑1, *inspectors for the purpose of investigating the affairs of private health insurers under Division 214, and to exercise other related powers and functions of the Council under that Division; and
(c) to appoint, under Subdivision 217‑B, persons as *external managers of *health benefits funds, and to exercise other related powers and functions of the Council under Division 217 and 220.
Public information functions
(5) The public information functions of the Council are:
(a) to make statistics, and other financial information, relating to a private health insurer or private health insurers, publicly available in accordance with the Private Health Insurance (Council) Rules; and
(b) to collect and disseminate information about private health insurance, for the purpose of enabling people to make informed choices about private health insurance.
Agency cooperation functions
(6) The agency cooperation functions of the Council are:
(a) to cooperate with other regulatory agencies on matters affecting private health insurers and the private health insurance industry generally; and
(b) to provide the Private Health Insurance Ombudsman, from time to time, with information in the Council’s possession that the Council considers likely to be of use in production of the State of the Health Funds Reports referred to in paragraph 238‑5(c).
264‑15 Report on private health insurers
(1) The Council must, as soon as practicable after 30 September in each year, give the Minister a report, for presentation to the Parliament, on the operations of private health insurers during the financial year ending on 30 June in that year.
Note: See also section 34C of the Acts Interpretation Act 1901, which contains extra rules about annual reports.
(2) The report must include, in respect of each *health benefits fund conducted by a private health insurer during the year to which the report relates, the following information:
(a) premiums payable to the fund;
(b) other amounts payable to the fund;
(c) fund benefits payable out of the fund;
(d) management expenses;
(e) other amounts payable out of the fund;
(f) the balance of the fund as at the end of that year;
(g) details of how the reserves of the fund have been invested;
(h) such other information as the Minister requires to be included.
Note: An annual report on the Council’s operations must also be prepared under section 9 of the Commonwealth Authorities and Companies Act 1997.
The Council has power to do all things necessary or convenient to be done for, or in connection with the performance of its functions.
(1) The Minister may, by legislative instrument, give directions with respect to the performance of the Council’s functions or the exercise of its powers.
(2) The Council must comply with any such direction.
(3) Before giving a direction under subsection (1), the Minister must consult the Council about the proposed direction.
Division 267—Constitution and administration
267‑1 Constitution of the Council
(1) The Council consists of the following members:
(a) a Commissioner of Private Health Insurance Administration;
(b) at least 2, and not more than 4, other members.
(2) The performance of the functions, or the exercise of the powers, of the Council is not affected only because there is a vacancy or vacancies in the membership of the Council.
(1) The *members are to be appointed in writing by the Minister.
(2) One of the *members may be appointed in writing by the Minister to be the Deputy Commissioner.
(3) Appointments must be made in accordance with the requirements (if any) specified in the Private Health Insurance (Council) Rules.
(4) The *Commissioner is to be appointed on a full‑time basis or on a part‑time basis.
(5) A *member, other than the *Commissioner, is to be appointed on a part‑time basis.
(6) If a *member is appointed as *Deputy Commissioner, that appointment is on a part‑time basis.
(7) A person cannot be appointed as a *member if that person is a *director, *officer or employee of a body regulated by the Council.
267‑10 Meetings of the Council
(1) Subject to subsection (2), the *Commissioner must convene a meeting of the Council when:
(a) the Commissioner thinks it necessary for the efficient performance of the Council’s functions; or
(b) directed to do so by written notice of the Minister; or
(c) requested in writing to do so by at least 2 *members.
(2) The *Commissioner must convene a meeting at least once every 6 months.
(3) The *Commissioner must determine the time and place at which a meeting is to be held.
(4) A majority of the *members constitutes a quorum.
(5) The *Commissioner must preside at all meetings.
(6) A question arising at a meeting is decided by a majority of the votes of the *members present and voting. The *Commissioner has a deliberative vote and, if necessary, also has a casting vote.
(7) Subject to this section, the *Commissioner must determine the procedure of the meeting.
267‑15 Delegation by the Council
The Council may, by writing under its common seal, delegate to:
(a) the *Chief Executive Officer; or
(b) another member of staff of the Council;
all or any of the functions and powers of the Council, other than functions and powers under the Commonwealth Authorities and Companies Act 1997.
267‑20 Modification of the Commonwealth Authorities and Companies Act 1997
Section 14 of the Commonwealth Authorities and Companies Act 1997 does not apply in relation to the Council.
270‑1 Terms and conditions etc.
The Private Health Insurance (Council) Rules may, subject to this Part, specify:
(a) the terms and conditions of appointment of the *Commissioner, of the other *members, and of a member as *Deputy Commissioner; and
(b) their periods of appointment.
270‑5 Validity of appointments
The appointment of a person as *Commissioner or as another *member is not invalid because of a defect or irregularity in connection with the person’s appointment.
(1) The Minister may appoint a person to act as *Commissioner:
(a) during a vacancy in the office of Commissioner (whether or not an appointment has been previously made to the office); or
(b) during any period, or during all periods, when, the Commissioner is absent from duty or from Australia or is, for any other reason, unable to perform the duties of the office;
but a person appointed to act during a vacancy must not continue to act for more than 12 months.
(2) Anything done by or in relation to a person purporting to act as *Commissioner is not invalid because:
(a) the occasion for the appointment had not arisen; or
(b) there was a defect or irregularity in connection with the appointment; or
(c) the appointment had ceased to have effect; or
(d) the occasion for the person to act as Commissioner had not arisen or had ceased.
270‑15 Deputy Commissioner to act as Commissioner in certain circumstances
(1) The *Deputy Commissioner is to act as *Commissioner:
(a) during a vacancy in the office of Commissioner (whether or not an appointment has been made to the office) if no‑one has been appointed to act as Commissioner; or
(b) during any period, or during all periods, when the Commissioner, and any person appointed to act as Commissioner, are absent from duty or from Australia or are, for any other reason, unable to perform the duties of the Commissioner.
(2) The *Deputy Commissioner must not act as *Commissioner during a vacancy in the office of Commissioner for more than 12 months.
(3) Anything done by or in relation to a person purporting to act as *Commissioner under this section is not invalid because the occasion for the person to act as Commissioner had not arisen or had ceased.
270‑20 Powers and duties of persons acting as Commissioner
(1) Subject to any direction by the *Commissioner, an acting Commissioner, or the *Deputy Commissioner when acting as Commissioner, has all the powers and functions of the Commissioner under this Act.
(2) A power or function of the *Commissioner under this Act or any other Act, when exercised or performed by an acting Commissioner, or by the *Deputy Commissioner when acting as Commissioner, is to be taken, for the purposes of this Act or any other Act, to have been exercised or performed by the Commissioner.
(3) The exercise of a power or the performance of a function of the *Commissioner under this Act or any other Act by an acting Commissioner, or by the *Deputy Commissioner when acting as Commissioner, does not prevent the exercise of the power or the performance of the function by the Commissioner.
(4) If, under this Act or any other Act:
(a) the exercise of a power or the performance of a function by the *Commissioner; or
(b) the operation of a provision of this Act or that other Act;
is dependent on the opinion, belief or state of mind of the Commissioner in relation to a matter:
(c) that power or function may be exercised or performed by an acting Commissioner, or by the *Deputy Commissioner when acting as Commissioner; and
(d) that provision may operate;
on the opinion, belief or state of mind in relation to that matter of the acting Commissioner, or of the Deputy Commissioner when so acting.
270‑25 Remuneration and allowances of members
(1) A *member is to be paid the remuneration that is determined by the Remuneration Tribunal. If no determination of that remuneration by the Tribunal is in operation, the member is to be paid the remuneration that is specified in the Private Health Insurance (Council) Rules.
(2) A *member is to be paid such allowances as are set out in the Private Health Insurance (Council) Rules.
(3) This section has effect subject to the Remuneration Tribunal Act 1973.
(1) A full‑time *Commissioner has such recreation leave entitlements as are determined by the Remuneration Tribunal.
(2) The Minister may grant a full‑time *Commissioner leave of absence, other than recreation leave, on such terms and conditions as to remuneration or otherwise as are specified in the Private Health Insurance (Council) Rules.
(3) The *Commissioner may grant another *member leave to be absent from a meeting or meetings of the Council.
A *member may resign by writing signed and given to the Minister.
270‑40 Termination of appointment
(1) The Minister may terminate the appointment of a *member for misbehaviour or physical or mental incapacity.
(2) The Minister must terminate the appointment of *a member if:
(a) the member becomes bankrupt, applies to take the benefit of a law for the relief of bankrupt or insolvent debtors, compounds with his or her creditors or makes an assignment of his or her remuneration for their benefit; or
(b) the member is absent, except with the leave of the *Commissioner, from 3 consecutive meetings of the Council; or
(c) the member is appointed as the Commissioner on a full‑time basis and engages, except with the Minister’s approval, in paid employment outside the duties of his or her office; or
(d) the member is appointed on a part‑time basis and engages in paid employment that, in the Minister’s opinion, conflicts with the proper performance of his or her duties; or
(e) the member fails, without reasonable excuse, to comply with section 270‑45.
270‑45 Disclosure of interests
(1) A *member who has a direct or indirect pecuniary interest in a matter being considered or about to be considered by the Council must disclose the nature of the interest to a meeting of the Council.
(2) The disclosure must be made as soon as possible after the relevant facts have come to the *member’s knowledge.
(3) The disclosure must be recorded in the minutes of the meeting of the Council.
(4) The *member:
(a) must not be present during any deliberation by the Council on the matter; and
(b) must not take part in any decision of the Council with respect to the matter.
Division 273—Chief Executive Officer and staff
(1) There is to be a *Chief Executive Officer of the Council who is to be appointed by the Council.
(2) The Council may:
(a) determine the terms and conditions of service of the *Chief Executive Officer in respect of matters not provided for by this Part; and
(b) at any time terminate such an appointment.
(3) The *Chief Executive Officer holds office on a full‑time basis.
(4) The *Chief Executive Officer holds office for the period, and subject to the terms and conditions, specified in the instrument of appointment.
(5) The appointment of a person as *Chief Executive Officer is not invalid because of a defect or irregularity in connection with the person’s appointment.
273‑5 Duties of Chief Executive Officer
(1) To the extent determined by the Council, the *Chief Executive Officer is to manage the affairs of the Council.
(2) The *Chief Executive Officer must, in managing the affairs of the Council, act in accordance with the policy of, and with any directions given by, the Council.
(1) The *Chief Executive Officer must not be present at a meeting of the Council when the Council is making a decision in relation to the office of Chief Executive Officer.
(2) If the *Chief Executive Officer has a direct or indirect pecuniary interest in a matter related to his or her duties as Chief Executive Officer, he or she must disclose the nature of the interest to the *Commissioner as soon as possible after the relevant facts have come to his or her knowledge.
(1) The Council may employ such staff as the Council thinks necessary to employ to assist the Council in the performance of its functions and the exercise of its powers.
(2) The *Commissioner may arrange with an Agency Head (within the meaning of the Public Service Act 1999) for the services of *officers or employees in the Agency to be made available to the Council.
(3) The Council may engage, under agreements in writing, persons having suitable qualifications and experience to perform services as consultants to the Council.
(4) The terms and conditions of staff employed, or consultants engaged, by the Council are such as are determined by the Council from time to time.
273‑20 Remuneration and allowances of Chief Executive Officer
(1) The *Chief Executive Officer is to be paid the remuneration that is determined by the Remuneration Tribunal. If no determination of that remuneration by the Tribunal is in operation, the Chief Executive Officer is to be paid the remuneration that is specified in the Private Health Insurance (Council) Rules.
(2) The *Chief Executive Officer is to be paid such allowances as are set out in the Private Health Insurance (Council) Rules.
(3) This section has effect subject to the Remuneration Tribunal Act 1973.
273‑25 Leave of absence of Chief Executive Officer
(1) The *Chief Executive Officer has such recreation leave entitlements as are determined by the Remuneration Tribunal.
(2) The Council may grant the *Chief Executive Officer leave of absence, other than recreation leave, on such terms and conditions as to remuneration or otherwise as are specified in the Private Health Insurance (Council) Rules.
Part 6‑4—Administration of premiums reduction and incentive payments schemes
Part 2‑2 provides for a premiums reduction scheme and an incentives payment scheme. This Part provides:
(a) for private health insurers to be reimbursed for premiums that were reduced under the premiums reduction scheme in Division 23; and
(b) for the Medicare Australia CEO to supervise that reimbursement and related matters; and
(c) for recovery of amounts paid in error; and
(d) for various other related administrative matters in relation to the schemes.
Division 279—Provisions applying only to premiums reduction scheme
Subdivision 279‑A—Reimbursement of private health insurers for premiums reduced under scheme
279‑1 Participating insurers may claim reimbursement
A private health insurer may claim reimbursement from the Medicare Australia CEO in accordance with section 279‑10 for each month during which it is a *participating insurer.
(1) A private health insurer may apply to the Minister, in the *approved form, to become a *participating insurer for the purposes of this Part.
(2) If the Minister approves the application, the private health insurer becomes a *participating insurer.
(3) The Minister must approve the application, unless:
(a) the insurer’s status as a *participating insurer has previously been revoked under subsection 206‑1(1); and
(b) the Minister is satisfied that the insurer is continuing, or will continue, to fail to comply with a provision or condition mentioned in that subsection.
Note: Rejections of applications are reviewable under Part 6‑9.
(4) The Minister must notify the applicant, within 28 days after the date of the decision, whether the application has been approved or rejected.
(5) If the application is rejected, the Minister must include his or her reasons for rejecting the application in the notice.
279‑10 Requirements for claims
(1) A claim by a private health insurer in respect of a month must be made to the Medicare Australia CEO, in the *approved form, on or before the seventh day of the following month.
(2) If the Medicare Australia CEO decides the claim is correct, the Medicare Australia CEO must pay the insurer, in accordance with section 279‑15, the amount payable under that section in respect of the month to which the claim relates.
279‑15 Amounts payable to the private health insurer
(1) Subject to subsection (2), the amount payable to the private health insurer in respect of the month is the sum of the amounts by which premiums in respect of that month under the *complying private health insurance policies issued by the private health insurer were reduced because of the operation of Division 23.
(2) The amount must be paid to the private health insurer within the period of 15 days starting on the first day of the following month.
(3) The amount must be paid in the way determined, in writing, by the Medicare Australia CEO.
279‑20 Notifying private health insurers if amount is not payable
(1) If the Medicare Australia CEO considers that a claim is incorrect, the Medicare Australia CEO may either refuse the claim or pay only such part of the claim as he or she is satisfied is correct.
(2) The Medicare Australia CEO must notify a private health insurer if the Medicare Australia CEO makes a decision mentioned in subsection (1).
(3) A notice under subsection (2) must include reasons for the decision.
(4) The Medicare Australia CEO is taken, for the purposes of this Part, to have decided that a claim is correct if the Medicare Australia CEO does not give notice of his or her decision that the claim is incorrect on or before the day under subsection 279‑15(2) on or before which, if the claim were correct, it would have been required to have been paid.
279‑25 Additional payment if insurer claims less than entitlement
(1) This section applies to a private health insurer in respect of a month if:
(a) the private health insurer is a *participating insurer in respect of the month; and
(b) the private health insurer made a claim in respect of the month under section 279‑1; and
(c) the amount claimed by the private health insurer was less than the sum of the amounts by which premiums in respect of the month under the *complying health insurance policies issued by the private health insurer were reduced because of the operation of this Division.
(2) The private health insurer may apply to the Medicare Australia CEO for payment of an amount (the additional amount) not exceeding the difference between:
(a) the sum of the amounts by which premiums in respect of the month under the *complying health insurance policies issued by the private health insurer were reduced because of the operation of this Division; and
(b) the amount already paid to the private health insurer under section 279‑1 in respect of the month.
(3) An application under subsection (2) may relate to more than one month.
279‑30 Additional payment if insurer makes a late claim
(1) This section applies to a private health insurer in respect of a month if:
(a) the private health insurer did not make a claim in respect of the month on or before the seventh day of the following month; and
(b) premiums in respect of the month under the *complying health insurance policies issued by the private health insurer were reduced because of the operation of this Division.
(2) The private health insurer may apply to the Medicare Australia CEO for payment of an amount (the additional amount) not exceeding the sum of the amounts by which premiums in respect of the month under the *complying health insurance policies issued by the private health insurer were reduced because of the operation of Division 23.
(3) An application under subsection (2) may relate to more than one month.
279‑35 Content and timing of application
(1) An application by a private health insurer under section 279‑25 or 279‑30 for payment of an additional amount must be in the *approved form.
(2) The application must be made:
(a) if the application relates to only one month—within 3 years of the end of that month; or
(b) if the application relates to more than one month—within 3 years of the end of the first of those months.
279‑40 Decision on application
(1) If a private health insurer makes an application under section 279‑25 or 279‑30 for payment of an additional amount, the Medicare Australia CEO must pay the additional amount sought if the Medicare Australia CEO is satisfied:
(a) that the additional amount sought is correct; and
(b) that it would be reasonable to grant the application.
(2) The Medicare Australia CEO may refuse the application, or decide to pay only part of the additional amount sought, if the Medicare Australia CEO is satisfied:
(a) that the additional amount sought is incorrect; or
(b) that it would not be reasonable to grant the application.
(3) The Medicare Australia CEO must notify the private health insurer of the Medicare Australia CEO’s decision on the application.
(4) A notice under subsection (3) must include reasons for the decision.
(5) The Medicare Australia CEO is taken, for the purposes of this Part, to have decided that:
(a) the additional amount sought is correct; and
(b) that it would be reasonable to grant the application;
if the Medicare Australia CEO does not give notice of his or her decision that the additional amount sought is incorrect, or that it would not be reasonable to grant the application, within the period of 3 months after the application was received by the Medicare Australia CEO.
(6) If the Medicare Australia CEO is taken to have made a decision under subsection (5) in respect of a private health insurer, the Medicare Australia CEO is taken to have given notice of that decision to the private health insurer.
279‑45 Reconsideration of decisions
(1) A private health insurer that has been given a notice under subsection 279‑20(2) or 279‑40(3) may request the Medicare Australia CEO to reconsider the decision.
(2) The request must:
(a) set out the reasons for the request; and
(b) be made within the period of 28 days after the day on which the Medicare Australia CEO gave the notice.
(3) As soon as practicable after receiving the request, the Medicare Australia CEO must reconsider the decision and:
(a) affirm it; or
(b) vary it; or
(c) revoke it and make a fresh decision.
Note: Decisions on reconsideration are reviewable under Part 6‑9.
(4) If the Medicare Australia CEO varies the decision or revokes the decision and makes a fresh decision, the decision as varied, or the fresh decision, as the case may be, has effect according to its terms and is taken always to have had that effect from the time when the original decision was made.
(5) The Medicare Australia CEO must notify the private health insurer stating the Medicare Australia CEO’s decision on the reconsideration together with a statement of his or her reasons for the decision.
(6) The Medicare Australia CEO is taken, for the purposes of this Part, to have revoked the decision if the Medicare Australia CEO does not notify the private health insurer of his or her decision on the reconsideration within 28 days after receiving the request.
Subdivision 279‑B—Powers of Medicare Australia CEO in relation to participating insurers
279‑50 Audits by Medicare Australia CEO
(1) The Medicare Australia CEO may, at any time, audit the accounts and records of a private health insurer that is, or has been, a *participating insurer.
(2) An audit under subsection (1) must relate only to the accounts and records of the private health insurer to the extent that they deal with:
(a) participation by persons in the *premiums reduction scheme; or
(b) reductions of premium payable under *complying private health insurance policies under the premiums reduction scheme; or
(c) receipt of money from the Medicare Australia CEO under this Division.
(3) The Medicare Australia CEO must not carry out an audit unless he or she has given notice to the private health insurer concerned stating that an audit is to be carried out.
(4) The private health insurer must ensure that the Medicare Australia CEO has full and free access to all accounts, records, documents and papers of the private health insurer that are relevant to the audit.
(5) The person carrying out the audit may make copies of, or take extracts from, such accounts, records, documents or papers for use in the audit.
(6) Without limiting the powers of the Medicare Australia CEO under this section, the Medicare Australia CEO may, by notice given to a private health insurer, require the insurer to give to the Medicare Australia CEO, within a period specified in the notice beginning at the end of a financial year, a certificate in writing by a registered company auditor as to the correctness of the accounts and records of the insurer for that year to the extent that those accounts and records deal with matters mentioned in paragraphs (2)(a), (b) and (c).
279‑55 Medicare Australia CEO may require production of applications
(1) The Medicare Australia CEO may, by notice given to a private health insurer, require the private health insurer:
(a) to produce to the Medicare Australia CEO, within the period and in the manner specified in the notice, applications retained under section 23‑45; or
(b) to make copies of any such applications and give them to the Medicare Australia CEO within the period and in the manner specified in the notice.
(2) A period specified under subsection (1) must not be less than one month.
(3) A private health insurer is entitled to be paid by the Medicare Australia CEO reasonable compensation for complying with paragraph (1)(b).
Division 282—Provisions applying to premiums reduction scheme and incentive payments scheme
Subdivision 282‑A—When and how payments can be recovered
(1) The following amounts are recoverable as debts due to the Commonwealth:
(a) a payment made to a person under Subdivision 26‑B to which the person was not entitled;
(b) a payment made to a person under Subdivision 26‑B in respect of a premium that was afterwards refunded;
(c) a payment made to a person under Subdivision 26‑B in respect of a claim that has been withdrawn under section 26‑15;
(d) so much of a payment made under section 279‑15 or 279‑40 as relates to a *complying health insurance policy that covers a person who was:
(i) a *participant in the premiums reduction scheme for the financial year concerned in respect of the policy; and
(ii) not eligible to participate in that scheme in respect of that policy;
(e) so much of a payment made under section 279‑15 or 279‑40 as relates to a premium for which a reduction was not allowable under section 23‑1;
(f) 150% of so much of a payment made under section 279‑15 or 279‑40 as:
(i) is not reflected in reductions in premiums payable under complying private health insurance policies issued by the private health insurer concerned; or
(ii) relates to a person whose application under subsection 23‑15(1) has not been retained by the private health insurer as required by section 23‑45; or
(iii) relates to a person whose application under subsection 23‑15(1) has been so retained, but has not been produced to the Medicare Australia CEO by the private health insurer in accordance with a requirement made by the Medicare Australia CEO under section 279‑55;
(g) so much of a payment purportedly made under section 279‑15 or 279‑40 as was not payable under that section;
(h) interest payable under subsection 282‑5(2).
(2) The amounts are recoverable from:
(a) if paragraph (1)(a), (b) or (c) applies—the person referred to in that paragraph or that person’s estate; or
(b) if paragraph (1)(d), (e), (f) or (g) applies—the private health insurer to which the payment concerned was made; or
(c) if paragraph (1)(h) applies:
(i) if the payment was made to a private health insurer—that insurer; or
(ii) if the payment was made to an individual—the individual or his or her estate.
(3) An amount recoverable under subsection (1) is recoverable whether or not any person has been convicted of an offence relating to the payment.
282‑5 Interest on amounts recoverable
(1) If the Medicare Australia CEO has served, on an individual from whom an amount is recoverable or the legal personal representative of such an individual, or on a private health insurer from which an amount is recoverable, under subsection 282‑1(1) a notice claiming an amount as a debt due to the Commonwealth and:
(a) an arrangement for the repayment of the amount has been entered into between the Medicare Australia CEO and the individual or the individual’s legal personal representative, or the private health insurer, as the case may be, within the period referred to in subsection (3), and there has been a default in payment of an amount required to be paid under the arrangement; or
(b) at the end of the period such an arrangement has not been entered into and all or part of the amount remains unpaid;
then, from and including the day after the end of the period, interest becomes payable on so much of the amount as from time to time remains unpaid.
(2) Interest is payable:
(a) at the rate of 15% per annum; or
(b) if a lower rate is specified in the Private Health Insurance (Incentives) Rules for the purposes of this paragraph—that rate.
(3) The period for entering into an arrangement under paragraph (1)(a) is the period of 3 months following the service of the notice under subsection (1), or such longer period as the Medicare Australia CEO allows.
(4) Despite subsection (1), in any proceedings instituted by the Commonwealth for the recovery of an amount due under paragraph 282‑1(1)(h), the court may order that the interest payable under that paragraph is, and is taken to have been, so payable from and including a day later than the day referred to in subsection (1).
282‑10 Medicare Australia CEO may set off debts against amounts payable
(1) Despite any other provision of Part 2‑2 or this Part, if:
(a) except for this section, an amount would be payable by the Medicare Australia CEO to a person or his or her estate, or to a private health insurer, under Part 2‑2 or this Part; and
(b) an amount is recoverable under section 282‑1 by the Commonwealth from the person or his or her estate, or from the insurer, as the case may be;
the Medicare Australia CEO may set off the whole or a part of the amount referred to in paragraph (b) against the amount referred to in paragraph (a).
(2) If the Medicare Australia CEO decides to make such a set‑off in respect of a person or his or her estate, the Medicare Australia CEO must serve on the person or his or her legal personal representative or the legal personal representative of his or her estate a notice of the decision.
(3) If the Medicare Australia CEO makes such a set‑off:
(a) the Medicare Australia CEO is liable to pay to the person or his or her estate, or to the insurer, only the amount remaining after the set‑off; and
(b) the amount referred to in paragraph (1)(b) is reduced by the amount set off.
282‑15 Reconsideration of certain decisions under this Division
(1) A person (the applicant) may apply to the Medicare Australia CEO for the Medicare Australia CEO to reconsider the following decisions:
(a) a decision that an amount is recoverable as a debt due to the Commonwealth under:
(i) paragraph 282‑1(1)(a) or (b); or
(ii) paragraph 282‑1(1)(h) in respect of a payment made to an individual; or
(b) a decision under subsection 282‑10(1) to set off a debt against an amount otherwise payable to a person (other than a private health insurer) or his or her estate.
(2) The application must:
(a) be in writing; and
(b) set out the reasons for the application.
(3) The application must be made within:
(a) 28 days after the day on which the applicant is notified of the decision; or
(b) if, either before or after the end of that period of 28 days, the Medicare Australia CEO extends the period within which the application may be made—the extended period for making the application.
(4) Upon receiving such an application, the Medicare Australia CEO must:
(a) reconsider the decision; and
(b) either affirm or revoke the decision.
Note: Decisions affirming an original decision of the Medicare Australia CEO are reviewable under Part 6‑9.
(5) If the Medicare Australia CEO revokes the decision, the revocation is taken to be a decision:
(a) in the case of a decision mentioned in paragraph (1)(a)—to waive the debt; or
(b) in the case of a decision mentioned in paragraph (1)(b)—not to set off a debt against an otherwise payable amount.
(6) The Medicare Australia CEO must give the applicant a notice stating his or her decision on the reconsideration together with a statement of his or her reasons for the decision.
(7) The Medicare Australia CEO must make his or her decision on the reconsideration within 28 days after the day on which he or she received the application for the reconsideration.
(8) The Medicare Australia CEO is taken, for the purposes of this Subdivision, to have made a decision confirming the original decision if the Medicare Australia CEO has not told the applicant of his or her decision on the reconsideration before the end of the period of 28 days.
Subdivision 282‑B—Miscellaneous
282‑20 Notification requirements—private health insurers
(1) The Medicare Australia CEO may, by notice given to a private health insurer, require the insurer, within the period specified in the notice, to provide information specified in the notice about a person who:
(a) is covered at any time during a financial year specified in the notice by a *complying health insurance policy issued by the insurer; or
(b) paid premiums under such a policy.
(2) The information must be given in the *approved form.
(3) A private health insurer commits an offence if:
(a) the insurer is required by a notice under subsection (1) to provide information within a specified period about a person or matter; and
(b) the insurer fails to comply with the requirement.
Penalty: 20 penalty units.
Note: The obligation to provide information in response to a notice under subsection (1) is a continuing obligation and a private health insurer commits an offence for each day, after the period specified in the notice, until the information is provided (see section 4K of the Crimes Act 1914).
(4) Strict liability applies to subsection (3).
Note: For strict liability, see section 6.1 of the Criminal Code.
282‑25 Use etc. of information relating to another person
A person commits an offence if:
(a) the person uses, makes a record of, or discloses or communicates to any person, any information that relates to the affairs of another person and was acquired under or for the purposes of Part 2‑2 or this Part; and
(b) the use, making of the record, disclosure or communication was not carried out in the performance of a function or obligation, or the exercise of a power, under Part 2‑2 or this Part.
Penalty: Imprisonment for 1 year.
282‑30 Information to be provided to the Commissioner of Taxation
(1) The Medicare Australia CEO must, within 120 days after the end of each financial year, give to the Commissioner of Taxation the information that the Commissioner of Taxation, by legislative instrument, determines.
(2) A determination under subsection (1) must not require the Medicare Australia CEO to give:
(a) the *tax file number of any person; or
(b) information about the physical, psychological or emotional health of any person.
The Medicare Australia CEO may, by writing, delegate all or any of his or her powers under Part 2‑2 or this Part to an employee of Medicare Australia.
Note: The Minister may also delegate his or her powers under Part 2‑2 or this Part (see section 333‑5).
The Consolidated Revenue Fund is appropriated for the purpose of making payments under Part 2‑2 and this Part.
Part 6‑5—External managers and terminating managers
External management of health benefits funds takes place under Division 217, and terminating management of health benefits funds takes place under Division 149. This Part provides for several matters relating to external management and terminating management under those Divisions.
287‑5 The Private Health Insurance (Management) Rules
*External management and *terminating management of *health benefits funds is also dealt with in the Private Health Insurance (Management) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Management) Rules are made by the Minister under section 333‑20.
Division 290—Powers of managers
(1) While a *health benefits fund is under *external management or *terminating management, the *manager has power, in the interests of the *policy holders of the fund:
(a) to control the business, affairs and property of the fund; and
(b) to carry on the business of the fund, and to manage the affairs and property of the fund; and
(c) to terminate or dispose of all or any part of the business, and to dispose of all or any part of the property, of the fund; and
(d) to execute a document, bring or defend proceedings, or do any other thing, in the name of the*responsible insurer for the fund, for the purposes of the business of the fund; and
(e) to appoint a solicitor to assist him or her in his or her duties; and
(f) to appoint an agent to do any business that the manager is unable to do, or that it is unreasonable to expect the manager to do, in person; and
(g) to perform any other function and exercise any other power that the insurer or any of its *officers could perform or exercise in relation to the conduct of the fund if the fund were not under external management or terminating management.
(2) The rights of the insurer, and any of its *officers, to exercise any of those powers in relation to the fund is suspended while the fund is under *external management or *terminating management.
290‑5 Officers etc. not to perform functions etc. while fund is under management
(1) A person commits an offence if:
(a) a *health benefits fund is under *external management or *terminating management; and
(b) the person performs or exercises in relation to the fund, or purports to perform or exercise in relation to the fund, a function or power of:
(i) an *officer of the *responsible insurer for the fund; or
(ii) a receiver, or receiver and manager, of any of the *assets of the fund; and
(c) the person is not the *manager of the fund; and
(d) it is a function or power of the manager; and
(e) the person does so without the manager’s written approval.
Penalty: 30 penalty units or imprisonment for 6 months, or both.
(2) Subsection (1) does not imply that an *officer of the insurer is removed from his or her office.
(3) Section 149‑30 or 217‑20 does not limit the scope of subsection (1).
(4) To avoid doubt, a person is not an *officer of a private health insurer merely because he or she is an employee of the insurer.
290‑10 Managers act as agents of private health insurers
(1) When exercising a power as *manager of a *health benefits fund, the manager is taken to be acting as the agent of the *responsible insurer for the fund.
(2) To avoid doubt, subsection (1) does not confer on the *responsible insurer for the fund power to direct the *manager in the exercise of his or her powers.
Division 293—Information concerning, and records and property of, health benefits funds
293‑1 Directors etc. to help managers
(1) As soon as practicable after the *external management or *terminating management of a *health benefits fund begins, each *director of the *responsible insurer for the fund must:
(a) deliver to the *manager all records in the director’s possession that relate to the business of the fund, other than records that the director is entitled to retain as against the manager and the insurer; and
(b) if the director knows of the locality of other records relating to the business of the fund—tell the manager of that locality.
(2) Within 7 days after the *external management or *terminating management of the fund begins, or such longer period as the *manager allows, the *directors and other *officers of the *responsible insurer for the fund must give to the manager a statement about the business, property, affairs and financial circumstances of the fund.
(3) The statement must comply with any requirements of the *manager as to its form and contents.
(4) A *director or other *officer of the *responsible insurer for the fund must:
(a) attend on the *manager at such times; and
(b) give the manager such information about the business, property, affairs and financial circumstances of the fund;
as the manager reasonably requires.
(5) A person who fails to comply with the requirements of subsection (1), (2), (3) or (4) commits an offence.
Penalty: 30 penalty units or imprisonment for 6 months, or both.
293‑5 Managers’ rights to certain records
(1) A person is not entitled, as against the *manager of a *health benefits fund:
(a) to retain possession of records of the *responsible insurer for the fund; or
(b) to claim or enforce a lien on such records;
but such a lien is not otherwise prejudiced.
(2) Paragraph (1)(a) does not apply in relation to records of which a secured creditor of the *responsible insurer for the fund is entitled to possession otherwise than because of a lien. However, the *manager is entitled to inspect, and make copies of, such records at any reasonable time.
(3) The *manager of a *health benefits fund may give to a person written notice requiring the person to deliver to the manager, as specified in the notice, records so specified that are in the person’s possession.
(4) A notice under subsection (3) must specify a period of at least 3 days as the period within which the notice must be complied with.
(5) A person commits an offence if:
(a) the person receives a notice under subsection (3) from the *manager of a *health benefits fund; and
(b) the person does not comply with the notice.
Penalty: 30 penalty units or imprisonment for 6 months, or both.
(6) Subsection (5) does not apply if the person is entitled to retain possession of the records, as against the *manager and also as against the *responsible insurer for the fund.
Note: The defendant bears an evidential burden in relation to the matter in subsection (6). See subsection 13.3(3) of the Criminal Code.
293‑10 Only manager can deal with property of fund under management
(1) A transaction or dealing affecting the property of a *health benefits fund under *external management or *terminating management, that is entered into by the *responsible insurer for the fund or by a person purportedly on behalf of the fund or the responsible insurer, is void unless:
(a) the transaction or dealing has been entered into by the *manager of the fund; or
(b) the manager consented to the transaction or dealing before it was entered into; or
(c) the transaction or dealing was entered into by order of the Federal Court or of the Supreme Court of a State or Territory.
(2) Subsection (1) does not apply to a payment that an *ADI makes, out of an account kept with the ADI by the *responsible insurer for the fund, that is made:
(a) in good faith and in the ordinary course of the ADI’s banking business; and
(b) after the *external management or *terminating management began but on or before the day on which:
(i) the *manager gives to the ADI written notice of the appointment that began the external management or terminating management; or
(ii) the manager notifies the appointment in a national newspaper, or in a newspaper circulating in each jurisdiction where the responsible insurer has its registered office or carries on business;
whichever happens first.
(3) Subsection (1) has effect subject to any order that the Federal Court makes after the purported transaction or dealing.
(4) A person commits an offence if:
(a) the person is:
(i) an *officer of the *responsible insurer for a *health benefits fund under *external management or *terminating management; or
(ii) a receiver, or receiver and manager, of any of the *assets of the fund; and
(b) the person:
(i) purported to enter into a transaction or dealing on behalf of the responsible insurer; or
(ii) was in any way, by act or omission, directly or indirectly concerned in, or party to, a transaction or dealing; and
(c) the transaction or dealing is, because of the operation of subsection (1), void, or would be void apart from subsection (3).
Penalty: 30 penalty units or imprisonment for 6 months, or both.
293‑15 Order for compensation where officer involved in void transaction
(1) If:
(a) a court finds a person guilty of an offence against subsection 293‑10(4) (including such an offence that is taken to have been committed because of section 5 of the Crimes Act 1914); and
(b) the court is satisfied that the *health benefits fund under *external management or *terminating management to which the offence relates has suffered loss or damage because of the act or omission constituting the offence;
the court may (whether or not it imposes a penalty) order the person to pay compensation of such amount as the order specifies to the *responsible insurer for the fund.
(2) An order under subsection (1) may be enforced as if it were a judgment of the court.
(3) If, in proceedings against a person under subsection 293‑10(4), it appears to the court that the person is, or might be, liable to pay compensation under subsection (1), but that:
(a) the person has acted honestly; and
(b) having regard to all the circumstances of the case, the person ought fairly to be excused from paying compensation;
the court may relieve the person either wholly or partly from a liability to pay compensation under subsection (1) to which the person would otherwise be subject, or that might otherwise be imposed on the person.
(4) If a person thinks that proceedings under subsection 293‑10(4) will, or might be, begun against him or her, he or she may apply to the Federal Court for relief.
(5) On an application under subsection (4), the Federal Court may grant relief under subsection (3) as if proceedings under subsection 293‑10(4) had been begun in the Federal Court.
(6) For the purposes of subsection (3) as it applies for the purposes of a case tried by a judge with a jury:
(a) a reference in that subsection to the court is a reference to the judge; and
(b) the relief that may be granted includes withdrawing the case in whole or in part from the jury and directing judgment to be entered for the defendant on such terms as to costs as the judge thinks appropriate.
Division 296—Provisions incidental to appointment of managers
296‑1 Remuneration of managers
(1) The Council may, in writing, determine:
(a) the remuneration and allowances that an *external manager or *terminating manager is to receive; and
(b) who is to pay that remuneration and those allowances, if they are not to be paid as mentioned in subsection (2).
(2) Unless the Council determines otherwise, the remuneration and allowances are to be paid out of the *assets of the *health benefits fund under *external management or *terminating management.
296‑5 Council may give directions to managers
(1) The Council may give a *manager written directions concerning the exercise of the powers that are vested in the manager.
(2) The directions given to the *manager will ordinarily be of a general nature but may, where appropriate, take into account specific circumstances relevant to the particular *health benefits fund under *external management or *terminating management.
(3) The Council may also give directions to the *manager concerning the provision to the Council, from time to time, of interim reports relating to the business of the *health benefits fund under *external management or *terminating management.
(4) The *manager must comply with any directions given to him or her under this section.
296‑10 Termination of appointments of managers
(1) The Council may, at any time, by written notice given to a *manager, terminate the appointment of the manager with effect from the date specified in the instrument of termination.
(2) If the Council terminates the appointment of an *external manager, it may appoint another external manager (the replacement external manager) to carry on the *external management.
(3) If the Council terminates the appointment of an *external manager of a *health benefits fund but does not appoint a replacement external manager, then, with effect from the termination:
(a) the external manager whose appointment has been terminated is divested of the power:
(i) to control the business, affairs and property of the fund; and
(ii) to carry on the business, and to manage the affairs and property, of the fund;
and those powers vest once again in the *officers of the *responsible insurer for the fund; and
(b) all of the other powers of the external manager in relation to the fund cease.
(4) If the Council terminates the appointment of a *terminating manager, it must appoint another terminating manager to carry on the *terminating management, unless:
(a) the Federal Court has ordered under section 149‑35 an end to the termination of the *health benefits funds in question; or
(b) the termination of those funds has been *completed, and the terminating manager has reported to the Council under section 149‑55.
296‑15 Acts of managers valid etc.
(1) The acts of the *manager of a *health benefits fund are valid despite any defects that may afterwards be discovered in his or her appointment.
(2) Despite any defect or irregularity affecting the validity of the appointment of *manager of a *health benefits fund:
(a) a conveyance, assignment, transfer, mortgage or charge of *assets of the fund; or
(b) a payment of money of the fund; or
(c) any other disposition of assets of the fund;
is valid in favour of any person taking such assets in good faith and for value and without actual knowledge of the defect or irregularity.
(3) Despite any defect or irregularity affecting the validity of the appointment of *manager of a *health benefits fund, a person making or permitting:
(a) a payment of money of the fund; or
(b) any other disposition of *assets of the fund;
is to be protected and indemnified in so doing despite any defect or irregularity affecting the validity of the appointment of the manager that is not then known to that person.
The *manager of a *health benefits fund is not subject to any action, claim or demand by, or liable to, any person in respect of anything done or omitted to be done in good faith in, or in connection with, the exercise of the powers conferred on the manager by this Act.
The *manager of a *health benefits fund has qualified privilege in respect of a statement that he or she makes, whether orally or in writing, in the course of his or her duties as manager.
299‑1 Time for doing act does not run while act prevented by this Division
If:
(a) for any purpose (for example, the purposes of a law, agreement or instrument) an act must or may be done within a particular period or before a particular time; and
(b) Division 149 or Part 5‑3 or this Part prevents the act from being done within that period or before that time;
the period is extended, or the time is deferred, because of this section, according to how long Division 149 or Part 5‑3 or this Part prevented the act from being done.
299‑5 Continued application of other provisions of Act
(1) The appointment of a person as the *external manager of a *health benefits fund does not affect the continued operation of provisions of this Act other than the provisions of Division 217:
(a) in relation to the fund; or
(b) in relation to the rights and obligations of persons in relation to the *responsible insurer for the fund.
(2) The appointment of a person as the *terminating manager of a *health benefits fund does not affect the continued operation of provisions of this Act other than the provisions of Division 149 or 220:
(a) in relation to the fund; or
(b) in relation to the rights and obligations of persons in relation to the *responsible insurer for the fund.
299‑10 Modifications of this Act in relation to health benefits funds under management
(1) The Private Health Insurance (Management) Rules may set out modifications of this Act (including omissions, additions and substitutions) relating to how Chapter 3 applies in relation to *health benefits funds for which:
(a) *external managers have been appointed under Division 217; or
(b) *terminating managers have been appointed under Division 149 or 220.
(2) The Private Health Insurance (Management) Rules may provide for different such modifications according to the nature of the *health benefits funds concerned.
(3) The modifications cannot:
(a) modify a provision of this Act that creates an offence; or
(b) include new provisions that create offences.
(4) This Act has effect subject to the modifications.
299‑15 Order of Court to be binding on all persons
An order of the Court made under Division 149, Part 5‑3 or this Part, relating to any matter, is binding on all persons and has effect despite anything in the constitution or *rules of a private health insurer to which the order may relate.
299‑20 Jurisdiction of Federal Court
The Federal Court has jurisdiction to hear and determine applications under Division 149, Part 5‑3 or this Part and to make any necessary orders in respect of those applications.
299‑25 Private Health Insurance (Management) Rules dealing with various matters
The Private Health Insurance (Management) Rules may:
(a) make provision for, or in relation to, any of the following matters in relation to meetings required or permitted to be held by Division 217, or by provisions of the Private Health Insurance (Health Benefits Fund Enforcement) Rules made for the purposes of that Division:
(i) the convening, conduct of, and procedure at, a meeting;
(ii) voting at a meeting (including proxy voting);
(iii) the number of persons that constitutes a quorum at a meeting;
(iv) the sending of notices to persons entitled to attend a meeting;
(v) the lodging of copies of notices of, or resolutions passed at, a meeting; and
(b) make provision relating to the form and contents of any document or instrument required or permitted to be given to the Council, or to an *external manager or *terminating manager of a *health benefits fund, by a provision of Division 217 or 149.
Part 6‑6—Private health insurance levies
Each private health insurance levy is imposed under a levy Act. This Part deals with collection of the levies and other matters relating to their administration.
304‑5 Private Health Insurance (Levy Administration) Rules
The collection of *private health insurance levies and other matters relating to administration of the levies are also dealt with in the Private Health Insurance (Levy Administration) Rules. The provisions of this Part indicate when a particular matter is or may be dealt with in these Rules.
Note: The Private Health Insurance (Levy Administration) Rules are made by the Minister under section 333‑20.
304‑10 Meaning of private health insurance levy
Each of the following levies is a private health insurance levy:
(a) levy imposed under the Private Health Insurance (Collapsed Insurer Levy) Act 2003 (collapsed insurer levy);
(b) levy imposed under the Private Health Insurance (Complaints Levy) Act 1995 (complaints levy);
(c) levy imposed under the Private Health Insurance (Council Administration Levy) Act 2003 (Council administration levy);
(d) levy imposed under the Private Health Insurance (Risk Equalisation Levy) Act 2003 (risk equalisation levy).
Division 307—Collection and recovery of private health insurance levies
307‑1 When private health insurance levy must be paid
(1) A *private health insurance levy that is imposed on a particular day (the imposition day) becomes due and payable on the day specified as the payment day for that imposition day in:
(a) a determination made by the Minister, by legislative instrument, if the levy is:
(i) *collapsed insurer levy; or
(ii) *Council administration levy imposed on a supplementary Council administration levy day (within the meaning of the Private Health Insurance (Council Administration Levy) Act 2003; or
(iii) *complaints levy imposed on a supplementary complaints levy administration day (within the meaning of the Private Health Insurance (Complaints Levy) Act 1995; or
(iv) *risk equalisation levy imposed on a supplementary risk equalisation levy day (within the meaning of the Private Health Insurance (Risk Equalisation Levy) Act 2003; and
(b) otherwise—the Private Health Insurance (Levy Administration) Rules.
(2) The Minister must obtain, and take into account, advice from the Council in relation to the day that is to be specified as the payment day in a determination made under subparagraph (1)(a)(i), (ii) or (iv).
(3) Advice given to the Minister under subsection (2) in relation to a determination under subparagraph (1)(a)(i) must be laid before each House of the Parliament with the determination to which it relates.
(1) If a *private health insurance levy remains wholly or partly unpaid by a private health insurer after it becomes due and payable, the insurer is liable to pay a late payment penalty under this section.
(2) The *late payment penalty is calculated:
(a) at the rate specified in the Private Health Insurance (Levy Administration) Rules (which must not be higher than 15%); and
(b) on the unpaid amount of the levy; and
(c) for the period:
(i) starting when the levy becomes due and payable; and
(ii) ending when the levy, and the penalty payable under this section, have been paid in full.
307‑10 Payment of levy and late payment penalty
(1) The following must be paid to the Commonwealth:
(a) a *complaints levy;
(b) a *late payment penalty in respect of a complaints levy.
(2) An amount of a kind specified in column 2 of the table must be paid to the Council. The amount is paid to the Council for the purpose specified in column 3 of the table:
Amounts payable to Council for certain purposes | ||
Item | An amount of this kind ... | is payable to the Council for the purpose of … |
1 | *collapsed insurer levy that is due and payable | helping a private health insurer that is unable to meet its liabilities to its contributors to meet those liabilities. |
2 | *late payment penalty in respect of *collapsed insurer levy | helping a private health insurer that is unable to meet its liabilities to its contributors to meet those liabilities. |
3 | *Council administration levy that is due and payable | meeting the general administrative costs of the Council. |
4 | *late payment penalty in respect of *Council administration levy | meeting the general administrative costs of the Council. |
5 | *risk equalisation levy that is due and payable | the *Risk Equalisation Trust Fund |
6 | *late payment penalty in respect of *risk equalisation levy | the *Risk Equalisation Trust Fund |
(3) The Consolidated Revenue Fund is appropriated for the purposes of subsection (2).
307‑15 Recovery of levy and late payment penalty
(1) A *private health insurance levy that is due and payable is a debt due to the Commonwealth.
(2) A *late payment penalty is a debt due to the Commonwealth.
(3) An amount referred to in subsection (1) or (2) may be recovered as a debt by action in a court of competent jurisdiction by:
(a) the Commonwealth, in respect of a debt payable to the Commonwealth under subsection 307‑10(1); or
(b) the Council, in respect of a debt payable to the Council under subsection 307‑10(2).
307‑20 Waiver of late payment penalty for levies other than collapsed insurer levy
(1) The Minister may waive the whole or part of an amount of *late payment penalty in respect of an unpaid amount of *complaints levy, if the Minister considers that there are good reasons for doing so.
(2) The Council may waive the whole or part of an amount of *late payment penalty in respect of an unpaid amount of:
(a) a *Council administration levy; or
(b) a *risk equalisation levy;
if the Council considers that there are good reasons for doing so.
307‑25 Waiver of collapsed insurer levy and late payment penalty for that levy
(1) If an amount of *collapsed insurer levy or *late payment penalty in respect of an amount of collapsed insurer levy (a collapsed insurer levy amount) is payable by a private health insurer, the insurer may apply for a waiver under this section.
(2) The application must be in writing and in the *approved form.
(3) The Minister may waive the whole or a part of the collapsed insurer levy amount if satisfied that the payment of the amount by the insurer would have a significantly adverse effect on the insurer’s ability to comply with:
(a) the *solvency standard or a *solvency direction; or
(b) the *capital adequacy standard or a *capital adequacy direction.
Note: Decisions under subsection (3) are reviewable under Part 6‑9.
(4) Before making a decision under subsection (3), the Minister must obtain, and take into account, advice from the Council as to whether to waive the collapsed insurer levy amount.
(5) The Minister must notify the insurer of the Minister’s decision under subsection (3).
(6) The notification must be:
(a) in writing; and
(b) given to the insurer within 28 days after the day on which the decision under subsection (3) is made.
The Private Health Insurance (Levy Administration) Rules may, in relation to *private health insurance levy or *late payment penalty, provide for, or for matters relating to, any or all of the following:
(a) methods for payment;
(b) extending the time for payment;
(c) refunding or otherwise applying overpayments.
Division 310—Returns, requesting information and keeping records
310‑1 Returns must be lodged with Council and Department
(1) A private health insurer must lodge a return for each *census day for the following levies:
(a) *collapsed insurer levy;
(b) *complaints levy;
(c) *Council administration levy.
(2) A census day for a levy means the day specified as the census day for that levy under the Act imposing the levy.
(3) The return must:
(a) be in the *approved form; and
(b) be lodged with:
(i) if the return relates to *complaints levy—the Secretary of the Department; and
(ii) otherwise—the Council; and
(c) be lodged within 28 days after the *census day for the levy to which it relates.
(4) A private health insurer commits an offence if the insurer fails to lodge the return.
Penalty: 60 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
310‑5 Insurer must keep records
(1) A private health insurer must keep all records that are relevant to either or both of following:
(a) whether the insurer is liable to pay a *private health insurance levy;
(b) the amount of the private health insurance levy that the insurer is liable to pay.
(2) The records must be kept in:
(a) an electronic form; or
(b) if the Council approves another form—that form.
(3) The records must be retained for a period of 7 years (or a shorter period allowed by the Private Health Insurance (Levy Administration) Rules) starting on the later of:
(a) the day on which the records were created; or
(b) 1 July 2004.
(4) A private health insurer commits an offence if the insurer fails to:
(a) keep the records; or
(b) keep the records in the form required by or under subsection (2); or
(c) retain the records for the period required by or under subsection (3).
Penalty: 60 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
(6) Nothing in this section is to be taken to have required an insurer to do an act or thing before the day on which this Act commences.
310‑10 Council may request information from insurer
(1) The Council may, if it believes on reasonable grounds that a private health insurer is capable of giving information that is relevant to:
(a) whether the insurer is liable to pay a *private health insurance levy (other than *complaints levy); or
(b) the amount of the private health insurance levy (other than complaints levy) that the insurer is liable to pay;
request the insurer to give the Council the information or records that are specified in the request, before the end of the period specified in the request.
(2) The Secretary of the Department may, if he or she believes on reasonable grounds that a private health insurer is capable of giving information that is relevant to:
(a) whether the insurer is liable to pay *complaints levy; or
(b) the amount of complaints levy that the insurer is liable to pay;
request the insurer to give him or her the information or records that are specified in the request, before the end of the period specified in the request.
(3) A request under subsection (1) or (2):
(a) must be served on the *chief executive officer of the insurer; and
(b) may require the information to be verified by statutory declaration; and
(c) must specify the manner in which the information must be given; and
(d) must contain a statement to the effect that a failure to comply with the request is an offence.
(4) A private health insurer commits an offence if the insurer fails to comply with a request under subsection (1) or (2).
Penalty: 60 penalty units.
(5) Strict liability applies to subsection (4).
Note: For strict liability, see section 6.1 of the Criminal Code.
Division 313—Power to enter premises and search for documents
313‑1 Authorised officer may enter premises with consent
(1) A person who is a member of staff of the Council or authorised in writing by the Minister for this purpose (both of these kinds of persons are authorised officers) may enter any *premises for the purpose of exercising *search powers in relation to *levy‑related documents if:
(c) the *occupier of the premises consents to the entry; and
(d) the officer shows the occupier his or her identity card.
(2) A levy‑related document is a document (including a copy of a document) that contains information relevant to:
(a) whether a private health insurer is liable to pay a *private health insurance levy; or
(b) the amount of the private health insurance levy that the insurer is liable to pay.
(3) Before obtaining the consent of the *occupier, the *authorised officer must inform the occupier that he or she may refuse consent.
(4) An entry by an *authorised officer with the consent of the *occupier is not lawful if the consent of the occupier is not voluntary.
(5) The *authorised officer must leave the *premises if the *occupier asks the officer to do so.
313‑5 Authorised officer may enter premises under warrant
(1) If an *authorised officer has reason to believe that there are *levy‑related documents on particular *premises, the officer may apply to a magistrate for a warrant authorising the officer to enter the premises for the purpose of exercising *search powers in relation to the documents.
(2) If the magistrate is satisfied by information on oath or affirmation that there are reasonable grounds for believing that there are *levy‑related documents on the *premises, the magistrate may issue a warrant.
(3) The warrant must:
(a) authorise one or more *authorised officers to enter the *premises for the purpose of exercising *search powers in relation to *levy‑related documents; and
(b) state whether the entry is authorised at any time of the day or night or during specified hours of the day or night; and
(c) authorise the officers to use such assistance and force as is necessary and reasonable to enter the premises for the purpose of exercising search powers in relation to levy‑related documents.
(4) The *authorised officers do not have to be named in the warrant.
313‑10 Announcement before entry
An *authorised officer executing a warrant under section 313‑5 in respect of *premises must, before entering the premises under the warrant:
(a) announce that he or she is authorised to enter the premises; and
(b) before using assistance and force under the warrant to enter the premises—give any person on the premises an opportunity to allow the authorised officer to enter the premises without the use of assistance and force.
313‑15 Executing a warrant to enter premises
Circumstances in which this section applies
(1) This section applies if:
(a) a warrant under section 313‑5 is being executed by an *authorised officer in respect of *premises; and
(b) the *occupier of the premises is present.
Obligations of authorised officer executing a warrant
(2) The *authorised officer must:
(a) make a copy of the warrant available to the *occupier; and
(b) show the occupier the officer’s identity card; and
(c) inform the occupier of the occupier’s rights and responsibilities under subsections (3) to (6).
Persons entitled to observe execution of warrant
(3) The *occupier, or a person nominated by the occupier who is readily available, is entitled to observe the execution of the warrant.
(4) The right to observe the execution of the warrant ceases if the *occupier or the nominated person impedes that execution.
(5) Subsection (3) does not prevent the execution of the warrant in 2 or more areas of the *premises at the same time.
Occupier to provide reasonable facilities and assistance
(6) An *occupier commits an offence if the occupier fails to provide the *authorised officer and any person assisting that officer with all reasonable facilities and assistance for the effective exercise of their powers under the warrant.
Penalty: 60 penalty units.
(1) For the purposes of this Division, the Council must issue an identity card to an *authorised officer in the *approved form. It must contain a recent photograph of the authorised officer.
(2) A person commits an offence if:
(a) the person has been issued with an identity card; and
(b) the person ceases to be an *authorised officer; and
(c) the person does not, as soon as it is practicable after so ceasing, return the identity card to the Council.
Penalty: 1 penalty unit.
(3) Strict liability applies to subsection (2).
Note: For strict liability, see section 6.1 of the Criminal Code.
(4) An *authorised officer must carry the identity card at all times when exercising powers or performing functions under this Division as an authorised officer.
Part 6‑7—Private Health Insurance Risk Equalisation Trust Fund
Division 318—Private Health Insurance Risk Equalisation Trust Fund
318‑1 Private Health Insurance Risk Equalisation Trust Fund
The Health Benefits Reinsurance Trust Fund established under section 73BC of the National Health Act 1953 is continued in existence as the Private Health Insurance Risk Equalisation Trust Fund (the Risk Equalisation Trust Fund).
318‑5 Amounts to be paid into the Risk Equalisation Trust Fund
(1) The following amounts are to be paid into the *Risk Equalisation Trust Fund:
(a) amounts appropriated by the Parliament for the purposes of the Fund;
(b) amounts received from the States or Territories for payment to the Fund;
(c) amounts of *risk equalisation levy received from private health insurers;
(d) amounts of *late payment penalty received from private health insurers in respect of unpaid amounts of risk equalisation levy;
(e) amounts received by the Council under paragraph 149‑45(b) or because of section 149‑50;
(f) the proceeds from any investments made using Fund money.
(2) The Consolidated Revenue Fund is appropriated for the purposes of paragraphs (1)(b), (c), (d) and (e) to the extent that section 81 of the Constitution applies to the amounts mentioned in those paragraphs.
318‑10 Operation of the Risk Equalisation Trust Fund
(1) The Private Health Insurance (Risk Equalisation Policy) Rules may set out requirements relating to how the *Risk Equalisation Trust Fund is to operate.
(2) Without limiting the matters that may be dealt with in those Rules, the Rules must specify:
(a) the method for working out the amount to be paid out of the Fund to a private health insurer; and
(b) the method for working out the amount to be paid into the Fund by private health insurers as *risk equalisation levy.
(3) If the Minister changes the Private Health Insurance (Risk Equalisation Policy) Rules, the Minister must notify the Council that the Minister has done so, as soon as practicable.
318‑15 Administration of the Risk Equalisation Trust Fund
The Private Health Insurance (Risk Equalisation Administration) Rules may set out requirements relating to the administration of the *Risk Equalisation Trust Fund and the *risk equalisation levy, including:
(a) the kinds of records to be kept by insurers who are required to pay risk equalisation levy; and
(b) the form in which those records are to be kept.
Part 6‑8—Disclosure of information
Division 323—Disclosure of information
323‑1 Prohibition on disclosure of information
(1) A person commits an offence if:
(a) the person has, or has at any time had, a duty, function or power under this Act; and
(b) the person discloses information to another person; and
(c) the information is *protected information; and
(d) the disclosure is not an *authorised disclosure.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
(2) Information is protected information if the information:
(a) either:
(i) is obtained by a person in the course of performing duties or functions, or exercising powers, under this Act; or
(ii) was information to which subparagraph (i) applied and is obtained by a person by way of an *authorised disclosure under section 323‑10, 323‑15 or 323‑20; and
(b) relates to a person other than the person who obtained it.
(3) A disclosure of information is an authorised disclosure if the disclosure is one that the person may make under section 323‑5, 323‑10, 323‑15, 323‑20, 323‑25, 323‑30 or 323‑35.
323‑5 Authorised disclosure: official duties
For the purposes of subsection 323‑1(3), a person may disclose information if the disclosure is made:
(a) in the course of performing a duty or function, or exercising a power, under this Act; or
(b) for the purpose of enabling a person to perform functions under the Medicare Australia Act 1973.
323‑10 Authorised disclosure: sharing information about insurers among agencies
(1) For the purposes of subsection 323‑1(3), a person to whom subsection (2) applies may disclose information to another such person if:
(a) the information relates to any or all of the following:
(i) a private health insurer;
(ii) an applicant to become a private health insurer;
(iii) a person carrying on *health insurance business;
(iv) a *director or *officer of a person mentioned in subparagraph (i), (ii) or (iii); and
(b) the information is not information of a kind specified in the Private Health Insurance (Information Disclosure) Rules as information that must not be disclosed under this section; and
(c) the disclosure is made in accordance with any requirements in the Private Health Insurance (Information Disclosure) Rules.
(2) This subsection applies to the following persons:
(a) the Minister;
(b) the Secretary of the Department;
(c) an APS employee in, or a person holding or performing the duties of an office in, the Department;
(d) a member of the Council;
(e) a person employed, or a consultant engaged, by the Council;
(f) the Private Health Insurance Ombudsman;
(g) an APS employee in, or a person holding or performing the duties of an office in, the Statutory Agency of the Private Health Insurance Ombudsman;
(h) the Medicare Australia CEO;
(i) an APS employee in, or a person holding or performing the duties of an office in, Medicare Australia.
323‑15 Authorised disclosure: sharing information about insurers other than among agencies
(1) For the purposes of subsection 323‑1(3), a person may disclose information to another person if:
(a) the information relates to any or all of the following:
(i) a private health insurer;
(ii) an applicant to become a private health insurer;
(iii) a person carrying on *health insurance business;
(iv) a *director or *officer of a person mentioned in subparagraph (i), (ii) or (iii); and
(b) the information is not information of a kind specified in the Private Health Insurance (Information Disclosure) Rules as information that must not be disclosed under this section; and
(c) the disclosure is made in accordance with any requirements in the Private Health Insurance (Information Disclosure) Rules; and
(d) the disclosure is, or is a kind of disclosure, certified by the Minister by written instrument to be in the public interest; and
(e) if there are any conditions specified in the certificate—the conditions are met.
(2) The Minister may specify conditions in a certificate under paragraph (1)(d) relating to the application of the certificate.
(3) A certificate under paragraph (1)(d) is not a legislative instrument.
323‑20 Authorised disclosure: public interest
(1) For the purposes of subsection 323‑1(3), a person may disclose information to another person if:
(a) the information does not relate to any of the following:
(i) a private health insurer;
(ii) an applicant to become a private health insurer;
(iii) a person carrying on *health insurance business;
(iv) a *director or *officer of a person mentioned in subparagraph (i), (ii) or (iii); and
(b) the information is not information of a kind specified in the Private Health Insurance (Information Disclosure) Rules as information that must not be disclosed under this section; and
(c) the disclosure is made in accordance with any requirements in the Private Health Insurance (Information Disclosure) Rules; and
(d) the disclosure is, or is a kind of disclosure, certified by the Minister by written instrument to be in the public interest; and
(e) if there are any conditions specified in the certificate—the conditions are met.
(2) The Minister may specify conditions in a certificate under paragraph (1)(d) relating to the application of the certificate.
(3) A certificate under paragraph (1)(d) is not a legislative instrument.
323‑25 Authorised disclosure: by the Secretary or Council if authorised by affected person
For the purposes of subsection 323‑1(3), the Secretary or the Council may disclose information to a person who is expressly or impliedly authorised by the person to whom the information relates to obtain it.
323‑30 Authorised disclosure: court proceedings
For the purposes of subsection 323‑1(3), a person who has, or has at any time had, a duty, function or power under this Act may disclose to a court information that relates to another person for the purposes of an action or proceeding before the court to which that other person is a party.
323‑35 Authorised disclosure: Council’s public information and agency cooperation functions
For the purposes of subsection 323‑1(3), the Council may disclose information to the extent necessary to perform the Council’s public information functions under subsection 264‑10(5) and agency cooperation functions under subsection 264‑10(6).
323‑40 Offence: disclosure of information obtained by certain authorised disclosures
A person commits an offence if:
(a) the person obtains information; and
(b) the person does so by way of an *authorised disclosure under section 323‑10, 323‑15 or 323‑20; and
(c) the person discloses the information; and
(d) the disclosure by the person is not an authorised disclosure.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
323‑45 Offence: soliciting disclosure of information
A person commits an offence if:
(a) the person solicits the disclosure of information from another person; and
(b) the information is *protected information; and
(c) the person knows, or ought reasonably to know, that the information is protected information; and
(d) the disclosure would not be an *authorised disclosure.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
323‑50 Offence: use etc. of unauthorised information
A person commits an offence if:
(a) information is disclosed to the person; and
(b) the information is *protected information; and
(c) the disclosure to the person is not an *authorised disclosure; and
(d) the person knows, or ought reasonably to know, that the disclosure to the person is not an authorised disclosure; and
(e) any of the following apply:
(i) the person solicited the disclosure of the information;
(ii) the person discloses the information;
(iii) the person uses the information.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
323‑55 Offence: offering to supply protected information
A person commits an offence if:
(a) the person:
(i) offers; or
(ii) holds himself or herself out as being able;
to supply (whether or not to a particular person) information about another person; and
(b) the person knows that the information is *protected information; and
(c) the supply would not be an *authorised disclosure.
Penalty: Imprisonment for 2 years or 120 penalty units, or both.
Division 328—Review of decisions
Several kinds of decisions made under this Act by the Medicare CEO, the Council, the Minister and the Private Health Insurance Ombudsman are reviewable by the Administrative Appeals Tribunal.
An application may be made to the Administrative Appeals Tribunal for the review of any of the following decisions:
Reviewable decisions | ||
Item | Decision | Provision under which decision is made |
1 | To reject an application for registration of a person in respect of a health insurance policy | section 23‑20 |
2 | To revoke a person’s registration in respect of a health insurance policy | section 23‑35 |
3 | To affirm an original decision of the Medicare Australia CEO rejecting a claim to be paid an amount under Division 26 | section 26‑25 |
4 | To refuse to make a declaration, or to revoke a declaration, that a facility is a *hospital | subsection 121‑5(6) |
4A | To specify a condition, in relation to a particular facility, to which a declaration that a facility is a *hospital is subject | paragraph 121‑7(1)(b) |
5 | To refuse an application for registration as a private health insurer | subsection 126‑20(1) |
6 | To grant an application, subject to terms and conditions, for registration as a private health insurer | subsection 126‑20(1) |
6A | To refuse an application for approval for a private health insurer to convert to being *registered as a for profit insurer | subsection 126‑42(5) |
7 | To refuse to make a declaration that the *solvency standard does not apply to a particular private health insurer | subsection 140‑15(2) |
8 | To impose conditions on a declaration that the *solvency standard does not apply to a particular private health insurer | subsection 140‑15(3) |
9 | To refuse to revoke or vary a declaration that the *solvency standard does not apply to a particular private health insurer | subsection 140‑15(6) or (7) |
10 | To refuse to revoke or vary conditions imposed on a declaration that the *solvency standard does not apply to a particular private health insurer | subsection 140‑15(6) or (7) |
11 | To refuse to revoke or vary a *solvency direction | subsection 140‑20(8) or (9) |
12 | To refuse to make a declaration that the *capital adequacy standard does not apply to a particular private health insurer | subsection 143‑15(2) |
13 | To impose conditions on a declaration that the *capital adequacy standard does not apply to a particular private health insurer | subsection 143‑15(3) |
14 | To refuse to revoke or vary a declaration that the *capital adequacy standard does not apply to a particular private health insurer | subsection 143‑15(6) or (7) |
15 | To refuse to revoke or vary conditions imposed on a declaration that the *capital adequacy standard does not apply to a particular private health insurer | subsection 143‑15(6) or (7) |
16 | To refuse to revoke or vary a *capital adequacy direction | subsection 143‑20(8) or (9) |
17 | To refuse to approve a restructure of the *health benefits funds of a private health insurer | subsection 146‑1(3) |
18 | To refuse to approve a transfer of the *health benefits funds of one or more private health insurers | subsection 146‑5(3) |
19 | To refuse to approve a restructure of the *health benefits funds of a private health insurer | section 149‑10 |
20 | To refuse to approve the appointment of a person as a private health insurer’s actuary | subsection 160‑1(5) |
21 | To declare under the Private Health Insurance (Insurer Obligations) Rules that a person is not eligible for appointment as a private health insurer’s actuary | subsection 160‑5(2) |
22 | To give a *prudential direction to a private health insurer | subsection 163‑15(1) |
23 | To refuse to revoke a *prudential direction | subsection 163‑15(3) |
24 | To disqualify a person from being or acting as a *director or *senior manager of a private health insurer | subsection 166‑20(1) |
25 | To refuse to revoke a disqualification of a *disqualified person | subsection 166‑20(3) |
26 | To refuse to determine that a person is not a *disqualified person | subsection 166‑25(3) |
27 | To specify conditions in a determination that a person is not a *disqualified person | subsection 166‑25(4) |
28 | To specify additional conditions to which determination that a person is not a *disqualified person is to be subject | subsection 166‑25(4) |
29 | To vary conditions to which determination that a person is not a *disqualified person is to be subject | subsection 166‑25(4) |
30 | To revoke a determination that a person is not a *disqualified person | subsection 166‑25(8) |
31 | To direct a private health insurer not to make a change that it proposes to make to its *rules | subsection 169‑10(2) |
32 | To refuse a request for a longer period for a private health insurer to respond to a request for an explanation | subsection 191‑1(3) |
33 | To refuse to consent to a private health insurer withdrawing or varying an undertaking | subsection 197‑1(3) |
34 | To give a direction to a private health insurer | section 200‑1 |
35 | To revoke a private health insurer’s status as a *participating insurer | section 206‑1 |
36 | To refuse to extend a period to report to the Private Health Insurance Ombudsman | subsection 241‑40(3) |
37 | To refuse to extend a period to give a record or information to the Private Health Insurance Ombudsman | subsection 250‑1(5) |
38 | To reject an application to become a *participating insurer | section 279‑5 |
39 | On reconsideration of a decision notifying a private health insurer in relation to a claim for payment under Division 279 | section 279‑45 |
40 | To affirm an original decision by the Medicare Australia CEO that an amount is recoverable as a debt under paragraph 282‑1(1)(a) or (b) | section 282‑15 |
41 | To affirm an original decision by the Medicare Australia CEO that an amount is recoverable as a debt under paragraph 282‑1(1)(h) in respect of a payment made to an individual | section 282‑15 |
42 | To affirm an original decision by the Medicare Australia CEO to set off a debt against an amount otherwise payable to a person or his or her estate | section 282‑15 |
43 | Not to waive, or to waive only a part of, an amount of *late payment penalty (other than late payment penalty in respect of an amount of *collapsed insurer levy) | section 307‑20 |
44 | Not to waive, or to waive only a part of, an amount of *collapsed insurer levy or *late payment penalty in respect of an amount of collapsed insurer levy | section 307‑25 |
(1) The Minister may, by writing, delegate all or any of his or her functions or powers under this Act (other than section 66‑10) to:
(a) the Secretary of the Department; or
(b) an SES employee, or acting SES employee, in the Department; or
(c) the Council.
(2) Without limiting subsection (1), the Minister may, by writing, delegate all or any of his or her functions or powers under Part 2‑2 or Part 6‑4 to:
(a) the Medicare Australia CEO; or
(b) an employee of Medicare Australia; or
(c) an APS employee in the Department.
(3) In performing a function or exercising a power under a delegation, the delegate must comply with any directions of the Minister.
(1) The Secretary of the Department may, by writing, delegate all or any of his or her functions or powers under this Act to an APS employee in the Department.
(2) In performing a function or exercising a power under a delegation, the delegate must comply with any directions of the Secretary.
(1) A statement, notice, application or other document is in the approved form if:
(a) it is in the form approved in writing by the person specified in the table as the approver of that form; and
(b) it contains a declaration signed by a person or persons as the form requires (see section 333‑15); and
(c) it contains the information that the form requires, and any further information, statement or document required by the approver, whether in the form or otherwise; and
(d) it is given in the manner (if any) required by the approver.
Person who approves forms | ||
Item | This person ... | is the approver of these forms ... |
1 | the Secretary of the Department | forms for which there is no other approver specified in this table. |
2 | the Medicare Australia CEO | forms under Part 2‑2. |
3 | the Council | (a) forms under Chapter 4, except a form under section 169‑10; (b) a form under subsection 310‑1(1), except a form that relates to *complaints levy; (c) a form under subsection 313‑20(1). |
(2) Despite subsection (1), a document that satisfies paragraphs (1)(a), (b) and (d) but not paragraph (1)(c) is also in the *approved form if it contains the information required by the approver. The approver must specify the requirement in writing.
(3) The approver may combine in the same *approved form more than one notice, statement, application or other document.
(4) The approver may approve a different *approved form for different kinds of private health insurers.
(5) The Medicare Australia CEO must not approve a form that requires a person to provide:
(a) the *tax file number of any person; or
(b) information about the physical, psychological or emotional health of any person.
A person who is required to do something in an *approved form must, if the form requires it, sign a declaration, or (if allowed by the form) have a declaration signed on the person’s behalf.
333‑20 Private Health Insurance Rules made by the Minister
(1) The Minister may, by legislative instrument, make Private Health Insurance Rules, specified in the second column of the table, providing for matters:
(a) required or permitted by the corresponding Chapter, Part or section specified in the third column of the table to be provided; or
(b) necessary or convenient to be provided in order to carry out or give effect to that Chapter, Part or section.
Private Health Insurance Rules made by Minister | ||
Item | Private Health Insurance Rules | Chapter/Part/section |
1 | Private Health Insurance (Incentives) Rules | Part 2‑2, section 206‑1, Part 6‑4 |
2 | Private Health Insurance (Lifetime Health Cover) Rules | Part 2‑3 |
3 | Private Health Insurance (Complying Product) Rules | Chapter 3 and section 188‑1 |
3A | Private Health Insurance (Benefit Requirements) Rules | Part 3‑3 |
4 | Private Health Insurance (Prostheses) Rules | Part 3‑3 |
5 | Private Health Insurance (Accreditation) Rules | section 81‑1 |
6 | Private Health Insurance (Health Insurance Business) Rules | Part 4‑2 |
7 | Private Health Insurance (Registration) Rules | Part 4‑3 |
8 | Private Health Insurance (Health Benefits Fund Policy) Rules | Part 4‑4 |
9 | Private Health Insurance (Data Provision) Rules | Part 4‑5 |
10 | Private Health Insurance (Health Benefits Fund Enforcement) Rules | Part 5‑3 |
11 | Private Health Insurance (Ombudsman) Rules | Part 6‑2 |
12 | Private Health Insurance (Council) Rules | Part 6‑3 |
13 | Private Health Insurance (Management) Rules | Part 6‑5 |
14 | Private Health Insurance (Levy Administration) Rules | Part 6‑6 |
15 | Private Health Insurance (Risk Equalisation Policy) Rules | Part 6‑7 |
16 | Private Health Insurance (Information Disclosure) Rules | Part 6‑8 |
(2) If, under this Act, Private Health Insurance Rules made by the Minister may modify a provision of this Act or another Act (including by modifying the effect, or the requirements, of such a provision), the Rules may do so by adding, omitting or substituting provisions (including effects or requirements of provisions).
333‑25 Private Health Insurance Rules made by the Council
(1) The Council may, by legislative instrument, make Private Health Insurance Rules, specified in the second column of the table, providing for matters:
(a) required or permitted by the corresponding Chapter, Part or section specified in the third column of the table to be provided; or
(b) necessary or convenient to be provided in order to carry out or give effect to that Chapter, Part or section.
Private Health Insurance Rules made by Council | ||
Item | Private Health Insurance Rules | Chapter/Part/section |
1 | Private Health Insurance (Health Benefits Fund Administration) Rules | Part 4‑4 |
2 | Private Health Insurance (Insurer Obligations) Rules | Part 4‑5 |
3 | Private Health Insurance (Risk Equalisation Administration) Rules | Part 6‑7 |
(2) To the extent that Private Health Insurance Rules made under this section deal with a matter that is dealt with in Private Health Insurance Rules made under section 333‑20, they must do so in a way that is not inconsistent with the Rules made under section 333‑20.
(3) If, under this Act, Private Health Insurance Rules made by the Council may modify a provision of this Act or another Act (including by modifying the effect, or the requirements, of such a provision), the Rules may do so by adding, omitting or substituting provisions (including effects or requirements of provisions).
The Governor‑General may make regulations prescribing matters:
(a) required or permitted by this Act to be prescribed; or
(b) necessary or convenient to be prescribed for carrying out or giving effect to this Act.
Note: See section 1‑10.
In this Act:
ADI (authorised deposit‑taking institution) means a corporation that is an ADI for the purposes of the Banking Act 1959.
adult means a person who is not a *dependent child.
applicable benefits arrangement means an applicable benefits arrangement within the meaning of the National Health Act 1953 as in force before 1 April 2007.
application provision is defined in subsection 217‑80(2).
applied Corporations Act provision is defined in subsection 217‑80(3).
appointed actuary, of a private health insurer, means the person holding an appointment by the insurer under section 160‑1.
approved form is a form that meets the requirements in section 333‑10.
assets, of a *health benefits fund, is defined in subsections 137‑1(3) to (4A).
authorised disclosure is defined in subsection 323‑1(3).
authorised officer is defined in subsection 313‑1(1).
base rate is defined in subsection 34‑1(2).
capital adequacy direction means a direction given under section 143‑20, and includes such a direction as varied under that section.
capital adequacy standard means a standard established under section 143‑5.
census day, for a levy, is defined in subsection 310‑1(2).
Chief Executive Officer means the Chief Executive Officer of the Council referred to in section 273‑1.
chief executive officer, of a private health insurer, is the person who is primarily and directly responsible to the *directors of the insurer for the general and overall management of the insurer.
collapsed insurer levy is defined in paragraph 304‑10(a).
Commissioner means the Commissioner of Private Health Insurance Administration referred to in paragraph 267‑1(1)(a).
complaints levy is defined in paragraph 304‑10(b).
complying health insurance policy is defined in section 63‑10.
complying health insurance product is defined in section 63‑5.
constitutional corporation means a corporation to which paragraph 51(xx) of the Constitution applies.
Council means the Private Health Insurance Administration Council continued in existence under Part 6‑3.
Council administration levy is defined in paragraph 304‑10(c).
Council‑supervised obligation is defined in section 185‑10.
cover has a meaning affected by section 69‑5.
declaration of contravention means a declaration under section 203‑5.
dependent child means a person:
(a) who is:
(i) aged under 18; or
(ii) a dependent child under the *rules of the private health insurer that insures the person; and
(b) who is not aged 25 or over; and
(c) who does not have a partner.
Deputy Commissioner means the *member (if any) appointed under subsection 267‑5(2) to be the Deputy Commissioner.
director has the same meaning as in the Corporations Act 2001.
disqualified person is defined in section 166‑15.
employee health benefits scheme is defined in section 121‑15.
enforceable obligation is defined in section 185‑5.
external management means management under Division 217 and Part 6‑5.
external manager, in relation to a *health benefits fund, means a person appointed under section 217‑10 as the external manager of the fund.
Federal Court means the Federal Court of Australia.
fringe benefit means:
(a) a fringe benefit as defined by subsection 136(1) of the Fringe Benefits Tax Assessment Act 1986; and
(b) a benefit that would be a fringe benefit (as defined by subsection 136(1) of that Act) if paragraphs (d) and (e) of the definition of employer in that subsection of that Act were omitted.
general treatment is defined in section 121‑10.
gold card is defined in subsection 34‑15(3).
health benefits fund is defined in section 131‑10.
health care provider means:
(a) a person who provides goods or services as, or as part of, *hospital treatment or *general treatment; or
(b) a person who manufactures or supplies goods provided as, or as part of, hospital treatment or general treatment.
health insurance business is defined in Division 121.
health‑related business is defined in section 131‑15.
holder, of an insurance policy, means a person who is insured under the policy and who is not a *dependent child.
hospital is defined in subsection 121‑5(5).
hospital cover is defined in section 34‑15.
hospital‑substitute treatment is defined in section 69‑10.
hospital treatment is defined in section 121‑5.
improper discrimination:
(a) in relation to an insurer who is not a *restricted access insurer—has the meaning given by subsection 55‑5(2); and
(b) in relation to a restricted access insurer—has the meaning given by subsection 55‑5(2) as affected by subsection 55‑5(3).
incentive amount is defined in section 23‑5.
incentive payments scheme means the scheme provided for by Division 26.
ineligible for Medicare, in relation to a person, means not an eligible person within the meaning of the Health Insurance Act 1973.
inspector means a person appointed as an inspector under section214‑1, and (except in section 214‑40) includes a person exercising powers under a delegation under section 214‑40.
insurance is defined in section 5‑1.
late payment penalty means a late payment penalty incurred under section 307‑5 in respect of a *private health insurance levy.
levy‑related document is defined in subsection 313‑1(3).
lifetime health cover base day is defined in section 34‑25.
makes a capital payment is defined in subsection 137‑5(3).
manager, in relation to a *health benefits fund, means an*external manager or *terminating manager of the fund.
medical practitioner means a medical practitioner within the meaning of the Health Insurance Act 1973.
Medicare Australia CEO means the Chief Executive Officer of Medicare Australia.
medicare benefit means a medicare benefit under Part II of the Health Insurance Act 1973.
medicare eligibility day is defined in subsection 34‑25(3).
member means a member of the Council and includes the *Commissioner.
net asset position, of a *health benefits fund, means the difference between:
(a) the *assets of the fund; and
(b) the *policy liabilities and other liabilities of the fund that the private health insurer conducting the fund has incurred for the purposes of the fund.
new arrival is defined in subsection 34‑25(2).
occupier, of *premises, includes:
(a) the person in charge or control, or apparently in charge or control, of the premises; or
(b) a person who represents, or apparently represents, that person.
officer, of a private health insurer, means:
(a) a *director of the insurer; or
(b) a *chief executive officer of the insurer; or
(c) a person who makes, or participates in making, decisions that affect the whole, or a substantial part, of the business of the insurer.
officer, of a subject of a complaint under Division 241 or an investigation under Division 244, means:
(a) if the subject is an individual—the individual; or
(b) if the subject is a private health insurer—a person who is an *officer of the insurer; or
(c) if the subject is a company within the meaning of the Corporations Act 2001—a *director of the company; or
(d) if the subject is an incorporated association—a member of the management committee of the association; or
(e) if the subject is an unincorporated entity—a member of the governing body of the entity; or
(f) if the subject is a partnership—a partner in the partnership.
old Schedule 2 is defined in subsection 34‑10(5).
overseas has a meaning affected by section 34‑30.
participant, in relation to the *premiums reduction scheme, means:
(a) a person who is registered as a participant in the scheme under subsection 23‑15(3); or
(b) a person who has applied to be registered as a participant in the scheme under subsection 23‑15(1) and whose application has not been refused.
participating insurer means:
(a) a private health insurer approved by the Minister under subsection 279‑5(2); or
(b) a private health insurer that has applied under subsection 279‑5(1) to be approved and whose application has not been rejected.
permitted days without hospital cover is defined in section 34‑20.
personal information means information or an opinion (including information or an opinion forming part of a database), whether true or not, and whether recorded in a material form or not, about an individual whose identity is apparent, or can reasonably be ascertained, from the information or opinion.
policy group, of a *health benefits fund, is defined in subsection 146‑1(5).
policy holder, of a *health benefits fund, means a *holder of a policy that is *referable to the fund.
policy liability of a private health insurer means:
(a) a liability that has arisen under an insurance policy; or
(b) a liability that, subject to the terms and conditions of an insurance policy, will arise on the happening of an event, or at a time, specified in the policy.
pre‑existing condition is defined in section 75‑15.
premises includes the following:
(a) a structure, building, vehicle or vessel;
(b) a place (whether enclosed or built on);
(c) a part of a thing referred to in paragraph (a) or (b).
premiums reduction scheme means the scheme provided for by Division 23.
private health insurance arrangement includes any of the following:
(a) a *private health insurance policy or a *product;
(b) an agreement or arrangement between a private health insurer and a *health care provider;
(c) an agreement or arrangement between a private health insurer and another person (other than a health care provider) that relates to insurance in relation to *hospital treatment or *general treatment;
(d) an agreement or arrangement between two or more health care providers that relates to insurance in relation to hospital treatment or general treatment;
(e) Private Health Insurance (Complying Product) Rules made for the purposes of item 1 or 5 of the table in subsection 72‑1(2);
(f) Private Health Insurance (Prostheses) Rules made for the purposes of item 4 of the table in subsection 72‑1(2);
(g) an arrangement between a private health insurer and a *private health insurance broker;
(h) an arrangement between a private health insurance broker and a person seeking to become insured under a private health insurance policy.
private health insurance broker means a person:
(a) who deals (otherwise than by carrying on *health insurance business) in insurance policies that *cover *hospital treatment or *general treatment or both; and
(b) who acts on behalf of persons seeking to become insured under those policies.
private health insurance levy is defined in section 304‑10.
Private Health Insurance Ombudsman means the Private Health Insurance Ombudsman appointed for the purposes of Part 6‑2.
private health insurance policy means an insurance policy that *covers *hospital treatment or *general treatment or both (whether or not it also covers any other treatment or provides a benefit for anything else).
private health insurer means a person registered under Part 4‑3.
product is defined in subsection 63‑5(2).
product subgroup is defined in subsection 63‑5(2A).
protected information is defined in subsection 323‑1(2).
prudential direction means a direction given under section 163‑15.
prudential matters is defined in subsection 163‑1(2).
prudential standard means a standard established under subsection 163‑1(1).
records, of a subject of a complaint under Division 241 or an investigation under Division 244, includes any of the following that are in the possession, or under the control, of the subject:
(a) the constitution and *rules of the subject, if the subject is a private health insurer;
(b) the internal training manuals and related documents of the subject;
(c) any documents relevant to a *private health insurance arrangement to which the subject is a party or that applies to the subject;
(d) to the extent that the complaint or investigation relates to the subject’s dealings with a particular person—the subject’s records relating to its dealings with that particular person including correspondence, internal memoranda, emails, and recordings of taped conversations;
whenever those records came into existence.
referable: an insurance policy is referable to a *health benefits fund if:
(a) the fund is identified under paragraph 93‑15(c) as the fund to which the policy is referable (and the policy has not been made referable to another *health benefits fund under Division 146); or
(b) the policy has been made referable to the fund under Division 146.
registered as a for profit insurer means a private health insurer that is registered under Part 4‑3 as a for profit insurer.
responsible insurer means:
(a) for a *health benefits fund that is under *external management—the private health insurer that was conducting the fund prior to the appointment of the *external manager of the fund; or
(b) for a health benefits fund that is under *terminating management—the private health insurer that was conducting the fund prior to the appointment of the *terminating manager of the fund.
restricted access group is defined in subsection 126‑20(7).
restricted access insurer means a private health insurer that is registered under Part 4‑3 as a restricted access insurer.
risk equalisation jurisdiction is defined in subsection 146‑1(6).
risk equalisation levy is defined in paragraph 304‑10(d).
Risk Equalisation Trust Fund means the Private Health Insurance Risk Equalisation Trust Fund continued in existence under Part 6‑7.
rules, of a private health insurer, means the body of rules established by the insurer that relate to the day‑to‑day operation of the insurer’s *health insurance business and (if any) *health‑related business.
schedule fee means the Schedule fee within the meaning of Part II of the Health Insurance Act 1973.
search powers means powers to search for, inspect, take extracts from, and make copies of, documents.
senior manager of a private health insurer means a person who has or exercises any of the senior management responsibilities (within the meaning of the *prudential standards) for the insurer.
solvency direction means a direction given under section 140‑20, and includes such a direction as varied under that section.
solvency standard means a standard established under section 140‑5.
standard information statement is defined in section 93‑5.
tax file number means a tax file number as defined in section 202A of the Income Tax Assessment Act 1936.
terminating management means management under Division 149 and Part 6‑5.
terminating manager, in relation to the *health benefits funds of a private health insurer, means a person appointed under paragraph 149‑10(2)(a) or Division 220 as the terminating manager of the funds.
termination day, in relation to the *health benefits funds of a private health insurer, is defined in subsection 149‑20(2).
transfer, in relation to a person, is defined in section 75‑10.
up to date, in relation to a *standard information statement, is defined in subsection 93‑1(2).
voluntary deed of arrangement means:
(a) a deed of arrangement agreed on at a meeting of a kind referred to in section 217‑45; or
(b) such a deed as varied in accordance with the Health Benefits Fund Enforcement Rules.
waiting period is defined in section 75‑5.
[Minister’s second reading speech made in—
House of Representatives on 7 December 2006
Senate on 26 February 2007]
(209/06)