GUIDE TO DETERMINING IMPAIRMENT AND COMPENSATION (GARP M)
INTRODUCTION
Purpose
This Guide is to be applied to assess the degree of impairment from service injury or disease. Its provisions are binding on the Military Rehabilitation and Compensation Commission, the Veterans’ Review Board, and the Administrative Appeals Tribunal.
Legal background
The Military Rehabilitation and Compensation Act 2004 provides for periodic payments to be made to members for impairment resulting from service injuries or diseases as defined in section 5 of the Act.
Part 2 of Chapter 4 of the Act provides that periodic payments are payable only if certain thresholds are reached as determined by reference to the extent of the veteran’s incapacity as assessed in accordance with this Guide. Subsection 67(1) of the Act provides that the Guide prepared by the Military Rehabilitation and Compensation Commission sets out:
(a) criteria to be used in deciding the degree of impairment of a person resulting from a service injury or disease; and
(b) methods by which the degree of that impairment can be expressed in impairment points on a scale from 0 to 100; and
(c) criteria to be used in assessing the effect of a service injury or disease on a person’s lifestyle; and
(d) methods by which the effect of a service injury or disease on a person’s lifestyle can be expressed as a numerical rating; and
(e) methods by which the impairment points of a person, and the effect on a person’s lifestyle, from a service injury or disease can be used to determine the compensation payable to the person under this Part by reference to the maximum compensation that can be payable to a person under this Part.
In addition the Guide, in accordance with subsection 67(2) of the Act
(a) specifies different methods under paragraph (1)(e) for:
(i) service injuries or diseases that relate to warlike service or non‑warlike service; and
(ii) other service injuries or diseases; and
(b) specifies a method for determining the compensation payable to a person who has both:
(i) a service injury or disease that relates to warlike service or non‑warlike service; and
(ii) another service injury or disease.
Definitions
In this Guide, unless a contrary intention appears:
accepted condition means an injury or disease that has been determined to be caused by service.
Act means the Military Rehabilitation and Compensation Act 2004 as amended from time to time.
add means find the arithmetic sum of two or more numbers.
clinical features includes signs and symptoms.
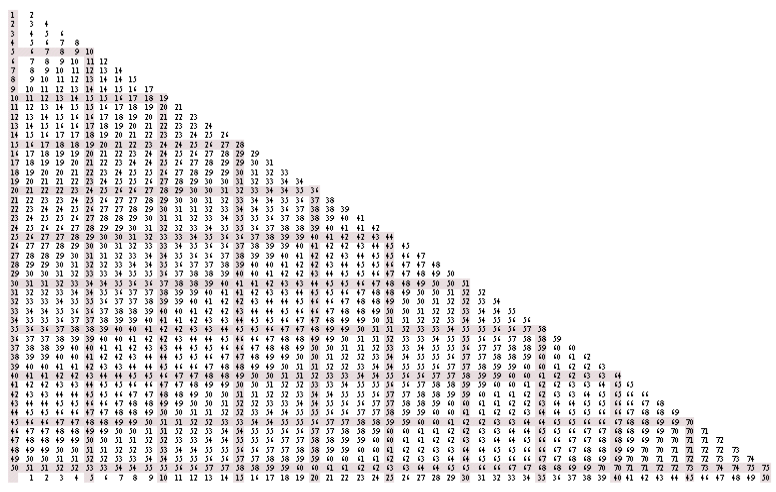
combine means produce a result by combining two or more numbers by applying Chart 18.1 (Combined Values Chart) in Chapter 18 in accordance with that Chapter.
Commission means the Military Rehabilitation and Compensation Commission.
condition means an injury or a disease.
defence-caused injury and defence-caused disease have the meaning given in section 70 of the VEA.
disease means:
(a) any physical or mental ailment, disorder, defect or morbid condition (whether of sudden onset or gradual development); or
(b) the recurrence of such an ailment, disorder, defect or morbid condition;
but does not include:
(c) the aggravation of such an ailment, disorder, defect or morbid condition; or
(d) a temporary departure from:
(i) the normal physiological state; or
(ii) the accepted ranges of physiological or biochemical measures;
that results from normal physiological stress (for example, the effect of exercise on blood pressure) or the temporary effect of extraneous agents (for example, the effect of alcohol on blood cholesterol levels).
GARP V means the Guide to the Assessment of Rates of Veterans’ Pensions, Fifth Edition (GARP V), instrument No.9 of 1997, as amended or remade from time to time.
Guide means this Guide to Determining Impairment and Compensation.
impairment, in relation to a person, means the loss, the loss of the use, or the damage or malfunction, of any part of the person’s body, of any bodily system or function, or of any part of such a system or function.
impairment rating means a measure of the degree of medical impairment on a scale of 0 to 100.
injury means any physical or mental injury (including the recurrence of a physical or mental injury) but does not include:
(a) a disease; or
(b) the aggravation of a physical or mental injury.
lifestyle points means the number of points determined using the tables in Chapter 22 of this Guide.
lifestyle averaged points means the total of lifestyle points added together and averaged for each of the tables used.
lump sum means the amount payable after determining the periodic payment for a service injury or disease and converted to a single dollar amount in accordance with the tables provided by the Australian Government Actuary for that purpose.
member or former member means a member or former member of the Defence Force who serves or served on or after 1 July 2004.
non-accepted condition means any injury or disease that has not been determined under the Act to be service related or has been determined under the Act not to be service related.
periodic payment means the amount determined by reference to the tables in this guide for warlike and non-warlike service or for peacetime service and the maximum amount payable under the relevant provision of the Act.
service means service in the Defence Force which is warlike service, non‑warlike service or peacetime service as determined by the Minister for Defence from time to time.
service disease has the meaning given by section 27, subsections 29(1) and (2), and section 30 of the Act.
Note: A reference to a service disease being contracted includes a reference to a disease being aggravated by defence service (see section 7 of the Act).
service injury has the meaning given by section 27, subsections 29(1) and (2), and section 30 of the Act.
Note: A reference to a service injury being sustained includes a reference to an injury being aggravated by defence service (see section 7 of the Act).
SRCA means the Safety, Rehabilitation and Compensation Act 1988.
Statement of Principles means:
(a) a Statement of Principles determined by the Repatriation Medical Authority under section 196B of the VEA and to which section 19 of the Consequential and Transitional Provisions Act 2004 applies; or
(b) a determination made by the Commission under subsection 340(2) or (3) of the Act.
VEA means the Veterans’ Entitlements Act 1986.
veteran means a member or former member of the Defence Force (including a deceased person) under section 5 of the MRCA in respect of whom an injury or disease has been determined to be caused by that service.
war-caused injury and war-caused disease have the meaning given in section 9 of the VEA.
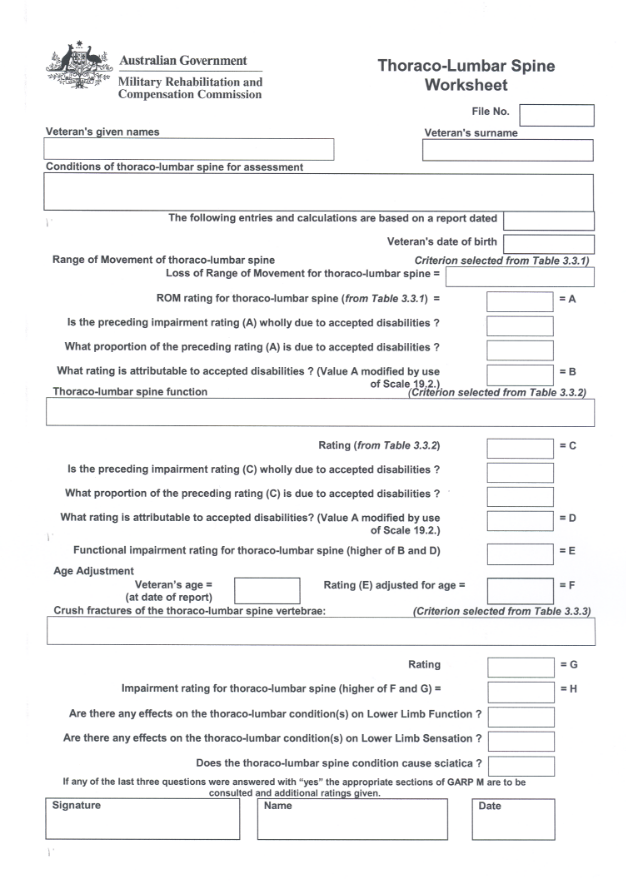
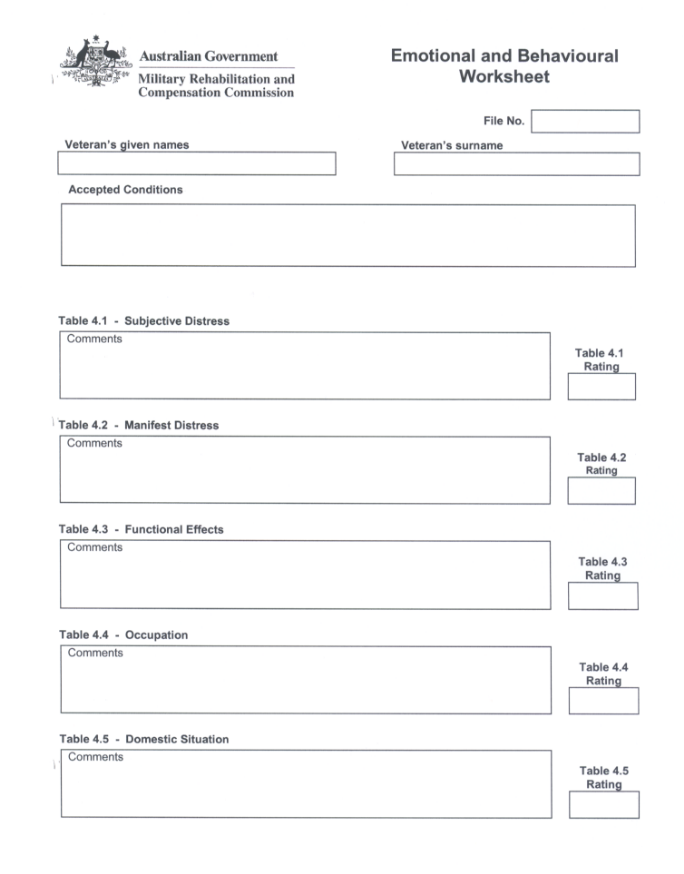
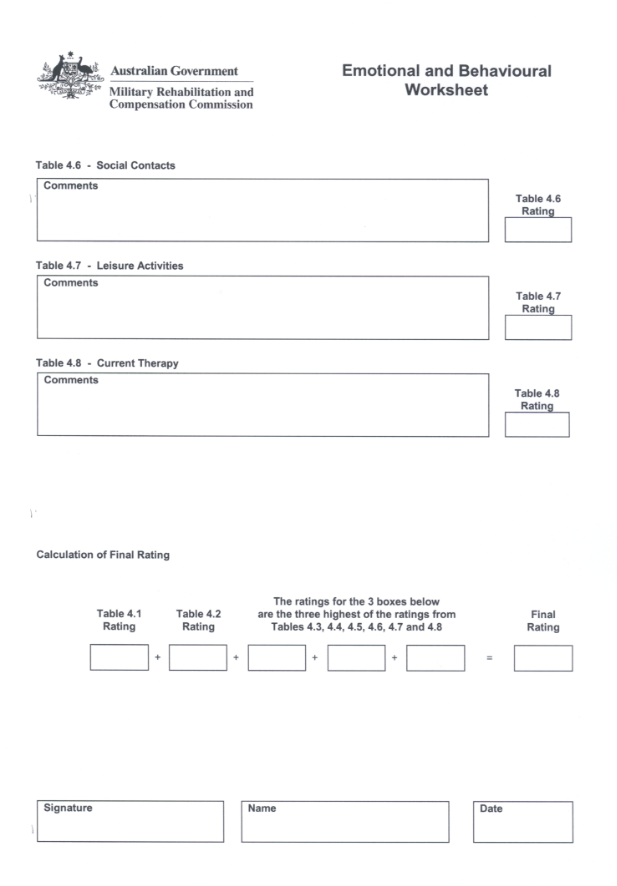
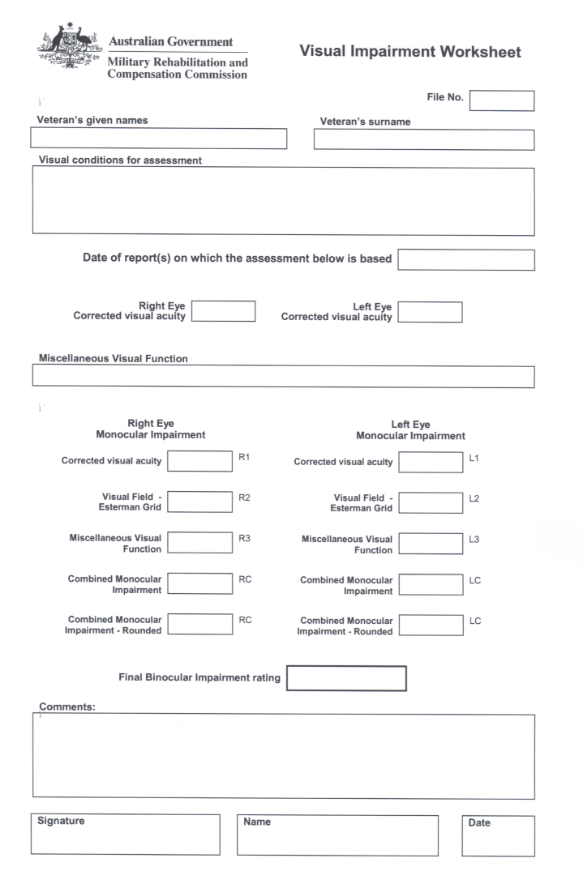
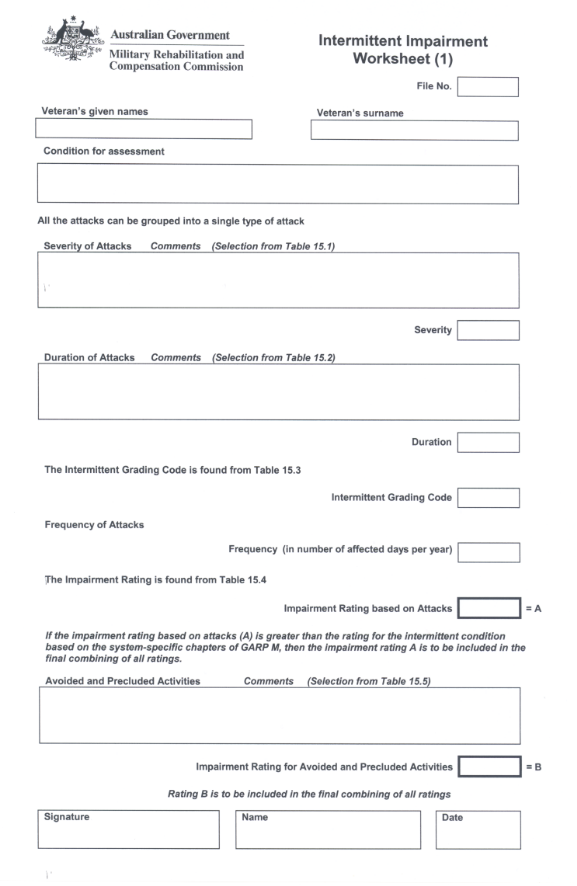
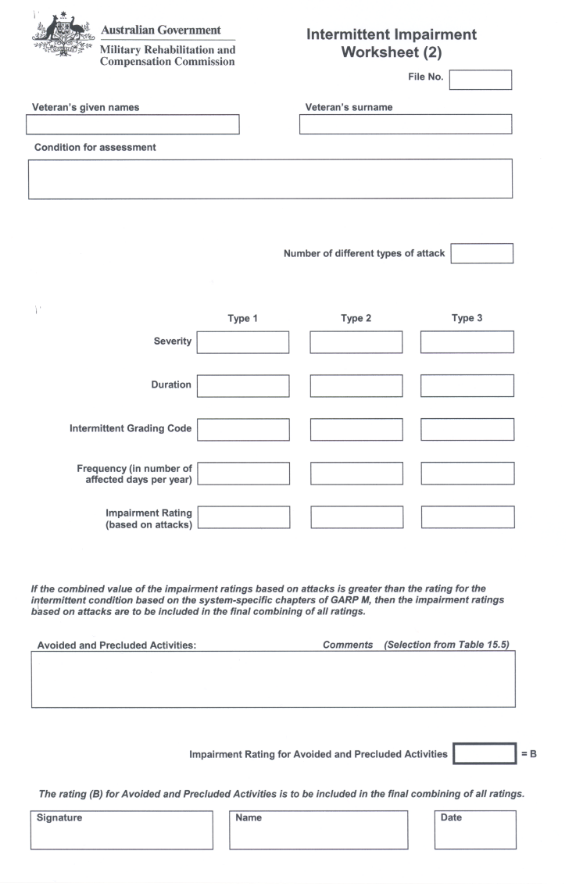
worksheet means a page or pages of this Guide, identified as such, that gives a structure by which certain calculations may be set out to assist in determining an impairment rating.
Definitions of words and phrases that are used in only one chapter are to be found in that chapter.
Acknowledgment of sources
The Guide to the Assessment of Rates of Veterans’ Pensions Fifth Edition, Part A Chapters 1–12 and Part B Chapters 13-17 and Part C Chapters 18-21 are the basic tables for this Guide.
That publication acknowledges that the following published works were found to be useful in the preparation of the VEA Guide (GARP V) and therefore were basic to this Guide as well:
Guides to the Evaluation of Permanent Impairment, 4th edition, American Medical Association, 1993;
International Classification of Impairments, Conditions, and Handicaps, World Health Organisation, Geneva, 1980; and
Publication No 118 of the National Acoustic Laboratories, Improved Procedure for Determining Percentage Loss of Hearing, by J. Macrae, Australian Government Publishing Service, Canberra, 1988.
HOW TO USE THIS GUIDE
The subject of assessment
This Guide is to be applied to assess the impairment points due to injuries or diseases, or both, that are determined to be service related.
In making any determination on the impairment the clinical features of injuries or diseases are to be taken into account. Sequelae of conditions can only be assessed after the sequelae have been determined to be service related.
The elements of whole person impairment and compensation
The two elements required to determine a periodic payment are medical impairment and lifestyle. Impairment is dealt with in Chapters 1 – 21 of this Guide. Lifestyle effects are dealt with separately and are described in Chapter 22 of this Guide.
Chapters 1 to 16 of this Guide contain two principal types of tables. Physical loss is to be rated against criteria in “Other Impairment” tables. Functional loss is to be rated against criteria in “Functional Loss” tables.
Greater emphasis has been given throughout this Guide to functional loss as a basis for assessment. It is measured by reference to an individual’s performance efficiency compared with an average, healthy person of the same age and sex, in a set of defined vital functions. This is a means of compensating for the loss of ability to perform everyday functions.
Each table contains benchmark values, generally at intervals of five points. In some cases the range between nil and five includes a rating of two points. In some other cases intervals are greater than five points because lesser increments of impairment cannot be distinguished.
Each benchmark is a threshold value, that is, the rating applies only if the threshold is achieved or exceeded. Ratings are not to be rounded up to the next benchmark. Similarly, ratings between benchmark values contained in the tables are not to be interpolated.
In some tables more than one criterion is stated opposite a benchmark value. The different criteria are marked by dot points. Where more than one criterion is stated for a particular value, the condition being assessed has to satisfy one of the criteria in order to attract the impairment rating of that value.
Each chapter contains step-by-step instructions to be followed in the use and application of the tables.
Determining compensation payable
This Guide specifies the only way of determining the amount of compensation payable is by reference to the maximum compensation that can be paid. The maximum is specified in the Act as a weekly amount. It becomes payable only when a person’s impairment rating reaches 80 points.
The Guide includes tables that will give a compensation factor for different impairment and lifestyle ratings. Different tables are used for warlike and non-warlike service and for peacetime service. The maximum compensation is multiplied by the compensation factor to give the weekly amount of compensation payable.
Medical impairment
Under this Guide medical impairment has two components:
(a) physical loss of, or disturbance to, any body part or system; and
(b) the resultant functional loss.
Whole person impairment
Medical impairment is expressed in impairment points, out of a maximum rating of 100. On this scale, zero corresponds to no impairment or negligible impairment from accepted conditions, and 100 points corresponds to death. Effectively, impairment points are percentages of the impairment of the whole person.
Loss of hearing, loss of taste, loss of smell, loss of a finger or of a toe as impairment for a single condition can be compensated for under this Guide only if a threshold value of 5 impairment points is reached. Any combination of loss from conditions that delivers a combined impairment of 10 or more will attract compensation.
Example
Loss of taste rated at 5 impairment points and mild reflux rated at 2 impairment points.
A payment for loss of taste is permitted but, since 5 plus 2 is 7 and does not reach the threshold of 10 impairment points, no other payment is made.
Loss of taste rated at 5 impairment points and reflux rated at 5 impairment points.
The reflux 5 points when combined with the loss of taste reaches the threshold of 10 impairment points and so payment is made on the basis of 10 impairment points.
Functional loss
Medical impairment is measured chiefly by loss of vital functions and is addressed in the twelve system specific chapters of this Guide, as follows:
Cardio-Respiratory Impairment
Hypertension and Non-Cardio Vascular Conditions
Impairment of Spine and Limbs
Emotional and Behavioural
Neurological Impairment
Gastro-intestinal Impairment
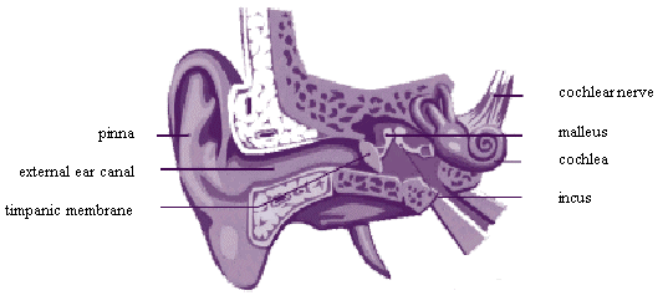
Ear, Nose, and Throat Impairment
Visual Impairment
Renal and Urinary Tract Function
Sexual Function, Reproduction, and Breasts
Skin Impairment
Endocrine and Haemopoietic Impairment
Other Impairment
Other Impairment is the physical loss of, or disturbance to, any body part or system. This concept is extended in some chapters in this Guide to include discomfort, pain, poor prognosis and other, less tangible, effects of accepted conditions.
Lifestyle effects
Lifestyle effects are to be assessed by applying Chapter 22 of this Guide in accordance with that Chapter.
The Tables
Types of Tables
There are several different sorts of tables used in GARP V that remain common to both GARP V and this Guide. Basically these are various impairment tables, the lifestyle tables and the tables to deal with more complex matters.
However the MRCA requires the Commission to specify two particular tables that are not used in GARP V or the VEA. These are tables that arise from the method specified by the Commission to determine compensation payable for warlike and non-warlike as distinct from peacetime service (see Tables 1 and 2 of Chapter 23). In addition the Commission must specify a method for determining compensation payable when a mixture of warlike (or non-warlike) and peacetime service causes the whole person impairment
Gender Use
Some tables are for men only, some for women only, and others (the majority) are not gender specific. Each table is clearly marked in the top right hand corner:
the symbol | 
| means that the table is only to be used for the assessment of female veterans; |
the symbol | 
| means that the table is only to be used for the assessment of male veterans; |
the symbol | 
| means that the table is used for either male or female veterans. |
Age Adjustment
Some tables incorporate age dependent criteria. Some other tables have no such criteria and require subsequent age adjustment by applying tables provided for that purpose.
Each table is clearly marked in the bottom left hand corner with instructions on age adjustment for ratings derived from that table.
Conversion Factor Tables
The Commission is required by paragraph 67(1)(e) to provide methods that enable Lifestyle to be combined with Impairment to give compensation for each type of service by reference to the maximum compensation payable. These are set out as compensation factors in tables in Chapter 23 and include a different set of factors to be used for warlike and non-warlike service and for other service as provided for in the Act (see subsection 67(2)).
Non-system specific assessments
This Guide has chapters describing alternate methods of assessing certain conditions:
Chapter 13 — Negligible Impairment
Chapter 14 — Malignant Conditions
Chapter 15 — Intermittent Impairment
Chapter 16 — Activities of Daily Living
Chapter 17 — Disfigurement
Conditions and their sequelae
Only the clinical features of an accepted condition may be taken into account in making an assessment. If the accepted condition causes some other distinct and diagnosable condition (sequela), the symptoms of the sequela cannot be taken into account when assessing the original accepted condition.
Sequelae can only be assessed when they have been separately determined to be service related.
Applying the instructions
To the extent of any inconsistency between an instruction in this “How to use the Guide” and a specific instruction concerning a particular matter in this Guide, the specific instruction in this “How to use the Guide” is to apply to that particular matter.
Duration of assessment period or date of determination and commencement of periodic payment and permanent impairment and interim payments
Assessment can only be made by reference to the available medical and other material that, of necessity, relates to a particular point or period in time.
The assessment of the impairment and lifestyle ratings must be based on the Commission’s reasonable satisfaction on the available material. If there is a significant change in impairment during the course of an investigation a payment may still be made as an interim payment. Interim payments are made until the Commission is satisfied that the condition has stabilised at an impairment level.
If the condition worsens after the last payment is made the person may claim additional compensation for the worsening and further periodic payments or lump sums can be made.
Apportionment of impairment ratings
It is sometimes necessary, for an accepted condition, to compare an impairment rating derived from one table with an impairment rating derived from another table. When two or more conditions contribute to the impairment ratings from either or both tables, and comparison is necessary, the method called “apportionment” is to be applied before making the comparison.
Details of the application of apportionment are given in Chapter 20.
Apportionment between tables
If a condition can be rated using both a functional loss table and an “Other Impairment” table, only the higher of the two ratings is to be given to the veteran.
Paired organ policy
The paired organ policy applies to eyes, kidneys etc and is described in detail in Chapter 21 of this Guide.
Impairment for specific disabilities
The Act provides only for impairment and does not convert that rating into a degree of incapacity like the VEA requires. Instead the impairment and lifestyle ratings determine a factor, not a degree of incapacity. Incapacity applies to ability to perform military service or a civilian occupation. Therefore, Chapter 24, “Degree of incapacity for specific disabilities” of GARP V, has been omitted. Instead impairment ratings are based only on the Tables from Chapter 1 to 21 of this Guide.
MEDICAL IMPAIRMENT
PART A: SYSTEM SPECIFIC ASSESSMENT
CHAPTER 1
CARDIORESPIRATORY IMPAIRMENT
INTRODUCTION
Cardiorespiratory impairment results from conditions that affect the function of the heart or lungs. The procedures described in this chapter are to be applied in assessing most conditions of the heart and lungs, and will usually also be appropriate for conditions affecting the function of the thorax or diaphragm, lesions of the nerves that supply the muscles of respiration, and conditions such as anaemia. The principal exception is any condition which is predominantly intermittent in nature and which would be better assessed by applying Chapter 15 (Intermittent Impairment).
Different procedures (described in Chapter 2) are to be applied to assess hypertension and non-cardiac vascular conditions (such as aortic aneurysm and varicose veins).
In general, cardiorespiratory impairment is to be measured by reference to exercise tolerance. Exercise tolerance is quantified in terms of METs (see pages 11–12). However, if a respiratory component is present, measurements of lung function, such as forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and maximal expiratory flow (MEF 25–75) are to be used in addition to exercise tolerance. FEV1 and FVC are to be measured by spirometry. For the purposes of assessment in accordance with this Guide, the terms “MEF 25–75” and “FEF 25–75” (forced expiratory flow between 25% and 75% of the vital capacity) are to be taken as equivalent.
The conversion of loss of exercise tolerance and measurements of lung function into an impairment rating is set out in Table 1.2 and Table 1.3.
Certain cardiorespiratory conditions cannot be rated by applying exercise tolerance. These include:
- conditions that do not decrease exercise tolerance;
- conditions that do not produce symptoms; and
- intermittent conditions.
“Exercise tolerance” refers to a person’s ability to exercise from a cardiorespiratory point of view rather than to a person’s total ability to exercise. For example, a veteran who has osteoarthritis of both knees may be greatly limited in walking but may still be able to swim a considerable distance. Such a veteran would still have good exercise tolerance from a cardiorespiratory point of view, though total ability to exercise would be reduced.
A veteran whose ability to exercise has been significantly reduced by other conditions (such as musculoskeletal conditions or being grossly overweight), or who no longer has cardiac or respiratory symptoms on exercise, cannot always be given an appropriate impairment rating for reduced exercise tolerance. However, the need to apply Chapter 19 (Partially Contributing Impairment) should always be considered before disregarding exercise tolerance figures.
Calculation of the impairment rating for accepted cardiorespiratory conditions
Follow the steps below to determine the impairment rating for cardiorespiratory conditions:
(Each step is elaborated in the following pages.)
Step 1 | Establish what cardiorespiratory conditions are present. | Page 7 |
Step 2 | Assess the information that is available and decide whether it is reliable and sufficient. | Page 8 |
Step 3 | Determine the impairment rating based on effort tolerance. | Page 9 |
Step 4 | (Omit this step if no respiratory disease is present.) Determine the impairment rating based on measurements of lung function. | Page 13 |
Step 5 | Determine the total accepted cardiorespiratory functional impairment rating. | Page 21 |
Step 6 | Consider the effects of cardiac failure (if any). | Page 24 |
Step 7 | Moderate the total cardiorespiratory functional impairment rating to allow for effects of any non-accepted conditions. | Page 24 |
Step 8 | Determine whether any ratings from the relevant Other Impairment tables apply (Tables 1.7, 1.8, 1.9, 1.10). | Page 25 |
Step 1: Establish what cardiorespiratory conditions are present.
For the purpose of assessing cardiorespiratory impairment, both the accepted and the non-accepted conditions are be taken into account. Both will affect the way in which cardiorespiratory functional impairment is calculated. (Their combined effect is taken into account in the application of Table 1.5 in Step 5.)
Any non-accepted conditions are to be subsequently allowed for by applying Chapter 19 (Partially Contributing Impairment) — see Step 7.
When considering the question: ‘What cardiorespiratory conditions are present in this veteran?’, it is not appropriate to rely simply on a list of accepted conditions. Both previously claimed but rejected cardiorespiratory conditions and unclaimed cardiorespiratory conditions may also be present.
Step 2: Assess the information that is available and decide whether it is reliable and sufficient.
To make a reliable cardiorespiratory assessment, there should be an adequate medical history of the veteran’s cardiorespiratory conditions. In addition, there should be information relating to the veteran’s effort tolerance and, if any respiratory disease is present, there should also be one or more sets of spirometry or other physiological measurements of respiratory function. The criteria by which the evaluation of the information is to be made are set out below.
Medical history
An adequate history of the veteran’s illness and a description of the current symptoms and details of the current treatment should be available.
The history should be reviewed at the start of the cardiorespiratory assessment procedure to establish whether any major cardiorespiratory event (for example a myocardial infarction or bypass surgery) has occurred within the period of assessment.
An examination of the history will indicate whether any Other Impairment ratings (from Tables 1.7, 1.8, 1.9, 1.10) are applicable. For example, in the case of ischaemic heart disease, the history will reveal whether the veteran has had any myocardial infarctions, whether coronary bypass surgery has been performed and the outcome of any such surgery. In other cases, for example when respiratory disease is present, the current treatment will reveal whether any Other Impairment rating for cardiorespiratory conditions is applicable.
In long-standing respiratory conditions, there will often be a disease complex present that is more extensive than that implied by the original diagnostic label. For example, asthma may lead to chronic obstructive respiratory disease and chronic bronchitis may lead to small airways disease. Such extensions of the disease process are to be assessed as part and parcel of the original condition unless there is clear reason why they should not be — for example, they have been determined to be non-accepted conditions.
Effort tolerance
Effort tolerance information should always be obtained except if the veteran has a condition that renders the collection of reliable effort tolerance information impracticable.
Examples of conditions that may render the collection of reliable effort tolerance information impracticable include:
- hemiparesis following a stroke;
- quadriplegia or hemiplegia;
- severe arthritis of the lower limbs; and
- certain mental conditions such as dementia (in which the veteran’s ability to co-operate or provide useful information may be restricted).
The date of the effort tolerance information used must be appropriate to the period of assessment: the effort tolerance information should be not more than six months older than the relevant time in the assessment period to which the information is to be applied.
Measurements of lung function
Spirometry should always be obtained if any condition affecting the function of the lungs is present unless it is not practicable or appropriate to perform spirometry because:
- the veteran is very old or frail and cannot reasonably attend a clinic where spirometry can be performed; or
- the veteran lives in a remote locality and cannot reasonably attend a clinic where spirometry can be performed; or
- the veteran’s impairment from other accepted conditions is of such a degree that it would result in a combined impairment rating of at least 68 points.
The date of the spirometry used must be appropriate to the period of assessment: the spirometry should be not more than six months older than the relevant time in the assessment period to which the information is to be applied.
The nature of the spirometry should be appropriate: the nature of the spirometric readings should be consistent with the known conditions affecting the veteran and should also be consistent with such other information (eg, old spirometry) as is available or can reasonably be obtained. There should be no unexplained inconsistencies between the various reports.
If the nature of the spirometry cannot be reconciled with other relevant information, the spirometry may need to be repeated or the veteran referred to a respiratory physician for clarification of the situation.
If a veteran has emphysema, as evidenced by diminished carbon monoxide diffusing capacity, and diagnosed by a specialist respiratory physician, assessment can be made on the basis of effort tolerance alone.
Step 3: Determine the impairment rating based on effort tolerance.
To determine the impairment rating based on effort tolerance follow the substeps below.
(Each step is elaborated in the following pages.)
Substep 3A | Determine the symptomatic activity level by applying Table1.1 — Activity Levels (with energy expenditure in METs). | Page 10 |
Substep 3B | Convert that symptomatic activity level into an impairment rating. This step involves consulting either Table 1.2 — Loss of Cardiorespiratory Function: Exercise Tolerance (Males); or Table 1.3 — Loss of Cardiorespiratory Function: Exercise Tolerance (Females). | Page 13 |
After both substeps have been completed, a single rating will have been obtained. This rating is known as the impairment rating for effort tolerance.
If symptoms do not occur, a rating for the condition may be found in Table 1.6 (Cardiac Failure) if applicable, or in the relevant Other Impairment table.
Substep 3A: Determine the symptomatic activity level.
The symptomatic activity level is the exercise level (measured in METs) at which symptoms occur. One MET represents the energy expenditure associated with the consumption of 3.5 mL oxygen per kilogram of body weight per minute. Table 1.1 lists various activities grouped according to their energy expenditure in METs.
The symptomatic activity level is the level at which the activities from within any one METs category consistently give rise to symptoms of the accepted cardiorespiratory condition, such as angina, dyspnoea, palpitations, or fatigue. The symptomatic activity level may be determined by reference to a report specifically provided for the purpose as well as by reference to clinical notes and by comparison of the information with the activities listed in Table 1.1. (The symptomatic activity level may be determined by reference to activities other than those contained in Table 1.1 if the energy expenditure (in METs) of those activities is available in the medical or scientific literature.)
In determining the symptomatic activity level, greater reliance is to be placed on activities that involve steady, as opposed to sporadic, expenditure of energy. Such activities are more reliable as indicators of exercise tolerance. Less reliance is to be placed on activities that can be completed in less than a few minutes, as symptoms may take longer than this to occur.
Responses of the type ‘I cannot do such and such’ or ‘I do not do so and so’ are not useful in assessing the symptomatic activity level. What must be established is that level of exercise that the veteran is able to do but which results in angina, breathlessness, or some other cardiorespiratory symptom.
Symptoms that occur while an activity is performed are not necessarily a result of the energy expenditure occasioned by the activity. Many specific activities can be performed in a way that would mean that they were no longer examples of the METs level in which they are placed in Table 1.1. For example, while driving a car sedately is an example of 2–3 METs, driving a car in a Grand Prix is not.
Estimations of exercise tolerance above the 6-7 METs level should only be made using exercise tests. The activities above the 6-7 METs level are listed for information only.
TABLE 1.1
CARDIORESPIRATORY IMPAIRMENT: ACTIVITY LEVELS
(with energy expenditure in METs)
1-2 METs | Energy expended at rest or minimal activity - Lying down.
- Sitting and drinking tea.
- Using sewing machine (electric).
- Sitting down.
- Sitting and talking on telephone.
- Travelling in car as passenger.
- Standing.
- Sitting and knitting.
- Playing cards.
- Strolling (slowly).
- Light sweeping.
- Clerical work (desk work only).
|
2–3 METs | Energy expanded in dressing, washing and performing light household duties - Light household duties.
- Walking slowly (3.5 km/h).
- Playing piano, violin, or organ.
- Typing.
- Cooking or preparing meals.
- Playing billiards.
- Clerical work which involves moving around.
- Setting table.
- Driving power boat.
- Washing dishes.
- Playing golf (with power buggy).
- Bench assembly work (seated).
- Dressing, showering.
- Horseback riding at walk.
- Using self-propelled mower.
- Light tidying, dusting.
- Lawn bowls.
- Polishing silver.
- Driving car.
|
3–4 METs | Energy expended in walking at an average pace - Walking at average walking pace (5 km/h).
- Golf (pulling buggy).
- Machine assembly.
- Cleaning car (excludes vigorous polishing).
- Minor car repairs.
- Tidying house.
- Welding.
- Cleaning windows.
- Table tennis.
- Pushing light power mower over flat suburban lawn at slow steady pace
- Vacuuming.
- Sedate cycling (10 km/h)
- Shifting chairs.
- Light gardening (weeding and water).
- Hanging out washing.
|
4–5 METs | Moderate activity: encompasses more strenuous daily activities with the exclusion of manual labour and vigorous exercise - Mopping floors.
- Golf (carrying bag).
- Light carpentry (eg, chiselling, hammering).
- Scrubbing floors.
- Ballroom dancing.
- Beating carpets.
- Tennis doubles (social, non-competitive).
- Stocking shelves with light objects.
- Polishing furniture.
- Wallpapering.
- Shopping and carrying groceries (10 kg).
- Gentle swimming.
- Painting outside of house.
- Hoeing (soft soil).
|
5–6 METs | Heavy exercise: manual labour or vigorous sports - Walking 6.5 km/h (sustained brisk walk, discomfort in talking at the same time).
- Walking slowly but steadily up stairs.
- Carpentry (eg. Sawing and planing with hand tools).
- Swimming laps (non-competitive).
- Pushing a full wheelbarrow (20 kg).
- Shovelling dirt (12 throws a minute).
|
6–7 METs | - Badminton (competitive)
- Tennis (singles, non-competitive).
- Water skiing.
- Loading truck with bricks.
- Using a pick and shovel to dig trenches.
|
7–8 METs | Very heavy exercise - Jogging (8 km/h).
- Horseback riding (galloping).
- Carrying heavy objects (30 kg) on level ground.
- Sawing hardwood with hand tools.
|
8–9 METs | - Running (9 km/h).
- Skiing (cross-country.
- Chopping hardwood.
- Callisthenics.
- Squash (non competitive).
|
10+ METs | - Running quickly (10 km/h).
- Cycling quickly (25 km/h).
- Carrying loads (10 kg) up a gradient.
- Football (any code).
|
The activities listed under each heading are examples. There will be other activities that have the same METs expenditure and hence can be used for reference if their METs level is known.
Alternate procedures for establishing the symptomatic activity level
1. The symptomatic activity level may be determined by exercise tests. These tests include:
use of treadmills; or
cycles; or
rowing machines.
Because of their greater objectivity, the results of exercise tests (when available) are to be used in preference to the method of calculating exercise tolerance as described above. Moreover, exercise tests must always be used to make an estimate of exercise tolerance above 6–7 METs.
2. If certain levels of activity have been prohibited by the treating doctor, because of the adverse effect the prohibited activity is likely to have on the veteran’s health as a result of the accepted condition, then the level of exercise that has been prohibited may be regarded as the symptomatic activity level.
Substep 3B: Convert the symptomatic activity level into an impairment rating.
The symptomatic activity level is used, in conjunction with the veteran’s age, height, and sex, to obtain an impairment rating.
In the case of a male, Table 1.2 is to be applied.
In the case of a female, Table 1.3 is to be applied.
For the purposes of Tables 1.2 and 1.3, a veteran’s age is taken to be his or her age in whole years at the date of the report relating to the exercise tolerance (unless the report is of a retrospective type and clearly refers to some earlier period, in which case the veteran’s age is taken to be his or her age in whole years at the relevant time).
Step 4: (Omit this step if no respiratory disease is present.) Determine the impairment rating based on measurements of lung function.
FEVl, FVC, and MEF 25–75 are the usual physiological measurements of lung function. Determinations of FEVl, FVC, and MEF 25–75 should be conducted by an experienced operator without specific administration of a bronchodilator. The best set of results should be selected, that is, the set of results which indicates the greatest degree of health and, consequently, the lowest degree of impairment.
If both pre-bronchodilator and post-bronchodilator results are available the pre-bronchodilator results are to be applied in determining the impairment rating based on measurements of lung function.
To determine the impairment rating based on measurements of lung function, follow the substeps below.
Substep 4A | Obtain the measured FEVl, FVC, and MEF 25–75 from the data. |
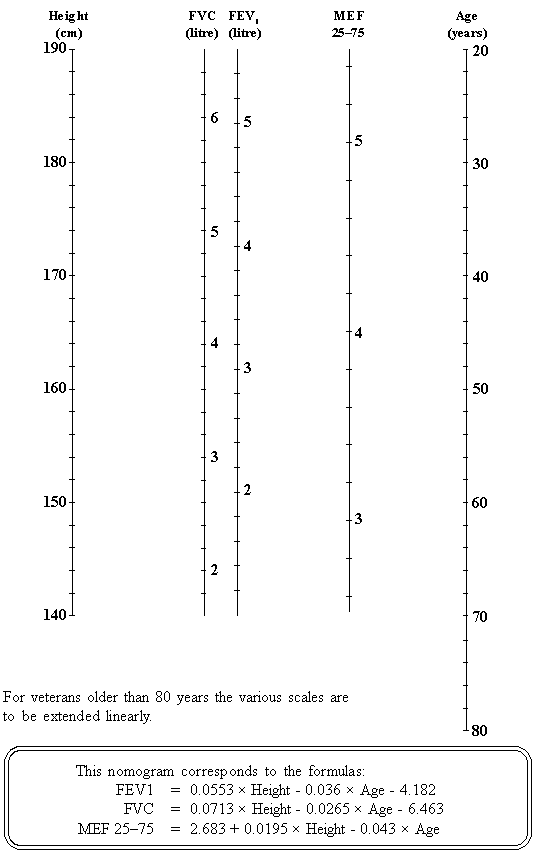
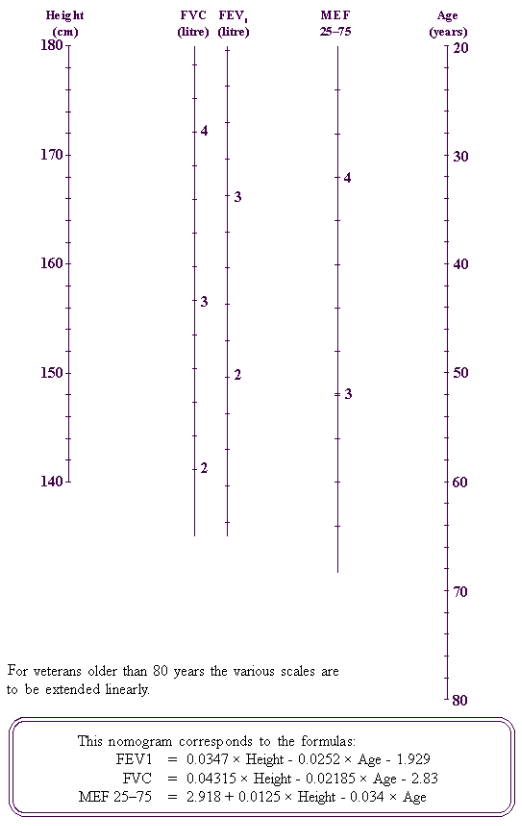
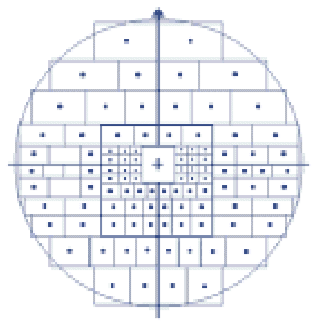
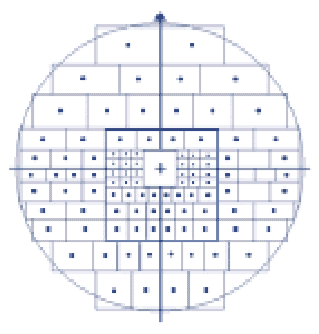
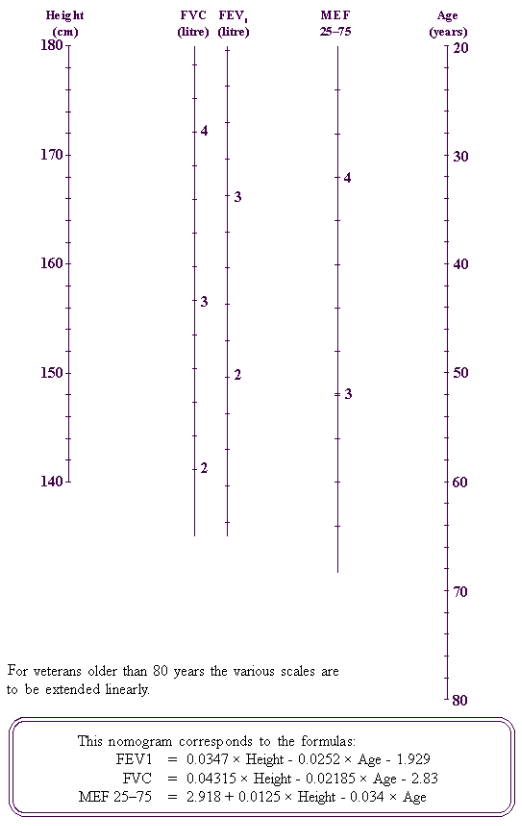
Substep 4B | Work out the predicted FEVl, FVC, and MEF 25–75 for a person of the same age, height, and gender. This can be done either by applying the nomograms Figure 1a (for males) or Figure 1b (for females) or by applying the formula relating to each nomogram. |
Substep 4C | Express the measured FEV1 as a percentage of the predicted FEV1, and Express the measured FVC as a percentage of the predicted FVC, and Express the measured MEF 25–75 (if appropriate) as a percentage of the predicted MEF 25–75. These conversions are performed by applying the formula: Measured value as % of predicted value = Actual value x 100 Predicted Value |
Substep 4D | Determine an impairment rating from a physiological measurement by using the percentage obtained in substep 4C in conjunction with Table 1.4. Separate impairment ratings can be obtained from each physiological measurement (that is, from the FEV1, FVC, and MEF 25–75). |
Substep 4E | The final impairment rating is the highest (or equal highest) of the ratings obtained in substep 4D. |
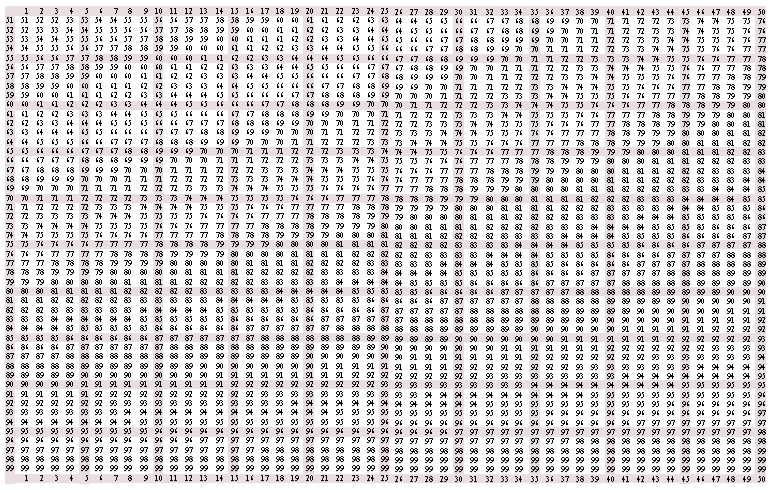
Function Loss Table 1.2 | 
|
LOSS OF CARDIORESPIRATORY FUNCTION: EXERCISE TOLERANCE | |
(Males) | |
Age | Symptomatic Activity Level | Age | Symptomatic Activity Level | |
| (METs*) | | (METs*) | |
less than 25 | 1–2 | 2–3 | 3–4 | 4–5 | 5–6 | 6–7 | 7–8 | 8–9 | 10+ | | 1–2 | 2–3 | 3–4 | 4–5 | 5–6 | 6–7 | 7–8 | 8–9 | 10+ | |
90 | 80 | 70 | 60 | 50 | 40 | 30 | 20 | 10 | 55 | 80 | 70 | 55 | 40 | 25 | 15 | 10 | | | |
25 | 90 | 80 | 70 | 60 | 50 | 40 | 30 | 20 | 10 | 56 | 80 | 70 | 54 | 39 | 24 | 15 | 9 | | | |
26 | 90 | 80 | 70 | 60 | 50 | 40 | 30 | 20 | 10 | 57 | 80 | 69 | 53 | 38 | 23 | 14 | 8 | | | |
27 | 89 | 80 | 70 | 59 | 48 | 38 | 28 | 19 | 10 | 58 | 80 | 69 | 52 | 37 | 22 | 14 | 7 | | | |
28 | 89 | 80 | 70 | 59 | 47 | 37 | 27 | 19 | 10 | 59 | 80 | 68 | 51 | 36 | 21 | 13 | 6 | | | |
29 | 88 | 80 | 70 | 58 | 46 | 36 | 26 | 18 | 10 | 60 | 80 | 68 | 50 | 35 | 20 | 13 | 5 | | | |
30 | 88 | 80 | 70 | 58 | 45 | 35 | 25 | 18 | 10 | 61 | 80 | 67 | 49 | 34 | 19 | 12 | 4 | | | |
31 | 87 | 80 | 70 | 57 | 44 | 34 | 24 | 17 | 10 | 62 | 80 | 67 | 48 | 33 | 18 | 12 | 3 | | | |
32 | 87 | 80 | 70 | 57 | 43 | 33 | 23 | 17 | 10 | 63 | 80 | 66 | 47 | 32 | 17 | 11 | 2 | | | |
33 | 86 | 80 | 70 | 56 | 42 | 32 | 22 | 16 | 10 | 64 | 80 | 66 | 46 | 31 | 16 | 11 | | | | |
34 | 86 | 80 | 70 | 56 | 41 | 31 | 21 | 16 | 10 | 65 | 80 | 65 | 45 | 30 | 15 | 10 | | | | |
35 | 85 | 80 | 70 | 55 | 40 | 30 | 20 | 15 | 10 | 66 | 80 | 64 | 44 | 29 | 15 | 9 | | | | |
36 | 85 | 80 | 70 | 55 | 39 | 29 | 20 | 15 | 9 | 67 | 79 | 63 | 43 | 28 | 14 | 8 | | | | |
37 | 85 | 79 | 69 | 54 | 38 | 28 | 19 | 14 | 8 | 68 | 79 | 62 | 42 | 27 | 14 | 7 | | | | |
38 | 85 | 79 | 69 | 54 | 37 | 27 | 19 | 14 | 7 | 69 | 78 | 61 | 41 | 26 | 13 | 6 | | | | |
39 | 85 | 78 | 68 | 53 | 36 | 26 | 18 | 13 | 6 | 70 | 78 | 60 | 40 | 25 | 13 | 5 | | | | |
40 | 85 | 78 | 68 | 53 | 35 | 25 | 18 | 13 | 5 | 71 | 77 | 59 | 39 | 24 | 12 | 4 | | | | |
41 | 85 | 77 | 67 | 52 | 34 | 24 | 17 | 12 | 4 | 72 | 77 | 58 | 38 | 23 | 12 | 3 | | | | |
42 | 85 | 77 | 67 | 52 | 33 | 23 | 17 | 12 | 3 | 73 | 76 | 57 | 37 | 22 | 11 | 2 | | | | |
43 | 85 | 76 | 66 | 51 | 32 | 22 | 16 | 11 | 2 | 74 | 76 | 56 | 36 | 21 | 11 | 1 | | | | |
44 | 85 | 76 | 66 | 51 | 31 | 21 | 16 | 11 | | 75 | 75 | 55 | 35 | 20 | 10 | | | | | |
45 | 85 | 75 | 65 | 50 | 30 | 20 | 15 | 10 | | 76 | 75 | 55 | 35 | 19 | 9 | | | | | |
46 | 85 | 75 | 64 | 49 | 30 | 20 | 15 | 9 | | 77 | 75 | 54 | 34 | 18 | 8 | | | | | |
47 | 84 | 74 | 63 | 48 | 29 | 19 | 14 | 8 | | 78 | 75 | 54 | 34 | 17 | 7 | | | | | |
48 | 84 | 74 | 62 | 47 | 29 | 19 | 14 | 7 | | 79 | 75 | 53 | 33 | 16 | 6 | | | | | |
49 | 83 | 73 | 61 | 46 | 28 | 18 | 13 | 6 | | 80 | 75 | 53 | 33 | 15 | 5 | | | | | |
50 | 83 | 73 | 60 | 45 | 28 | 18 | 13 | 5 | | 81 | 75 | 52 | 32 | 14 | 4 | | | | | |
51 | 82 | 72 | 59 | 44 | 27 | 17 | 12 | 4 | | 82 | 75 | 52 | 32 | 13 | 3 | | | | | |
52 | 82 | 72 | 58 | 43 | 27 | 17 | 12 | 3 | | 83 | 75 | 51 | 31 | 12 | 2 | | | | | |
53 | 81 | 71 | 57 | 42 | 26 | 16 | 11 | 2 | | 84 | 75 | 51 | 31 | 11 | 1 | | | | | |
54 | 81 | 71 | 56 | 41 | 26 | 16 | 11 | | | 85 | 75 | 50 | 30 | 10 | | | | | | |
| | | | | | | | | above 85 | 75 | 50 | 30 | 10 | | | | | | |
*One MET represents the energy expenditure associated with the consumption of 3.5 mL oxygen/kg body Weight/min. | |
| | | | | | | | | | | | | | | | | | | | | |
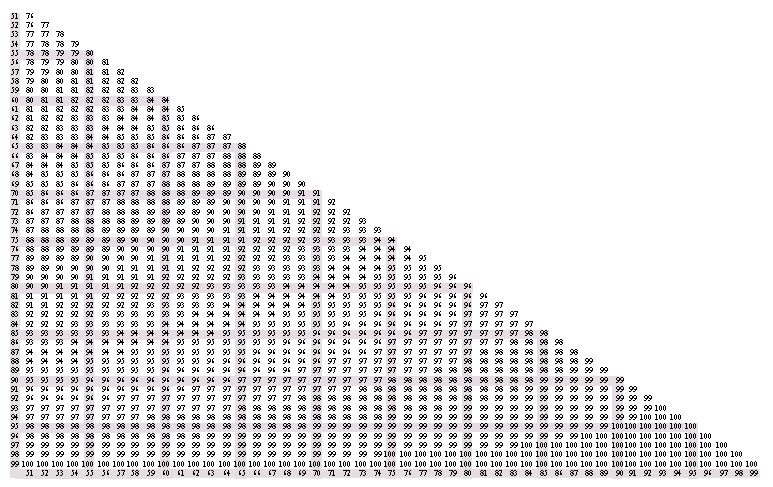
Functional Loss Table 1.3 | 
|
LOSS OF CARDIORESPIRATORY FUNCTION: EXERCISE TOLERANCE |
(Females) |
Age | Symptomatic Activity Level | Age | Symptomatic Activity Level |
| (METs*) | | (METs*) |
less than 25 | 1-2 | 2-3 | 3-4 | 4-5 | 5-6 | 6-7 | 7-8 | 8-9 | 10+ | | 1-2 | 2-3 | 3-4 | 4-5 | 5-6 | 6-7 | 7-8 | 8-9 | 10+ | |
90 | 80 | 70 | 55 | 40 | 30 | 20 | 15 | 10 | 55 | 80 | 65 | 50 | 30 | 20 | 15 | 10 | | | |
25 | 90 | 80 | 70 | 55 | 40 | 30 | 20 | 15 | 10 | 56 | 80 | 65 | 49 | 29 | 20 | 15 | 9 | | | |
26 | 90 | 80 | 69 | 54 | 40 | 30 | 20 | 15 | 10 | 57 | 80 | 64 | 48 | 28 | 19 | 14 | 8 | | | |
27 | 89 | 79 | 68 | 53 | 39 | 29 | 20 | 15 | 10 | 58 | 80 | 64 | 47 | 27 | 19 | 14 | 7 | | | |
28 | 89 | 79 | 67 | 52 | 39 | 29 | 20 | 15 | 10 | 59 | 80 | 63 | 46 | 26 | 18 | 13 | 6 | | | |
29 | 88 | 78 | 66 | 51 | 38 | 28 | 20 | 15 | 10 | 60 | 80 | 63 | 45 | 25 | 18 | 13 | 5 | | | |
30 | 88 | 78 | 65 | 50 | 38 | 28 | 20 | 15 | 10 | 61 | 80 | 62 | 44 | 24 | 17 | 12 | 4 | | | |
31 | 87 | 77 | 64 | 49 | 37 | 27 | 20 | 15 | 10 | 62 | 80 | 62 | 43 | 23 | 17 | 12 | 3 | | | |
32 | 87 | 77 | 63 | 48 | 37 | 27 | 20 | 15 | 10 | 63 | 80 | 61 | 42 | 22 | 16 | 11 | 2 | | | |
33 | 86 | 76 | 62 | 47 | 36 | 26 | 20 | 15 | 10 | 64 | 80 | 61 | 41 | 21 | 16 | 11 | | | | |
34 | 86 | 76 | 61 | 46 | 36 | 26 | 20 | 15 | 10 | 65 | 80 | 60 | 40 | 20 | 15 | 10 | | | | |
35 | 85 | 75 | 60 | 45 | 35 | 25 | 20 | 15 | 10 | 66 | 80 | 59 | 39 | 20 | 15 | 9 | | | | |
36 | 85 | 75 | 60 | 45 | 34 | 25 | 20 | 15 | 9 | 67 | 79 | 58 | 38 | 19 | 14 | 8 | | | | |
37 | 85 | 75 | 60 | 44 | 33 | 24 | 19 | 14 | 8 | 68 | 79 | 57 | 37 | 19 | 14 | 7 | | | | |
38 | 85 | 75 | 60 | 44 | 32 | 24 | 19 | 14 | 7 | 69 | 78 | 56 | 36 | 18 | 13 | 6 | | | | |
39 | 85 | 75 | 60 | 43 | 31 | 23 | 18 | 13 | 6 | 70 | 78 | 55 | 35 | 18 | 13 | 5 | | | | |
40 | 85 | 75 | 60 | 43 | 30 | 23 | 18 | 13 | 5 | 71 | 77 | 54 | 34 | 17 | 12 | 4 | | | | |
41 | 85 | 75 | 60 | 42 | 29 | 22 | 17 | 12 | 4 | 72 | 77 | 53 | 33 | 17 | 12 | 3 | | | | |
42 | 85 | 75 | 60 | 42 | 28 | 22 | 17 | 12 | 3 | 73 | 76 | 52 | 32 | 16 | 11 | 2 | | | | |
43 | 85 | 75 | 60 | 41 | 27 | 21 | 16 | 11 | 2 | 74 | 76 | 51 | 31 | 16 | 11 | 1 | | | | |
44 | 85 | 75 | 60 | 41 | 26 | 21 | 16 | 11 | | 75 | 75 | 50 | 30 | 15 | 10 | | | | | |
45 | 85 | 75 | 60 | 40 | 25 | 20 | 15 | 10 | | 76 | 75 | 49 | 29 | 15 | 9 | | | | | |
46 | 85 | 74 | 59 | 39 | 25 | 20 | 15 | 9 | | 77 | 75 | 48 | 28 | 14 | 8 | | | | | |
47 | 84 | 73 | 58 | 38 | 24 | 19 | 14 | 8 | | 78 | 75 | 47 | 27 | 14 | 7 | | | | | |
48 | 84 | 72 | 57 | 37 | 24 | 19 | 14 | 7 | | 79 | 75 | 46 | 26 | 13 | 6 | | | | | |
49 | 83 | 71 | 56 | 36 | 23 | 18 | 13 | 6 | | 80 | 75 | 45 | 25 | 13 | 5 | | | | | |
50 | 83 | 70 | 55 | 35 | 23 | 18 | 13 | 5 | | 81 | 75 | 44 | 24 | 12 | 4 | | | | | |
51 | 82 | 69 | 54 | 34 | 22 | 17 | 12 | 4 | | 82 | 75 | 43 | 23 | 12 | 3 | | | | | |
52 | 82 | 68 | 53 | 33 | 22 | 17 | 12 | 3 | | 83 | 75 | 42 | 22 | 11 | 2 | | | | | |
53 | 81 | 67 | 52 | 32 | 21 | 16 | 11 | 2 | | 84 | 75 | 41 | 21 | 11 | 1 | | | | | |
54 | 81 | 66 | 51 | 31 | 21 | 16 | 11 | | | 85 | 75 | 40 | 20 | 10 | | | | | | |
above 85 | 75 | 40 | 20 | 10 | | | | | | |
*One MET represents the energy expenditure associated with the consumption of 3.5mL oxygen/kg body weight/min. |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
FIGURE 1a ‑ PREDICTION NOMOGRAM: MALE (BTPS)
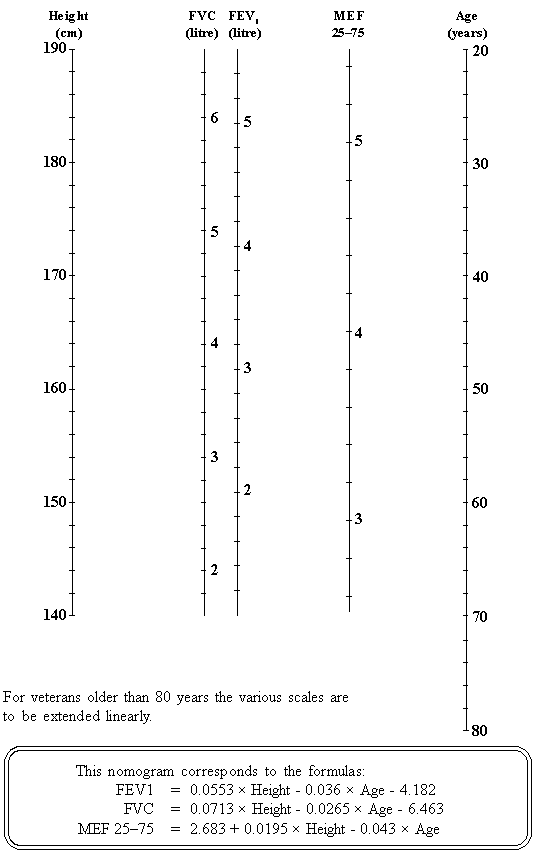
FIGURE 1b ‑ PREDICTION NOMOGRAM: FEMALE (BTPS)
Functional Loss Table 1.4 | 
|
LOSS OF CARDIORESPIRATORY FUNCTION: PHYSIOLOGICAL MEASUREMENTS |
Impairment Rating | FEV1 as a percentage of predicted | FVC as a percentage of predicted | MEF 25–75 as a percentage of predicted |
NIL | 85 | 85 | 85 |
TWO | | 84 | |
SIX | 84 | | 84 |
SEVEN | | 83 | |
EIGHT | 83 | | 83 |
TEN | 82 | | 82 |
ELEVEN | 81 | 82 | 81 |
TWELVE | | | |
THIRTEEN | 80 | | 80 |
FOURTEEN | 79 | 81 | 79 |
FIFTEEN | | | |
SIXTEEN | 78 | 80 | 78 |
SEVENTEEN | 77 | | 77 |
EIGHTEEN | 76 | 79 | 76 |
NINETEEN | | | |
TWENTY | 75 | 78 | 75 |
TWENTY-ONE | 74 | | 74 |
TWENTY-TWO | 73 | 77 | 73 |
TWENTY-THREE | 72 | | 72 |
TWENTY-FOUR | 71 | 76 | 71 |
TWENTY-FIVE | | | |
TWENTY-SIX | 70 | 75 | 70 |
TWENTY-SEVEN | 69 | 74 | 69 |
TWENTY-EIGHT | 68 | | 68 |
TWENTY-NINE | 67 | 73 | 67 |
THIRTY | 66 | 72 | 66 |
THIRTY-ONE | 65 | 71 | 65 |
THIRTY-TWO | 64 | | 64 |
THIRTY-THREE | 63 | 70 | 63 |
THIRTY-FOUR | 62 | 69 | 62 |
THIRTY-FIVE | 61 | 68 | 61 |
THIRTY-SIX | 60 | 67 | 60 |
THIRTY-SEVEN | 59 | | 59 |
| | | | |
Functional Loss Table 1.4 (continued) | 
|
LOSS OF CARDIORESPIRATORY FUNCTION: PHYSIOLOGICAL MEASUREMENTS |
Impairment Rating | FEV1 as a percentage of predicted | FVC as a percentage of predicted | MEF 25–75 as a percentage of predicted |
THIRTY-EIGHT | 58 | 66 | 58 |
THIRTY-NINE | 57 | 65 | 57 |
FORTY | | 64 | |
FORTY-ONE | 56 | 63 | 56 |
FORTY-TWO | 55 | 62 | 55 |
FORTY-THREE | 54 | 61 | 54 |
FORTY-FOUR | 53 | 60 | 53 |
FORTY-FIVE | 52 | | 52 |
FORTY-SIX | 51 | 59 | 51 |
FORTY-SEVEN | 50 | 58 | 50 |
FORTY-EIGHT | 49 | 57 | 49 |
FORTY-NINE | 48 | 56 | 48 |
FIFTY | 47 | 55 | 47 |
FIFTY-ONE | 46 | 54 | 46 |
FIFTY-TWO | 45 | 53 | 45 |
FIFTY-THREE | 44 | 52 | 44 |
FIFTY-FOUR | 43 | 51 | 43 |
FIFTY-FIVE | 42 | 50 | 42 |
FIFTY-SIX | 41 | 49 | 41 |
FIFTY-SEVEN | 40 | | 40 |
FIFTY-EIGHT | 39 | 48 | 39 |
FIFTY-NINE | 38 | 47 | 38 |
SIXTY | 37 | 46 | 37 |
SIXTY-ONE | 36 | 45 | 36 |
SIXTY-TWO | 35 | 44 | 35 |
SIXTY-THREE | 34 | 43 | 34 |
SIXTY-FOUR | 33 | 42 | 33 |
SIXTY-FIVE | 32 | 41 | 32 |
SIXTY-SIX | 31 | 40 | 31 |
SIXTY-SEVEN | 30 | 39 | 30 |
SIXTY-EIGHT | 29 | 38 | 29 |
SIXTY-NINE | 28 | 37 | 28 |
SEVENTY | 27 | 36 | 27 |
| | | | |
Impairment rating based on FEV1 | = | 98 - % FEV1 + | 50 (% FEV1-90) |
Impairment rating based on FVC | = | 108 - % FVC + | 100 (%FVC-88.5) |
Impairment rating based on MEF 25–75 | = | 98 - % MEF + | 50 (% MEF-90) |
When the measured parameter is 85% or more of the predicted, then the impairment rating is defined as NIL
“%FEV1” means measured FEV1 expressed as a percentage of predicted FEV1.
“%FVC” means measured FVC expressed as a percentage of predicted FVC. “%MEF” means measured MEF 25‑75 expressed as a percentage of predicted MEF 25–75.
In each case the percentage is to be rounded to the nearest integer before the formula is applied.
If these formulas are applied the resulting impairment rating is always to be rounded to the nearest integer.
Step 5: Calculate the total accepted cardiorespiratory functional impairment rating.
At this stage there will usually be an impairment rating derived from effort tolerance information and there may also be an impairment rating derived from measurements of lung function. These must be combined into a single cardiorespiratory functional impairment rating. The method by which that is to be done is set out in Table 1.5.
For the purposes of Table 1.5, the following abbreviations have been used:
Abbreviation | Meaning |
“FI” | means cardiorespiratory functional impairment rating. |
“No FI” | means a cardiorespiratory functional impairment rating cannot be calculated from either effort tolerance information or measurements of lung function. |
“METs” | means the cardiorespiratory functional impairment rating is to be taken as the impairment rating derived from METs alone. |
“Spirometry” | means the cardiorespiratory functional impairment rating is to be taken as the impairment rating derived from measurements of respiratory function. |
“average of METs and Spirometry” | means the average of the cardiorespiratory functional impairment rating derived from METs alone and the cardiorespiratory functional impairment rating derived from measurements of respiratory function alone — using the ordinary formula for averaging two quantities or by use of the nomogram in Figure 1c. In either case, the result is to be rounded to the nearest integer. |
Procedural Table 1.5 | 
|
CARDIORESPIRATORY FUNCTIONAL IMPAIRMENT |
| | Respiratory disease present | No respiratory disease |
| | Spirometry obtainable | Spirometry not obtainable | |
Cardiac disease present | METs data obtainable | FI = higher of METs and Spirometry | FI = METs | FI = METs |
METs data not obtainable | FI = Spirometry | No FI | No FI |
No cardiac disease | METs data obtainable | FI = average of METs and Spirometry | FI = METs | |
METs data not obtainable | FI = Spirometry | No FI | |
In applying this table, both accepted and non-accepted conditions are to be taken into account. |
| | | | | |
From Table 1.5 it will be seen that:
- if cardiac conditions exist in the absence of respiratory disease, cardiorespiratory functional impairment should be measured by effort tolerance alone;
- if respiratory conditions exist in the absence of cardiac disease, the cardiorespiratory functional impairment rating is the rounded average of (i) impairment as measured by effort tolerance, and (ii) impairment as measured by spirometry;
- if both cardiac and respiratory conditions co-exist, the cardiorespiratory functional impairment rating is the greater of (i) the impairment rating as measured by effort tolerance, and (ii) the impairment rating as measured by spirometry.
In applying these rules, both accepted and non-accepted cardiac and respiratory conditions are to be taken into account.
Only one rating for effort tolerance is to be given irrespective of the number of conditions that contribute to the relevant impairment.
Only one rating is to be given for physiological measurements of lung function irrespective of the number of conditions that contribute to the relevant impairment.
This single “total cardiorespiratory functional impairment” is due to the combined effect of all cardiorespiratory conditions whether accepted or not.
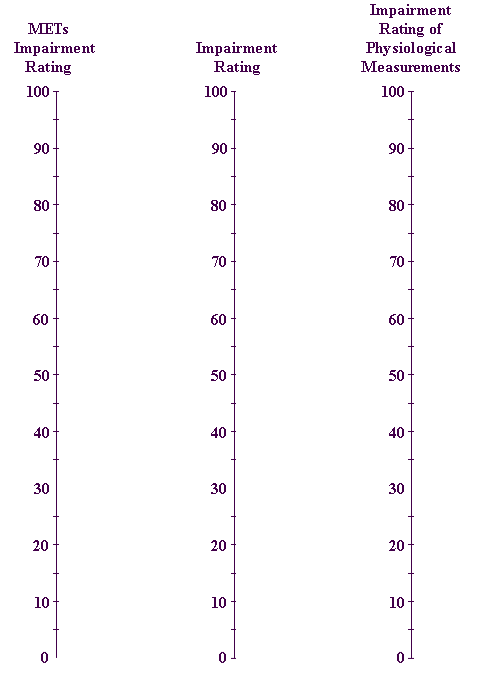
FIGURE 1c ‑ LOSS OF REPIRATORY FUNCTION RESPIRATORY NOMOGRAM
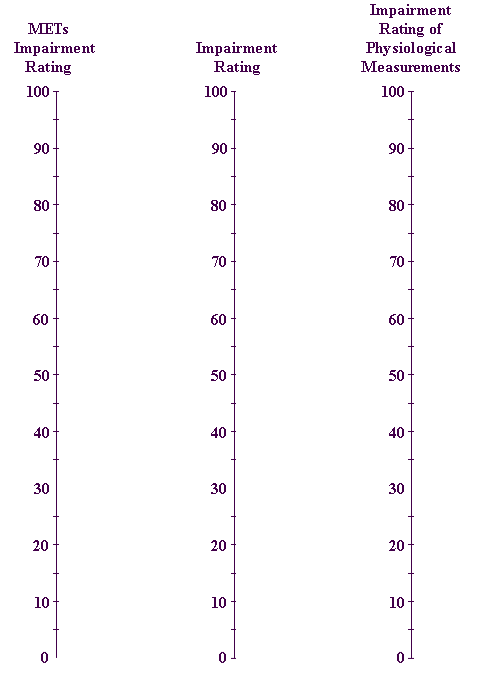
This nomogram is to be used in accordance with the instructions in Step 5 and the procedural Table 1.5.
Results from this nomogram are to be rounded to the nearest five points. 2.5 is to be rounded up to 5 and 7.5 is to be rounded up to 10.
This nomogram corresponds to the formula:
| METs Impairment Rating + Impairment Rating of Physiological Measurement 2 |
Step 6: Consider the effects of cardiac failure (if any).
For the purposes of assessment under this Guide, cardiac failure is considered to be a surrogate measure of cardiorespiratory impairment. When cardiac failure is present, the impairment rating calculated using effort tolerance will usually exceed any possible impairment rating from Table 1.6. Table 1.6 is of particular importance in assessing a veteran who is unable to be rated using effort tolerance because of significant conditions such as hemiplegia.
Functional Loss Table 1.6 | 
|
CARDIAC FAILURE |
Impairment Ratings | Criteria |
NIL | No cardiac failure; that is, neither symptoms nor X-ray evidence of cardiac failure. |
TEN | - No symptoms, but X-ray evidence of early cardiac failure.
- Evidence of right ventricular failure.
|
FIFTEEN | Left or biventricular cardiac failure demonstrated by ejection fraction of between 40% and 60% and persisting despite therapy. |
TWENTY | Left or biventricular cardiac failure demonstrated on X-ray or by ejection fraction of less than or equal to 40% and persisting despite therapy. |
Only one rating is to be selected from this table for any condition or combination of conditions. If more than one criterion applies, that which gives the higher or highest rating is to be chosen. |
| | |
A rating from Table 1.6 is to be compared with the total cardiorespiratory functional impairment rating (obtained in Step 5) and the higher of the two is to be chosen.
Step 7: Moderate the total cardiorespiratory functional impairment rating to allow for effects of any non-accepted conditions.
Partially contributing impairment
If non-accepted conditions contribute to the impairment, Chapter 19 (Partially Contributing Impairment) is to be applied to determine impairment from the accepted conditions.
If cardiac conditions exist in the absence of respiratory disease: if there is more than one cardiac condition present (for example ischaemic heart disease and a valvular heart disease) and some are accepted and some are not accepted, then the total cardiorespiratory functional impairment rating must be moderated by applying Chapter 19 to determine the impairment due to the accepted condition.
If a respiratory condition exists in the absence of cardiac disease, the symptomatic activity level will generally be the exercise level (in METs) at which dyspnoea occurs. If there is more than one respiratory condition present and at least one is accepted and at least one is not accepted, then the total cardiorespiratory functional impairment rating must be moderated by applying Chapter 19 to determine the impairment due to the accepted condition or conditions.
If cardiac and respiratory conditions co-exist, and at least one is accepted and at least one is not accepted, it is necessary to determine the total cardiorespiratory functional impairment rating (as set out in the previous steps), and then to moderate that rating by applying Chapter 19 to determine the impairment due to the accepted condition.
The result that is then derived is the “total accepted cardiorespiratory functional impairment rating”.
Step 8: Determine whether any ratings from the cardiorespiratory Other Impairment tables apply.
Cardiorespiratory Other Impairment tables
Once the total accepted cardiorespiratory functional impairment rating has been determined, it must be compared with the relevant cardiorespiratory Other Impairment tables. For assessment purposes, four categories of cardiorespiratory condition are recognised. These categories are:
- ischaemic heart disease;
- valvular heart disease;
- miscellaneous heart disease; and
- lower respiratory tract conditions.
There are four cardiorespiratory Other Impairment tables — corresponding to each of the above categories. These tables are:
Table 1.7 — Cardiorespiratory Impairment: Ischaemic;
Table 1.8 — Cardiorespiratory Impairment: Valvular;
Table 1.9 — Cardiorespiratory Impairment: Miscellaneous; and
Table 1.10 — Cardiorespiratory Impairment: Respiratory.
Only one rating is to be selected from each of these cardiorespiratory Other Impairment tables (Tables 1.7, 1.8, 1.9, and 1.10) for any condition or combination of conditions.
If accepted conditions belonging to more than one of the four categories of cardiorespiratory disease above are present, then the relative contribution of their effect on the total accepted cardiorespiratory functional impairment must be estimated by applying Chapter 20 (Apportionment). The rating for each condition will be the higher of the cardiorespiratory functional impairment rating attributed to it and its cardiorespiratory Other Impairment rating.
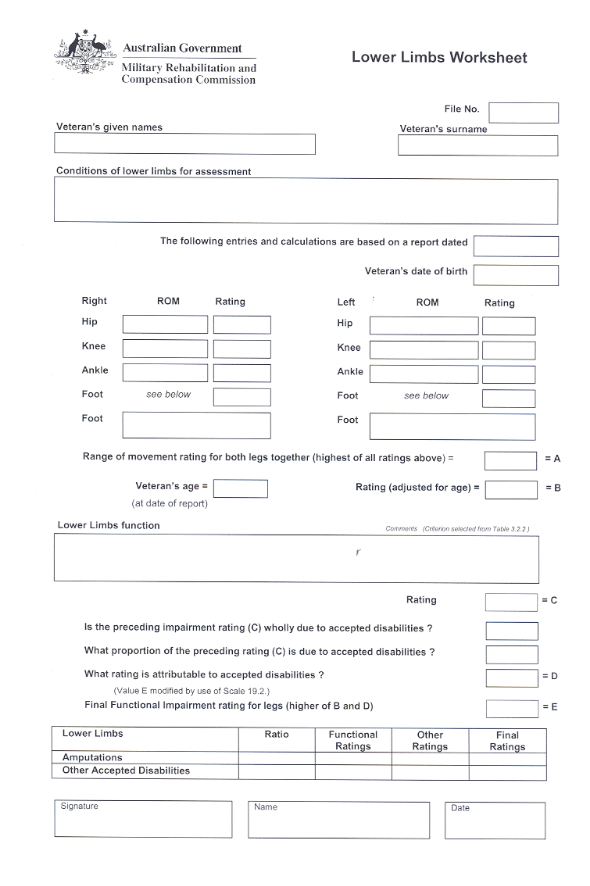
The cardiorespiratory worksheet (at page 29) should also be consulted.
Other Impairment Table 1.7 | 
|
CARDIORESPIRATORY IMPAIRMENT: ISCHAEMIC HEART DISEASE |
Impairment Ratings | Criteria |
NIL | No history of symptoms but evidence of transient ischaemia on exercise ECG testing. |
TEN | - Coronary artery disease, characterised by typical history of angina pectoris.
- Coronary artery disease, characterised by history of uncomplicated myocardial infarct, with no subsequent evidence of cardiac failure and infrequent or no angina.
- Coronary artery disease, with single vessel disease (other than left main coronary) demonstrated on angiogram.
- Coronary artery disease with successful coronary artery surgery, followed by no angina or only infrequent angina but no further infarcts or cardiac failure.
|
FIFTEEN | Coronary artery disease with multi-vessel disease (not successfully corrected) demonstrated on angiogram. |
TWENTY | - Coronary artery disease characterised by a history of myocardial infarct followed, immediately or after a lapse of time, by continuing angina or further infarcts.
- Coronary artery disease characterised by left main coronary artery disease (not successfully corrected) demonstrated on angiogram.
- Coronary artery disease with successful coronary artery surgery, followed, after a lapse of time, by frequent angina or further infarcts or cardiac failure.
|
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one criterion applies, that which gives the higher or highest rating is to be chosen. |
| | |
Other Impairment Table 1.8 | 
|
CARDIORESPIRATORY IMPAIRMENT: VALVULAR HEART DISEASE |
Impairment Ratings | Criteria |
NIL | - Mitral valve prolapse with no or minimal symptoms.
- Aortic sclerosis with no or minimal symptoms.
|
FIVE | Diagnosed valvular heart disease (other than mitral valve prolapse or aortic sclerosis) with no symptoms and no X-ray evidence of cardiac failure. |
TEN | Valvular heart disease with successful valve replacement, not requiring anticoagulant medication, with no subsequent symptoms or evidence of cardiac failure. |
FIFTEEN | Valvular heart disease with successful valve replacement, requiring anticoagulant medication, with no subsequent symptoms or evidence of cardiac failure. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one criterion applies, that which gives the higher or highest rating is to be chosen. |
| | |
Other Impairment Table 1.9 | 
|
CARDIORESPIRATORY IMPAIRMENT: MISCELLANEOUS |
Impairment Ratings | Criteria |
NIL | Flow murmurs. |
TWO | Chronic asymptomatic arrhythmia, eg. atrial fibrillation, atrial or ventricular ectopic beats. |
FIVE | Need for a permanent pacemaker. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one criterion applies, that which gives the higher or highest rating is to be chosen. |
| | |
Arrhythmias are usually to be rated by applying Chapter 15 (Intermittent Impairment) unless they cause a permanent restriction of exercise tolerance, in which case they are to be assessed by their effect on effort tolerance.
Other Impairment Table 1.10 | 
|
CARDIORESPIRATORY IMPAIRMENT: LOWER RESPIRATORY TRACT |
Impairment Ratings | Criteria |
NIL | Asymptomatic pleural plaques |
TWO | - Recurrent lower respiratory infections (at least 6 per year)
- Intermittent use of bronchodilator medication.
|
FIVE | - Daily use of inhaled steroids required.
- Regular, daily use of bronchodilator medication.
- Chronic cough, with production of at least 50mL sputum/day.
|
TEN | - Regular, daily use of bronchodilator medication required in addition to daily inhaled steroids.
- Chronic cough, with production of at least 100 mL sputum/day.
|
TWENTY | Repeated courses (at least several courses per year) or permanent use of oral steroids required. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one criterion applies, that which gives the higher or highest rating is to be chosen. |
| | |
Peripheral Vascular Conditions
Tables 1.2 and 1.3 are to be applied to assess those conditions that affect exercise tolerance from a cardiorespiratory point of view. Peripheral vascular conditions typically cause loss of function of the lower limbs only and therefore are to be assessed under lower limb impairment (using Chapter 3).
Atherosclerosis frequently causes both a cardiorespiratory condition and a peripheral vascular condition. In such cases, if both types of conditions are accepted conditions, then both conditions are to be rated using the appropriate assessment procedure.
The rating of asthma depends on the clinical circumstances. If asthma has caused chronic airways obstruction the method of assessment described in this chapter is to be applied. If there is little fixed obstruction and a large reversible component, the rating is to be based on the occurrence of attacks using the method of intermittent impairment (Chapter 15). Asthma can also be rated, if there is minimal loss of function, from Table 1.10.

CHAPTER 2
HYPERTENSION AND NON-CARDIAC VASCULAR CONDITIONS
This Chapter contains three parts:
Part 2.1 — Hypertension
Part 2.2 — Vascular Conditions of the Lower Limbs
Part 2.3 — Other Non-Cardiac Vascular Conditions
INTRODUCTION
This chapter is to be applied in determining impairment ratings for hypertension and non-cardiac vascular conditions. For conditions affecting the heart itself refer to Chapter 1 (Cardiorespiratory Impairment).
Hypertension, of itself, does not affect effort tolerance. Therefore, uncomplicated hypertension is not to be assessed under Chapter 1 (Cardiorespiratory Impairment) but in the manner set out below.
Calculation of the impairment rating for hypertension
Follow the steps below to calculate the impairment rating for hypertension.
STEP 1 | Establish whether any target organ damage is present. | Page 30 |
STEP 2 | (Omit this step if there is no target organ damage.) Calculate the total functional impairment for any accepted target organ damage | Page 31 |
STEP 3 | Calculate the Other Impairment rating for the accepted hypertension by applying Table 2.1.1. | Page 32 |
STEP 4 | (Omit this step if there is no target organ damage.) Compare the rating obtained in Step 2 with the rating obtained in Step 3. Take the higher of these two ratings | Page 32 |
Step 1: Establish whether any target organ damage is present.
For the purposes of this chapter, “target organ damage” means any of the following:
- hypertensive retinopathy, grade III or IV;
- hypertensive cardiac disease, with ECG or X-ray evidence of left ventricular hypertrophy;
- hypertensive nephropathy demonstrated at biopsy, or by presence of proteinuria or elevated serum creatinine level; or
- hypertensive cerebral haemorrhage.
Certain other conditions have hypertension as a contributing factor in their aetiology (for example: ischaemic heart disease and peripheral vascular disease). Such conditions are not to be regarded as being target organ damage when applying Part 2.1.
Step 2: Calculate the total functional impairment due to any accepted target organ damage.
Accepted hypertensive retinopathy is to be assessed by applying Chapter 8.
If other ophthalmic conditions are present, they must be allowed for by applying Chapter 20 (Apportionment) or Chapter 19 (Partially Contributing Impairment) as appropriate.
Accepted hypertensive cardiac disease is to be assessed by applying Chapter 1.
If other cardiorespiratory conditions are present, they must be allowed for by applying Chapter 20 (Apportionment) or Chapter 19 (Partially Contributing Impairment) as appropriate.
Accepted hypertensive nephropathy is to be assessed by applying Chapter 9.
If other renal conditions are present, they must be allowed for by applying Chapter 20 (Apportionment) or Chapter 19 (Partially Contributing Impairment) as appropriate.
Accepted hypertensive cerebral haemorrhage is to be assessed according to the specific effects of the haemorrhage.
The impairment ratings attributable to the accepted target organ damage are to be combined by applying Chapter 18 (Combined Values Chart) to obtain the total impairment rating for accepted target organ damage.
Target organ damage that is not an accepted condition cannot be assessed under this Guide. Target organ damage can be assessed under this Guide only after it has been claimed and has become an accepted condition.
The criterion in Table 2.1.1 which refers to “hypertension of such a degree that target organ damage is present” is not an assessment of the target organ damage itself but is a measure of the severity of the hypertension.
Step 3: Determine an impairment rating for hypertension from Table 2.1.1.
Other Impairment Table 2.1.1 | 
|
HYPERTENSION |
Impairment Ratings | Criteria |
NIL | Hypertension adequately controlled by diet and weight loss without long-term medication. |
TWO | Hypertension requiring long-term medication but without side-effects of the medication and with no evidence of target organ damage. |
FIVE | - Hypertension with diastolic pressure consistently at or greater than 90 mm Hg despite treatment.
- Hypertension: controlled but frequent minor side effects of medication which cause no loss of function.
|
TEN | - Hypertension: diastolic pressure consistently greater than 100 mm Hg.
- Hypertension of such a degree that target organ damage is present.
- Hypertension: controlled but with side effects of medication causing a significant and persistent loss of function.
|
| Only one rating is to be selected from this table. |
| | |
For the purpose of determining a rating of 10 impairment points from Table 2.1.1 (dot point 2) target organ damage has to be present either as an accepted condition or as a non-accepted condition.
Step 4: (Omit this step if is there is no target organ damage.) Compare the rating obtained in Step 2 with the rating obtained in Step 3. Take the higher rating.
The total impairment rating for accepted target organ damage is to be compared with any applicable rating from Table 2.1.1, and the higher of the two is to be taken as the impairment rating for the accepted hypertension.
Substep 4A | If the impairment rating from Table 2.1.1 is higher than the total rating for accepted target organ damage, the latter rating is to be discarded and its components are not to be used in any further calculations. |
Substep 4B | If the impairment rating for accepted target organ damage is higher than the rating from Table 2.1.1, the rating from Table 2.1.1 is to be discarded and each of the components of the rating for accepted target organ damage is to be included in the final combining of all impairment ratings. |
Impairment ratings from Table 2.1.1 are not routinely compared with ratings from the functional loss tables in Chapter 1 (Cardiorespiratory Impairment) except if hypertensive cardiomyopathy is present. Instead, they are to be compared with the impairment rating for the total loss of function due to target organ damage.
The total impairment rating for target organ damage is not to be combined with the impairment rating obtained from Table 2.1.1.
PART 2.2: VASCULAR CONDITIONS OF THE LOWER LIMBS
Each vascular condition of the lower limbs is characterised as belonging to one or more of three categories. These categories are:
- (arterial) peripheral vascular disease;
- varicose veins and vascular leg ulcers; and
- oedema.
Each category is to be assessed by applying a specific table from this part of the Guide. Depending on their effects, vascular conditions of the lower limbs may be rated under one or more of these tables.
Determination of the impairment rating for vascular conditions of the lower limbs
Follow the steps below to determine the impairment rating for each type of accepted vascular condition of the lower limbs.
(Each step is elaborated in the following pages.)
Step 1 | Establish whether any effect on lower limb function is present. | Page 34 |
Step 2 | Establish whether any effect on the skin is present. | Page 34 |
Step 3 | (Omit this step if there is no effect on lower limb function) Determine the impairment rating for the effects on lower limb function. | Page 34 |
Step 4 | (Omit this step if there is no effect on skin) Determine the impairment rating for the effects on the skin. | Page 34 |
Step 5 | Determine the Other Impairment rating for the vascular conditions of the lower limbs by applying Tables 2.2.1, 2.2.2, and 2.2.3. | Page 34 |
Step 6 | Combine the impairment ratings obtained in Steps 3 and 4. | Page 36 |
Step 7 | Combine the impairment ratings obtained in Step 5. | Page 36 |
Step 8 | Compare the impairment ratings obtained in Steps 6 and 7. | Page 36 |
Step 9 | If the comparison made in Step 8 shows that the impairment rating obtained in Step 6 is greater than the impairment rating obtained in Step 7, then the ratings obtained in Steps 3 and 4 are the final impairment ratings for the vascular condition. | Page 36 |
Step 10 | If the comparison made in Step 8 shows that the impairment rating obtained in Step 7 is greater than the impairment rating obtained in Step 6, then the separate ratings that have been combined in Step 5 are the final impairment rating(s) for the vascular condition. | Page 37 |
Step 1: Establish whether any effect on lower limb function is present.
Lower limb function may be affected by peripheral vascular disease. If peripheral vascular disease is present, the veteran’s walking distance is likely to be reduced as a result of intermittent claudication (cramplike pain in the calves of the legs).
Step 2: Establish whether any effect on the skin is present.
Varicose veins can affect the skin of the lower limbs. They may cause discolouration or pruritus (itching). Excoriations (scratch marks) may be present.
Step 3: (Omit this step if there is no effect on lower limb function.) Determine the impairment rating for the effects on lower limb function.
Lower Limb Function is to be assessed by applying Chapter 3 (Impairment of Spine And Limbs) — Part 3.2. If other conditions affecting lower limb function are present, they must be allowed for by applying Chapter 20 (Apportionment) or Chapter 19 (Partially Contributing Impairment) as appropriate.
The effects of vascular conditions of the lower limbs on lower limb function are taken to be symptoms or manifestations of the condition. Hence, they are to be assessed as part of the vascular condition of the lower limbs.
Step 4: (Omit this step if there is no effect on the skin.) Determine the impairment rating for the effects on the skin.
Skin conditions are to be assessed by applying Chapter 11 (Skin Impairment). If other conditions affecting the skin are present, they must be allowed for by applying Chapter 20 (Apportionment) or Chapter 19 (Partially Contributing Impairment) as appropriate.
The effects of vascular conditions of the lower limbs on the skin of the lower limbs are taken to be symptoms or manifestations of the condition. Hence, they are to be assessed as part of the vascular condition of the lower limb.
Step 5: Determine the Other Impairment rating for the vascular conditions of the lower limbs by applying Tables 2.2.1, 2.2.2, and 2.2.3.
There are three Other Impairment tables relating to the effects of vascular conditions of the lower limbs. A condition may be rated under more than one table if appropriate. However, only one rating may be taken from each table irrespective of how many conditions contribute to the type of impairment to which that table relates.
The three Other Impairment tables are:
Table 2.2.1 — (Arterial) Peripheral Vascular Disease
Table 2.2.2 — Varicose Veins
Table 2.2.3 — Oedema.
Amputations arising from peripheral vascular disease cannot be assessed unless they have been separately accepted. They can then be assessed under Chapter 3 (Impairment of Spine and Limbs).
Other Impairment Table 2.2.1 | 
|
(ARTERIAL) PERIPHERAL VASCULAR DISEASE |
Impairment Ratings | Criteria |
NIL | No peripheral vascular disease is present. |
TWO | Minor peripheral vascular disease or peripheral vascular disease that has been successfully treated. |
FIVE | Moderate peripheral vascular disease is present but causes little restriction of activities. |
TEN | Severe peripheral vascular disease, the expected effects of which are masked by a non-accepted condition (eg, masked by restriction on walking due to a musculoskeletal disorder). |
| Irrespective of whether one or two legs are affected, only one rating may be selected from this table. |
| | |
Other Impairment Table 2.2.2 | 
|
VARICOSE VEINS |
Impairment Ratings | Criteria |
NIL | - Varicose veins which are not greatly disfiguring, which cause only trivial symptoms, and which impose no significant restriction on activities.
- Superficial, small or transient ulceration.
|
TWO | Varicose veins which are unsightly or even gross but which impose no significant restriction on activities. |
FIVE | Varicose veins, varicose ulcers — causing constant or almost constant symptoms which are not easily tolerated and require medication or therapy. |
TEN | Very severe varicose veins or ulceration — difficult to control and requiring periodic confinement or hospital admissions. |
| Irrespective of whether one or two legs are affected, only one rating may be selected from this table. |
| | |
Other Impairment Table 2.2.3 | 
|
OEDEMA |
Impairment Ratings | Criteria |
NIL | Mild or transient oedema. |
FIVE | Moderate and persistent oedema. |
TEN | Marked oedema, that is only partly controlled by treatment or therapy. |
| Irrespective of whether one or two legs are affected, only one rating may be selected from this table. |
| | |
An impairment rating from this table may be given in addition to an impairment rating from Chapter 1 even when both arise from the same condition (eg, heart failure).
Step 6: Combine the impairment ratings obtained in Steps 3 and 4.
If ratings were obtained both in Step 3 and in Step 4, then the ratings are to be combined. This combining is for the purpose of the comparison to be made in Step 8. If only one rating has been given in Steps 3 and 4, then the result to be obtained in Step 6 is to be the same as the one rating given in either Step 3 or Step 4.
Step 7: Combine the impairment ratings obtained in Step 5.
If more than one rating has been given in Step 5 then the ratings are to be combined. This combining is for the purpose of the comparison to be made in Step 8. If only one rating has been given in Step 5, then the result to be obtained in Step 7 is to be the same as the result obtained in Step 5.
Step 8: Compare the impairment ratings obtained in Steps 6 and 7.
Step 9: If the comparison made in Step 8 shows that the impairment rating obtained in Step 6 is higher than the impairment rating obtained in Step 7, then the ratings obtained in Steps 3 and 4 are the final impairment ratings for the vascular condition.
If more than one rating was obtained in Steps 3 and 4 those ratings are not to be combined at this stage, but each is to be included in the final combining of all ratings.
Step 10: If the comparison made in Step 8 shows that the impairment rating obtained in Step 7 is higher than the impairment rating obtained in Step 6, then the rating(s) obtained in Step 5 are the final impairment rating(s) for the vascular condition.
If more than one rating was obtained in Step 5 those ratings are not to be combined at this stage, but each is to be included in the final combining of all ratings.
PART 2.3: OTHER NON-CARDIAC VASCULAR CONDITIONS
This Part is to be applied for a variety of vascular conditions not covered elsewhere in the Guide.
Other Impairment Table 2.3.1 | 
|
ANEURYSMS AND INTRA-VASCULAR CONDITIONS |
Impairment Ratings | Criteria |
NIL | No aneurysms or intra-vascular conditions present. |
TWO | - Aortic aneurysm of diameter less than 6 cm.
- Renal artery stenosis.
- Iliac or femoral or carotid aneurysms.
|
FIVE | - Embolus requiring anticoagulant medication.
- Non-valvular vascular conditions requiring anti-coagulant medication.
- Aortic aneurysm of 6 cm diameter or more.
- Aortic aneurysm surgically corrected.
|
TEN | Other vascular conditions (eg. severe deep venous thrombosis) that are difficult to control. |
| The impairment from any single condition can only receive one rating from this table. If the impairment from a given condition (eg, an aortic aneurysm) satisfies more than one criterion, it is to be given only the highest applicable rating. |
| | |
Aneurysms, atherosclerosis, and cerebrovascular disease
Impairment from atherosclerosis is to be rated by applying the appropriate tables in Chapter 1, Part 2.2 of Chapter 2, and Chapter 5 (Neurological Impairment) according to the losses of function or other impairments which it causes.
Impairment from cerebral aneurysms and cerebrovascular disease is to be rated by applying Chapter 5 (Neurological Impairment) and any other applicable chapter, according to the other effects of the cerebrovascular disease.
CHAPTER 3
IMPAIRMENT OF SPINE AND LIMBS
This chapter contains six parts:
Part 3.1 — Upper Limbs
Part 3.2 — Lower Limbs
Part 3.3 — Spine
Part 3.4 — Resting Joint Pain
Part 3.5 — Ranges of Joint Movement
Part 3.6 — Spine and Limbs Age Adjustment
INTRODUCTION
This chapter is used to assess the motor function of the spine and limbs. Sensory loss is to be assessed under Chapter 5 (Neurological Impairment).
Impairment of limbs
When a previously-accepted condition is later removed by an amputation that is also an accepted condition, the rating is to be based on the amputation or the resulting functional deficit, whichever results in the higher impairment rating. The previously accepted condition is not to be given an impairment rating.
Functional impairment is to be calculated separately for each upper limb. Thus one functional impairment rating may be calculated for the right upper limb and another for the left upper limb.
Calculation of the impairment rating for conditions of each upper limb
Follow the steps below to calculate the impairment rating for accepted conditions of each upper limb:
(Steps 2–8 are elaborated in the following pages.)
STEP 1 | If accepted condition(s) affect only the right upper limb, follow steps 2–8. If accepted condition(s) affect only the left upper limb, follow steps 2–8 substituting “left” for “right” in the instructions. If accepted condition(s) affect both upper limbs, follow steps 2–8 to assess the right upper limb, and then, to assess the left upper limb, repeat steps 2–8 substituting “left” for “right” in the instructions. | |
STEP 2 | Establish which joints in the right upper limb, if any, have some restriction of movement as a result of accepted conditions affecting the right upper limb. | Page 40 |
STEP 3 | (Omit this step if is there is no restriction of joint movement in the right upper limb.) Calculate the functional impairment due to restriction of range of movement of joints in the right upper limb as a result of accepted conditions of the right upper limb. | Page 41 |
STEP 4 | Calculate the functional impairment rating for the right upper limb as a whole using Table 3.1.2. | Page 43 |
STEP 5 | Compare the functional impairment rating for the right upper limb as a whole with the functional impairment rating from any restricted range of movement. Take the higher of these two as the final functional impairment rating for the right upper limb. | Page 43 |
STEP 6 | Make any applicable age adjustment to the final functional impairment rating for the right upper limb by applying Table 3.6.1 in Part 3.6 of this chapter. | Page 43 |
STEP 7 | Determine if any Other Impairment rating applies to the right upper limb. | Page 44 |
STEP 8 | (Omit this step if no Other Impairment rating applies to the right upper limb.) Compare the final functional impairment rating for the right upper limb with any Other Impairment rating applicable to the right upper limb. Take the higher of these ratings. | Page 45 |
Step 2: Establish which joints in the right upper limb have some restriction of movement as a result of accepted conditions of the right upper limb.
For the purposes of assessment under the Guide, the major joints of the upper limb are the shoulder, the elbow and the wrist.
In addition, the joints of the thumb and fingers are also to be considered. However, only one rating is to be given for the total effect of restrictions in all joints of the thumb and fingers considered together.
Conditions such as painful arc syndrome and fractured neck of radius may affect the range of movement (ROM) of the shoulder. A condition such as fractured scaphoid will be likely to affect the ROM of the wrist. In cases of fractures, the ranges of movements of the joints proximal to and distal to the fracture site should generally be considered as joints the ROM of which may be affected.
Hence, it must be determined which, if any, of
- shoulder;
- elbow;
- wrist; and
- thumb and fingers,
potentially have loss of range of movement due to accepted conditions.
Certain vascular conditions or neurological conditions of the upper limb, such as muscle weakness, tremor, apraxia, and loss of co-ordination, may have an effect on the function of the upper limb without restricting the range of movement of any joint of the limb. The assessment of such conditions is to be made under Step 4 of this Part.
Step 3: Calculate the functional impairment due to restriction of range of movement of joints in the right upper limb as a result of accepted conditions of the right upper limb.
Single functional impairment ratings may be obtained for each of the following four joints or sets of joints based on restriction of range of movement due to accepted conditions:
- shoulder;
- elbow;
- wrist; and
- thumb and fingers.
These impairment ratings are to be obtained by applying Table 3.1.1. Such functional impairment ratings are referred to as the functional impairment rating of the upper limb based on restriction of range of movement of the shoulder, elbow, wrist, or thumb and fingers respectively.
The loss of range of movement is to be estimated to the nearest quarter of the normal range of movement.
The range of movement relevant to assessment under this Guide is the active range of movement of the joint, that is the range through which the veteran can move the joint by virtue only of those muscles whose normal function it is to do so. The ability of a veteran to flex a joint by use of other, non-affected body parts does not reduce the rating which the impaired joint attracts. (For example, if a veteran cannot flex the right elbow in the normal fashion, by use of the right biceps, but can use the left hand to bend the right elbow, the right elbow should be assessed as having “loss of almost all movement”.)
The loss of range of movement will usually be provided as a fractional loss of range of movement and such data can be related directly to items within Table 3.1.1. However, sometimes, the measured movements of an affected joint will be available in degrees. In such a case the measured movement must be compared with the average range of movement of a normal joint to obtain the fractional loss of range of movement.
The average ranges of movement of various normal joints of the upper limb may be obtained from Table 3.5.1 in Part 3.5. These values are to be used in arriving at the fractional loss of range of movement when the actual movements of a joint are known in degrees.
If non-accepted conditions contribute to the loss of range of movement, Chapter 19 (Partially Contributing Impairment) is to be applied in conjunction with Table 3.1.1.
For the purposes of this chapter: |
“position of function” means the position that interferes least with the total function of the limb or the spine; and |
“unfavourable position” means a position that is significantly different from the position of function; and |
“flail joint” means a joint that is completely unstable in all directions. |
Functional Loss Table 3.1.1 | 
| |
LOSS OF MUSCULOSKELETAL FUNCTION: UPPER LIMB JOINTS | |
| Impairment Ratings | Shoulder | Elbow | Wrist | Thumb and Fingers |
| NIL | - No abnormality.
- X-ray changes only with normal range of movement.
| - No abnormality.
- X-ray changes only with normal range of movement.
| - No abnormality.
- X-ray changes only with normal range of movement.
| - No abnormality.
- X-ray changes only with normal range of movement.
|
| FIVE | | | Loss of about one-quarter normal range of movement. | - Ankylosis in any position of joints of 4th or 5th finger.
- Ankylosis in any position of function of any joints of 2nd or 3rd finger.
|
| TEN | Loss of about one-quarter normal range of movement. | Loss of about one-quarter normal range of movement. | Loss of about one-half normal range of movement. | - Ankylosis in an unfavourable position of any or all joints of 2nd and 3rd finger.
- Thumb: loss of almost all movement or complete ankylosis of any or all joints (in position of function).
|
| FIFTEEN | | | Loss of about three-quarters normal range of movement. | Thumb: ankylosis of any or all joints in an unfavourable position. |
| TWENTY | Loss of about one-half normal range of movement. | Loss of about one-half normal range of movement. | Loss of almost all movement, or complete ankylosis in position of function. | |
| THIRTY | Loss of about three-quarters normal range of movement. | Loss of about three-quarters normal range of movement. | Ankylosis in an unfavourable position, or a flail joint. | |
| FORTY | Loss of almost all movement, or complete ankylosis in position of function. | Loss of almost all movement, or complete ankylosis in position of function. | | |
| FIFTY | Ankylosis in an unfavourable position, or a flail joint. | Ankylosis in an unfavourable position, or a flail joint. | | |
| | Only one rating is to be selected from this table fro each shoulder, elbow, or wrist; and only one rating is to be selected from this table for the thumb and fingers together. Of these ratings only the highest is to be taken for each side. |
| | | | | | | |
Step 4: Calculate the functional impairment rating for the right upper limb as a whole using Table 3.1.2.
Table 3.1.2 measures the loss of function relating to the upper limb as a whole. Only one rating is to be given from this table, for the right upper limb, for any condition or combination of conditions. To attract a particular rating, the degree of impairment must be greater than that described at all lower levels.
Table 3.1.2 is the only relevant table if the use of an upper limb is restricted by vascular conditions or neurological conditions, such as muscle weakness, tremor, apraxia, loss of co-ordination, fatigue or pain, and when no condition affecting the range of movement of a joint is present.
If non-accepted conditions contribute to the loss of function, Chapter 19 (Partially Contributing Impairment) is to be applied in conjunction with Table 3.1.2.
Step 5: Compare the impairment rating for loss of function of the right upper limb with the impairment rating from any restricted range of movement. Take the higher of these two as the final functional impairment rating for the right upper limb.
After the application of Chapter 19 (Partially Contributing Impairment) in Step 3, the functional impairment rating from loss of range of movement is to be compared with the functional impairment for the use of the limb as whole.
The higher of these two ratings is then taken as the final functional impairment rating for the right upper limb.
Step 6: Make any applicable age adjustment to the final functional impairment rating for the right upper limb by applying Table 3.6.1 in Part 3.6 of this chapter.
The functional impairment rating obtained in Step 4 is to be age adjusted by applying Table 3.6.1.
Total loss of function of each upper limb is considered to be 60 per cent impairment of the whole person. Amputation of an arm at the shoulder joint, or total loss of use of an arm is equivalent to 60 impairment points.
With the exception of a forequarter amputation, no condition or combination of conditions affecting an arm shall receive an impairment rating exceeding 60 points.
In the case of a veteran aged 45 years or less, if the application of age adjustment to the functional impairment rating of an accepted condition affecting the right upper limb results in an impairment rating higher than 60 impairment points, the functional impairment rating for the right upper limb is to be taken as 60 impairment points and not at the higher rating obtained by applying Table 3.6.1.
Functional Loss Table 3.1.2 | 
|
LOSS OF MUSCULOSKELETAL FUNCTION: (BASED ON USE OF LIMB AS A WHOLE) |
Impairment Ratings | Criteria |
NIL | Can use limb efficiently for normal tasks and without undue fatigue. |
TWO | Can use limb efficiently for normal tasks but with excessive fatigue towards the end of the day. |
FIVE | Can use limb efficiently for normal tasks without excessive fatigue for no more than half an hour. |
TEN | - Can use limb reasonably well in most circumstances, but frequent difficulties are manifested by:
- minor loss of digital dexterity causing handwriting changes, or difficulty in manipulation of small or fine objects, or - minor loss of grip strength causing difficulty in gripping moderately heavy to heavy objects. - Can use limb efficiently for normal tasks without excessive fatigue for no more than ten minutes.
|
FIFTEEN | Can use limb reasonably well in most circumstances, but frequent difficulties are manifested by: - minor loss of digital dexterity causing handwriting changes, or difficulty in manipulation of small or fine objects, and - minor loss of grip strength causing difficulty in gripping moderately heavy to heavy objects. |
TWENTY | Can use limb reasonably well in some circumstances, but with more noticeable difficulty manifested by either or both of: - minor loss of digital dexterity and reduced grip strength causing difficulty in manipulation of larger objects, or - major loss of digital dexterity causing marked difficulty in handwriting or manipulation of everyday domestic objects. |
THIRTY | Can use limb reasonably well in a few circumstances only. Use of limb is otherwise inefficient, with increasing difficulty for self-care activities. Poor digital co-ordination and markedly reduced grip strength in, eg, lifting light objects. Problems with dressing, feeding or writing. |
FORTY | Uses limb inefficiently in all circumstances. Use of limb subject to major limitations, capable of light grip only. Aids, eg, splints, required for everyday activities such as writing and eating. |
FIFTY | Has only some movement against gravity at elbow, shoulder or wrist. |
SIXTY | Unable to use upper limb at all. |
| Only one rating is to be selected from this table for each upper limb, for any condition or combination of conditions. |
| | |
Step 7: Determine if any Other Impairment rating applies to the right upper limb.
There are three Other Impairment tables relating to the upper limb. These are:
Table 3.1.3 — Amputations of Fingers and Thumb; and
Table 3.1.4 — Amputations of Upper Limb; and
Table 3.1.5 — Dislocation of Shoulder.
Not more than one rating may be selected from either Table 3.1.3 or Table 3.1.4, if the veteran has an amputation affecting the right upper limb.
An additional rating may be selected from Table 3.1.5 if it is applicable to the right shoulder.
If no ratings from Tables 3.1.3 or 3.1.4 or 3.1.5 apply to the right upper limb, then the functional impairment rating obtained under Step 6 is the final functional impairment rating for the right upper limb.
Step 8: Compare the final functional impairment rating for the right upper limb with any Other Impairment rating applicable to the right upper limb. Take the higher of these ratings.
The final functional impairment rating obtained in Step 6 is to be compared with the impairment rating for that limb obtained in Step 7 (if any).
The higher of the two ratings is then to be taken as the total final impairment rating for the right upper limb.
If multiple accepted conditions are responsible for the impairment of an upper limb, the situation will be more complicated and may require applying Chapter 20 (Apportionment).
If the veteran has received a rating from either Table 3.1.3 or Table 3.1.4 and also a rating from Table 3.1.5 the substeps below are to be followed.
Substep 8A | The functional impairment rating for the right upper limb, obtained in Step 6, is to be apportioned into two or three parts, as appropriate, by applying Chapter 20 (Apportionment). The parts are: - one part corresponding to the impairment due to amputations affecting the right upper limb;
- one part corresponding to the impairment due to dislocation of the right shoulder;
- one part corresponding to the impairment (if any) of the right upper limb due to all causes other than dislocation of shoulder and amputations.
|
Other Impairment Table 3.1.3 | 
|
AMPUTATIONS OF FINGERS AND THUMB |
Impairment Ratings | Criteria |
NIL | No amputation of fingers or thumb. |
TWO | Amputation of little finger of one hand. |
FIVE | Amputation of ring finger of one hand. |
TEN | - Amputation of index finger of one hand
- Amputation of middle finger of one hand.
- Amputation of ring and little fingers of one hand.
|
FIFTEEN | - Amputation of index and little fingers of one hand.
- Amputation of middle and little fingers of one hand.
- Amputation of index and ring fingers of one hand.
- Amputation of middle and ring fingers of one hand.
|
TWENTY | - Amputation of thumb of one hand.
- Amputation of index and middle fingers of one hand
- Amputation of index, ring, and little fingers of one hand.
- Amputation of middle, ring, and little fingers of one hand.
|
TWENTY-FIVE | - Amputation of thumb and ring finger of one hand.
- Amputation of thumb and little finger of one hand.
- Amputation of index, middle, and ring fingers of one hand.
- Amputation of index, middle, and little fingers of one hand.
|
THIRTY | - Amputation of thumb and index finger of one hand.
- Amputation of thumb and middle finger of one hand.
- Amputation of thumb, index and little fingers of one hand.
- Amputation of thumb, middle and little fingers of one hand.
- Amputation of thumb, ring, and little fingers of one hand.
- Amputation of index, middle, ring and little finger, but not thumb, of one hand.
|
THIRTY-FIVE | - Amputation of thumb, index, and middle fingers of one hand.
- Amputation of thumb, index and ring fingers of one hand.
- Amputation of thumb, middle and ring fingers of one hand.
- Amputation of thumb, index, ring, and little fingers of one hand.
- Amputation of thumb, middle, ring, and little fingers of one hand.
|
FORTY | - Amputation of thumb, index, middle, and ring fingers of one hand.
- Amputation of thumb, index, middle, and little fingers of one hand.
|
FORTY-FIVE | Amputation of index, middle, ring, and little fingers, and thumb, of one hand. |
| One rating may be given from this table for each side, as applicable. |
| | |
Other Impairment Table 3.1.4 | 
|
AMPUTATIONS OF UPPER LIMB |
Impairment Ratings | Criteria |
NIL | No amputations involving the upper limb. |
FIFTY | - Mid-carpal amputation of one hand.
- Mid-metacarpal amputation of one hand.
- Disarticulation at wrist joint.
- Amputation of forearm distal to biceps tendon insertion.
|
SIXTY | - Amputation of forearm proximal to biceps tendon insertion.
- Disarticulation at elbow.
- Amputation between deltoid insertion and elbow.
- Amputation above deltoid insertion.
- Disarticulation at shoulder.
|
SEVENTY | Forequarter amputation. |
| One rating may be given from this table for each upper limb, as applicable. |
| | |
Other Impairment Table 3.1.5 | 
|
DISLOCATION OF SHOULDER |
Impairment Ratings | Criteria |
NIL | - No recurrent dislocation of shoulder.
- Dislocation of shoulder on a single occasion.
|
TWO | Recurrent dislocation of shoulder surgically corrected. |
FIVE | Recurrent dislocation of shoulder not surgically corrected. |
TEN | Dislocation of shoulder resulting in prophylactic restriction of movement. |
| Only one rating is to be selected from this table for each shoulder. |
| | |
Substep 8B | Compare the apportioned functional impairment rating corresponding to the impairment due to amputations affecting the right upper limb (obtained in substep 8A) with the Other Impairment rating from either Table 3.1.3 or Table 3.1.4 (obtained in Step 7). The higher of these two ratings is to be selected. |
Substep 8C | Compare the apportioned functional impairment rating corresponding to the impairment due to dislocations of the right shoulder (obtained in substep 8A) with the Other Impairment rating from Table 3.1.5 (obtained in Step 7). The higher of these two ratings is to be selected. |
Substep 8D | The veteran’s accepted right upper limb condition(s) will receive (up to) three impairment ratings: - The functional impairment rating corresponding to the impairment of the right upper limb due to all causes other than amputations and dislocation of shoulder (if such a rating is obtained in substep 8A);
- The impairment rating obtained in substep 8B; and
- The impairment rating obtained in substep 8C.
These ratings are not to be combined at this stage but are to be included in the final combining of all ratings. |
Example 1
A veteran has an amputation of the right thumb as the only accepted disability of the right upper limb.
By following steps 1 to 7 inclusive, a rating will have been selected
from Table 3.1.2:
probably 20 to 40 impairment points (depending on the severity of the effect on the hand)
from Table 3.1.3:
20 impairment points.
These two ratings are compared and the veteran receives the higher as the final impairment rating for the right upper limb.
Example 2
A veteran has an amputation of his right thumb and dislocation of the right shoulder as the only accepted conditions of the right upper limb.
By following steps 1 to 7 inclusive, a rating will have been selected
from Table 3.1.2:
say, 40 impairment points (the veteran can use the right upper limb reasonably well in a few circumstances only)
from Table 3.1.3:
20 impairment points; and
from Table 3.1.5:
10 impairment points.
Medical evidence shows that the incapacity of the veteran’s right upper limb is due 80% to the shoulder condition and 20% to the amputated thumb. Apportioning the 40 impairment points in the ratio of 4:1, 34 points are obtained for the shoulder, and 9 points for the thumb (Table 20.1).
After comparing the apportioned functional impairment rating of 34 for the right shoulder with the Other Impairment rating of 10 from Table 3.1.5, the veteran gets 34 points for the shoulder. After comparing the apportioned functional impairment rating of 9 for the amputated right thumb with the Other Impairment rating of 20 from Table 3.1.3, the veteran gets 20 points for the amputation of the right thumb.
In this case the final impairment ratings for the right upper limb are 34 points and 20 points. These are to be included in the final combining of all ratings.
An Upper Limb Worksheet is provided on page 70. |
A separate Upper Limb Worksheet is to be used for each upper limb. If, for either upper limb, two Other Impairment ratings are applicable the Functional Impairment rating (E) is to be compared with the Other Impairment ratings in accordance with Step 8. |
Because the two lower limbs constitute a functional unit, a single functional impairment rating is calculated for both lower limbs together.
Calculation of the impairment rating for conditions of the lower limbs
Follow the steps below to calculate the impairment rating due to accepted conditions of the lower limbs:
(Each step is elaborated in the following pages.)
Step 1 | Establish which joints in the lower limbs, if any, have some restriction of movement as a result of accepted conditions affecting the lower limbs. | Page 50 |
Step 2 | (Omit this step if there is no restriction of joint movement in the limbs.) Calculate the functional impairment due to restriction of the range of movement of joints in the lower limbs as a result of accepted conditions of the lower limbs. | Page 51 |
Step 3 | Make any applicable age adjustment to the final functional impairment rating for the limbs by applying Table 3.6.1 in Part 3.6 of this chapter. | Page 53 |
Step 4 | Calculate the functional impairment rating for the lower limbs as a whole by applying Table 3.2.2. | Page 54 |
Step 5 | Compare the functional impairment rating for the lower limbs as a whole with the functional impairment rating due to any restricted range of movement. Take the higher of these two ratings as the final functional impairment rating for the limb. | Page 56 |
Step 6 | Determine if any Other Impairment rating applies to the lower limbs. | Page 56 |
Step 7 | (Omit this step if no Other Impairment rating applies to the limbs.) Compare the final functional impairment rating for the limbs with any Other Impairment rating applicable to the limbs. Take the higher of these ratings. | Page 56 |
Step 1: Establish which joints in the lower limbs, if any, have some restriction of movement as a result of accepted conditions affecting the lower limbs.
For the purposes of assessment under this Guide, the major joints of the lower limbs are the hip, the knee and the ankle.
In addition, the joints of the toes are also to be considered. However, only one rating is to be given for the total effect of restrictions in all joints of the toes of one foot considered together.
Conditions such as chondromalacia patellae and torn medial meniscus may affect the range of movement of the knee. A condition such as fractured neck of femur will be likely to affect the range of movement of the hip. In cases of a fracture, the ranges of movements of the joints both proximal to and distal to the fracture site should generally be considered as joints the range of movement of which may be affected. The closer a fracture site is to a joint, the more likely it is that it will have some effect on the range of movement of that joint.
Hence, it must be determined which, if any, of both right and left:
potentially have loss of range of movement due to accepted conditions.
Certain vascular conditions or neurological conditions of the lower limb, such as muscle weakness, tremor, apraxia, or loss of co-ordination may have an effect on the function of the lower limb without restricting the range of movement of any joint of the limbs. The assessment of such conditions is made under Step 4 of this Part.
Step 2: Calculate the functional impairment due to restriction of the range of movement of joints in the lower limbs as a result of accepted conditions of the lower limbs.
Single functional impairment ratings may be obtained for each of the following eight joints or sets of joints based on restriction of range of movement due to accepted conditions:
These impairment ratings are obtained by applying Table 3.2.1. Such functional impairment ratings are referred to as the functional impairment rating of the relevant lower limbs based on restriction or range of movement of the right or left hip, knee, ankle, or toes respectively.
The loss of range of movement is to be estimated to the nearest quarter of the normal range of movement.
The range of movement relevant to assessment under this Guide is the active range of movement of the joint, that is the range through which the veteran can move the joint by virtue only of those muscles whose normal function it is to do so. The ability of a veteran to flex a joint by use of other, non-affected body parts does not reduce the rating which the impaired joint attracts. (For example, if a veteran cannot flex the right knee in the normal fashion, by use of the hamstring muscles, but can use a hand to bend the right knee, the right knee should be assessed as having “loss of almost all movement”.)
“Unfavourable position” and “position of function” and “flail joint” are defined at page 41.
The loss of range of movement will usually be provided as a fractional loss of range of movement and such data can be related directly to items within Table 3.2.1. However, sometimes, the measured movements of an affected joint will be available in degrees. In such a case the measured movement is to be compared with the average range of movement of a normal joint to obtain the fractional loss of range of movement.
The average ranges of movement of various normal joints of the lower limbs may be obtained from Table 3.5.1 in Part 3.5 of this Chapter. These values are to be used in arriving at the fractional loss of range of movement when the movements of a joint are known in degrees.
If non-accepted conditions contribute to the loss of range of movement, Chapter 19 (Partially Contributing Impairment) is to be used in conjunction with Table 3.2.1.
If various impairment ratings have been obtained for lower limb joints, and Chapter 19 has been applied to them, take the highest resultant rating. This is the final functional impairment rating for the lower limbs based on loss of range of movement. If Chapter 19 did not have to be applied, then take the highest of the various impairment ratings that have been obtained for each lower limb joint. In that case, this is the final functional impairment rating for the lower limbs.
Functional Loss Table 3.2.1 | 
|
LOSS OF MUSCULOSKELETAL FUNCTION: LOWER LIMB JOINTS |
Impairment Ratings | Hip | Knee | Ankle | Toes |
NIL | X-ray changes only with normal range of movement. | X-ray changes only with normal range of movement. | X-ray changes only with normal range of movement. | Incomplete loss of range of movement of any toe. |
TWO | | | | Ankylosis of any toe other than hallux. |
FIVE | | | Loss of about one-quarter normal range of movement. | Hallux: ankylosis in favourable position of either interphalangeal joint; or metatarsophalangeal joint. |
TEN | Loss of about one-quarter normal range of movement. | Loss of about one-quarter normal range of movement. | Loss of about one-half normal range of movement. | Hallux: ankylosis in an unfavourable position of either interphalangeal joint and/or metatarso-phalangeal joint. |
FIFTEEN | | | Loss of about three-quarters normal range of movement. | |
TWENTY | Loss of about one-half normal range of movement. | Loss of about one-half normal range of movement. | Loss of almost all movement, or complete ankylosis in position of function. | |
THIRTY | Loss of about three-quarters normal range of movement. | Loss of about three-quarters normal range of movement. | Ankylosis in an unfavourable position, or a flail joint. | |
FOURTY | Loss of almost all movement, or complete ankylosis in position of function. | Loss of almost all movement, or complete ankylosis in position of function. | | |
FIFTY | Ankylosis in an unfavourable position, or a flail joint. | Ankylosis in an unfavourable position, or a flail joint. | | |
| Only one rating is to be selected from this table for each hip, knee, or ankle; and only one rating is to be selected from this table for the toes of each foot. Of these ratings only the highest is to be taken. |
| | | | | |
Step 3: Make any applicable age adjustment to the functional impairment rating for the lower limbs based on loss of range of movement by applying Table 3.6.1 in Part 3.6 of this chapter.
The functional impairment rating based on loss of range of movement obtained in Step 2 is to be age adjusted using Table 3.6.1.
For veterans aged 46 to 55 years at the relevant time, age adjustment will not result in any change of the impairment rating. For veterans aged 56 years and older at the relevant time, the impairment rating will be reduced by an amount dependent upon their age. For veterans aged 45 years or less at the relevant time, the impairment rating will be increased by an amount dependent upon their age.
Total loss of function of each lower limb is considered to be 50 per cent impairment of the whole person. Amputation of a lower limb at the hip joint, or total loss of the use of a lower limb is equivalent to 50 impairment points.
With the exception of a hindquarter amputation, no condition or combination of conditions causing impairment in a lower limb shall receive an impairment rating exceeding 50 points.
In the case of a veteran aged 45 years or less, if the application of age adjustment to the functional impairment rating results in an impairment rating higher than 50 impairment points, the functional impairment rating for that lower limb is to be taken as 50 impairment points and not as the higher rating obtained by applying Table 3.6.1.
Step 4: Calculate the functional impairment rating for the lower limbs as a whole by applying Table 3.2.2.
Table 3.2.2 measures the loss of function relating to the two lower limbs together. Only one rating is to be given from this table for any condition or combination of conditions. To attract a particular rating, the degree of impairment must be greater than that described at all lower levels.
Impairment ratings derived from Table 3.2.2 are not to be age adjusted by applying Table 3.6.1. The reason is that many of the criteria within the table are age-dependent: they compare veterans with others of the same age.
Table 3.2.2 is the only relevant table if the use of lower limbs is restricted by vascular conditions or neurological conditions, such as muscle weakness, tremor, apraxia, loss of co-ordination, fatigue or pain, and when no condition affecting the range of movement of a joint is present.
If non-accepted conditions contribute to the loss of function, Chapter 19 (Partially Contributing Impairment) is to be applied in conjunction with Table 3.2.2.
Functional Loss Table 3.2.2 | 
|
LOSS OF MUSCULOSKELETAL FUNCTION: LOWER LIMBS (BASED ON USE OF BOTH LOWER LIMBS TOGETHER) |
Impairment Ratings | Criteria |
NIL | - Walks in a manner normal for age on a variety of different terrains and at varying speeds.
- Sciatic pain — occasional twinges but no effect on walking most of the time.
|
FIVE | - Walks with intermittent difficulty, such as locking or giving way, without falling. Caution needed on steps and uneven ground, or when running.
- Has intermittent pain from weight-bearing, ie, not all the time, or only after weight-bearing for some time.
- Sciatic pain occurring frequently: present some of the time when walking.
|
TEN | - Walks at normal pace on level ground, but has constant difficulty up and down steps and over uneven ground. Need for a walking stick may be manifested:
Pain and/or slowness; or constant pain from weight-bearing. - Pain restricts walking to 500 m or less, at a slow to moderate pace (4 km/h). Can walk further after resting.
- Sciatic pain daily — present most of the time during walking.
|
TWENTY | - Walks at moderately reduced pace in comparison with peers on flat ground; and is unable to
manage stairs or ramps without rails; or rise from the sitting position without the assistance of one hand. - Pain restricts walking (4 km/h) to 250 m or less at a time. Can walk further after resting.
|
THIRTY | - Walks at significantly reduced pace in comparison with peers and:
legs give way frequently, resulting in falls. Can walk more efficiently with a brace or an artificial limb; or is unable to negotiate stairs without personal assistance; or is unable to rise to standing position without the assistance of both hands. - Pain restricts walking (4 km/h) to 100 m or less at a time. Can walk further after resting.
|
FORTY | - Walks at greatly reduced pace in comparison with peers, is unable to negotiate kerbs, gutters or uneven ground, and
is restricted to walking in home and around block. Probably needs a walking aid; or finds transfer difficult without personal assistance. - Pain restricts walking (4 km/h) to 50 m or less at a time. Can walk further after resting.
|
| Restricted to walking in and around home; and requires quad stick, crutches or similar walking aid; is unable to transfer without personal assistance. |
SIXTY | Restricted to walking in and around home. Can walk only with personal assistance, or with a walking aid such as a pickup frame. |
SEVENTY | Unable to walk or stand. Mobile only in a wheelchair. |
| Only one rating is to be selected from this table for any condition or combination of conditions. |
| | |
For the purposes of Table 3.2.2 “transfer” means:
- a move from one seat to another;
- a move from sitting to standing;
- a move on and off the toilet; or
- a move in and out of bed.
Step 5: Compare the functional impairment rating for the lower limbs as a whole with the functional impairment rating due to any restricted range of movement. Take the higher of these two ratings as the final functional impairment rating for the limbs.
After applying Chapter 19 (Partially Contributing Impairment) in Step 4, the functional impairment rating from loss of range of movement is to be compared with the functional impairment for the use of the limbs as whole.
The higher of these two ratings is the final functional impairment rating for the limbs.
Step 6: Determine if any Other Impairment rating applies to the lower limbs.
There are two Other Impairment tables relating to the lower limbs:
Table 3.2.3 — Amputations of Lower Limbs; and
Table 3.2.4 — Lower Limbs - Joint Replacements.
Step 7: Compare the final functional impairment rating for the lower limbs with any Other Impairment rating applicable to the lower limbs. Take the higher of these.
Substep 7A | When the only Other Impairment rating relates to amputations. The final functional impairment rating of the lower limbs (obtained in Step 5) is to be compared with the Other Impairment rating or ratings from Table 3.2.3. The higher of the two ratings is then taken as the total final impairment rating for the lower limbs. |
Other Impairment Table 3.2.3 | 
|
AMPUTATIONS OF LOWER LIMBS |
Impairment Ratings | Criteria |
NIL | No amputation of any toes. |
TWO | Amputation of single toe other than great toe. |
FIVE | Amputation of 2 to 4 toes on foot excluding great toe. |
TEN | - Amputation of great toe.
- Amputation of great toe and one other toe on one foot.
|
FIFTEEN | - Amputation of great toe and 2 or more other toes on one foot.
- Mid-metatarsal amputation.
|
TWENTY | Mid-tarsal amputation. |
THIRTY | - Amputation at ankle.
- Amputation below knee with functional stump.
|
FORTY | - Amputation above knee with functional stump.
- Disarticulation at knee.
- Amputation below knee with short stump (that is 7.5 cm or less below intercondylar notch).
|
FIFTY | - Disarticulation at hip joint.
- Amputation above knee with short stump (that is 7.5 cm or less below tuber ischii).
|
SIXTY | Hemipelvectomy. |
| If applicable, ratings may be given from this table for each of the lower limbs. |
| | |
Other Impairment Table 3.2.4 | 
|
LOWER LIMBS: JOINT REPLACEMENTS AND REALIGNMENTS |
Impairment Ratings | Criteria |
NIL | No joint replacement or realignment in lower limbs. |
FIVE | Tibial osteotomy |
TEN | - Total knee replacement.
- Total hip replacement
|
| Where applicable, up to four ratings may be made from this table — one rating for each knee and one for each hip. |
| | |
Example:
A veteran has an amputation of his right foot as the only accepted condition of his lower limbs which upon investigation is found to fit the description of “amputation below knee with functional stump”.
By following steps 1 to 6 inclusive, a rating will have been selected:
from Table 3.2.2:
probably 10 to 30 impairment points (depending on the severity of the effect of the amputation on the particular veteran);
from Table 3.2.3:
30 impairment points.
These two ratings are to be compared and the veteran receives the higher as the total final impairment rating for his amputation of right foot.
If multiple accepted conditions are responsible for the impairment of the lower limbs, the situation will be more complicated and may require applying Chapter 20 (Apportionment).
In some cases, two other impairment ratings are to be given. In such cases, the functional impairment for the limbs should be apportioned into three parts:
- one part corresponding to the impairment due to any amputation of the right leg;
- one part corresponding to the impairment due to any amputation of the left leg; and
- one part corresponding to all other causes.
Substep 7B | When the only Other Impairment rating relates to joint replacements and realignments. Ratings from Table 3.2.4 are to be given only if both the following conditions apply: - the predominant cause of loss of lower limb function is a vascular condition (such as peripheral vascular disease); and
- the rating obtained from Table 3.2.2 is higher than the highest rating obtained from Table 3.2.1.
Other Impairment rating or ratings from Table 3.2.4 are to be included in the final combining of all impairment ratings. Unlike Other Impairment ratings from most other tables, ratings from Table 3.2.4 are not to be compared with a functional impairment rating. |
Example:
A veteran has osteoarthritis of both knees as an accepted condition and has had bilateral knee replacements resulting in reasonably good function. The veteran also has peripheral vascular disease as an accepted condition which limits walking distance to about 200 metres.
By following steps 1 to 6 inclusive, a rating will have been selected:
from Table 3.2.2:
20 impairment points; and
two ratings will have been selected from Table 3.2.4:
10 impairment points for the right knee replacement; and
10 impairment points for the left knee replacement.
The veteran receives all three impairment ratings. The three ratings are to be included in the final combining of all impairment ratings.
The following conditions, whether alone or in combination, are to be assessed by applying Table 3.2.5 if they have no effect on lower limb function. If these conditions have an effect on lower limb function they are to be assessed by applying Table 3.2.2.
Other Impairment Table 3.2.5 | 
|
MINOR DISORDERS OF THE LOWER LIMBS |
Impairment Ratings | Criteria |
NIL | - Pes planus with no symptoms.
- Hammer toes with no symptoms.
- Claw toes with no symptoms.
- Hallux valgus with no symptoms.
- Calcaneal spurs with no symptoms.
- Genu varum with no symptoms.
- Genu valgum with no symptoms.
|
TWO | - Pes planus with minor symptoms.
- Hammer toes with minor symptoms.
- Claw toes with minor symptoms.
- Hallux valgus with minor symptoms.
- Calcaneal spurs with minor symptoms.
- Genu varum with minor symptoms.
- Genu valgum with minor symptoms.
|
| Where applicable a rating is to be selected from this table for each condition. |
| | |
A Lower Limbs Worksheet is provided on page 69.
A single Lower Limbs Worksheet is to be used for both lower limbs together. The Lower Limbs Worksheet is designed to facilitate calculation of the functional impairment of the lower limbs. That functional impairment is to be compared with any Other Impairment ratings in accordance with this Guide.
Part 3.3 of Chapter 3 is to be applied in assessing impairment of the spinal column, not of the spinal cord. Impairments of the spinal cord are to be assessed by applying Chapter 5 of this Guide.
For the purposes of assessment under Part 3.3 the spine consists of two parts — the cervical spine and the thoraco-lumbar spine — each of which is to be given a separate impairment rating if appropriate.
Determination of the impairment rating for conditions of the spine.
Follow the steps below to determine the impairment rating from accepted conditions affecting the function of the spine. Because the cervical spine and the thoraco-lumbar spine are each to be separately assessed, this set of steps is to be followed twice (if applicable): once for the cervical spine and once for the thoraco-lumbar spine.
(Each step is elaborated in the following pages.)
STEP 1 | Calculate the functional impairment due to restriction of range of movement of the spine as a result of accepted conditions. | Page 60 |
STEP 2 | (Omit this step if you are not assessing an impairment of the thoraco-lumbar spine.) Determine the impairment rating applicable to the thoraco-lumbar spine by applying Table 3.3.2. | Page 61 |
STEP 3 | (Omit this step if you are not assessing an impairment of the thoraco-lumbar spine.) Compare the rating obtained in Step 1 in respect of impairment of the thoraco-lumbar spine with the rating obtained in Step 2. Take the higher rating. | Page 63 |
STEP 4 | Make any applicable age adjustment to the functional impairment rating for the spine by applying Table 3.6.1. | Page 63 |
STEP 5 | Determine if any Other Impairment rating applies to the spine. | Page 63 |
STEP 6 | Compare the impairment rating obtained in Step 4 with the impairment rating obtained in Step 5. Take the higher rating. | Page 64 |
Step 1: Calculate the functional impairment due to restriction of range of movement of the spine as a result of accepted conditions.
Table 3.3.1 is to be applied to rate spinal function. It is based on range of movement of the spine. Two ratings may be given from this table — one for the cervical spine and one for the thoraco-lumbar spine. Only one rating is to be given for the cervical spine for any condition or combination of conditions which contribute to the loss of range of movement of the cervical spine. Only one rating is to be given for the thoraco-lumbar spine for any condition or combination of conditions that contribute to the loss of range of movement of the thoraco-lumbar spine.
It is not practicable to measure range of movement of the thoracic spine independently of that of the lumbar spine. If only the thoracic spine is to be rated, all movements are to be measured, but emphasis is given to rotation. If only the lumbar spine is to be rated, all movements are to be measured, but emphasis is given to forward flexion. However, even if conditions of both the thoracic and lumbar spine are to be assessed, only one rating is to be made from the thoraco-lumbar spine column of Table 3.3.1.
The loss of range of movement should be estimated to the nearest quarter of the normal range of movement.
The loss of range of movement will usually be provided as a fractional loss of range of movement and such data can be used directly in Table 3.3.1. However, sometimes, the measured movements of the affected part of the spine will be available in degrees. In such a case the measured movement is to be compared with the average range of movement of the normal spine to obtain the fractional loss of range of movement.
The average ranges of movement of the normal spine may be obtained from Table 3.5.1 in Part 3.5. These values are to be used in arriving at the fractional loss of range of movement when the actual movements of the spine are known in degrees.
If a functional impairment rating obtained from Table 3.3.1 has been contributed to by any non-accepted conditions, then that rating is to be moderated by applying Chapter 19 (Partially Contributing Impairment).
Step 2: (Omit this step if you are not assessing an impairment of the thoraco-lumbar spine.) Determine the impairment rating applicable to the thoraco-lumbar spine by applying Table 3.3.2.
Table 3.3.2 is to be applied to assess functional loss of the thoraco-lumbar spine that is not adequately measured by loss of range of movement. Ratings obtained from Table 3.3.2 are not to be combined with any ratings obtained from Table 3.3.1 in respect of the thoraco-lumbar spine. Ratings obtained from Table 3.3.2 are compared with ratings obtained from Table 3.3.1 in respect of the thoraco-lumbar spine in Step 3.
If a functional impairment rating obtained from Table 3.3.2 has been contributed to by any non-accepted conditions, then that rating is to be moderated by applying Chapter 19 (Partially Contributing Impairment).
Functional Loss Table 3.3.1 | 
|
LOSS OF MUSCULOSKELETAL FUNCTION: SPINAL MOVEMENT |
Impairment Ratings | Criteria | |
| Cervical spine | Thoraco-lumbar spine |
NIL | X-ray changes only. Normal or nearly normal range of movement. | X-ray changes only. Normal or nearly normal range of movement. |
FIVE | Loss of about one-quarter of normal range of movement. | |
TEN | Loss of about half of normal range of movement | Loss of about one-quarter normal range of movement. |
FIFTEEN | Loss of about three-quarters of normal range of movement. | |
TWENTY | Loss of almost all movement, or complete ankylosis in position of function | Loss of about half of normal range of movement. |
THIRTY | Ankylosis in an unfavourable position. | Loss of about three-quarters of normal range of movement. |
FORTY | | Loss of almost all movement, or complete ankylosis in position of function. |
FIFTY | | Ankylosis in an unfavourable position, or unstable joint. |
| Where applicable, two ratings are to be selected from this table — one for the cervical spine and one for the thoraco-lumbar spine. |
| | | |
Functional Loss Table 3.3.2 | 
|
LOSS OF MUSCULOSKELETAL FUNCTION:
THORACO-LUMBAR SPINE (BASED ON USE OF SPINE) |
Impairment Ratings | Criteria |
NIL | Thoraco-lumbar spine condition causes no difficulty in sitting or standing or other normal activities. |
TWO | Thoraco-lumbar spine condition causes occasional difficulties in prolonged sitting or standing. |
FIVE | Thoraco-lumbar spine condition causes difficulties in sitting or standing that generally result in pain or undue fatigue by the end of the day. |
TEN | Thoraco-lumbar spine condition generally causes pain or undue fatigue within half an hour, and so requires frequent changes of posture. |
FIFTEEN | Thoraco-lumbar spine condition generally causes pain or undue fatigue within five minutes, and so requires very frequent changes of posture. |
| One rating may be selected from this table in respect of the thoraco-lumbar spine. No rating is to be selected from this table in respect of the cervical spine. |
| | |
Step 3: (Omit this step if you are not assessing an impairment of the thoraco-lumbar spine.) Compare the rating obtained in Step 1 in respect of impairment of the thoraco-lumbar spine with the rating obtained in Step 2. Take the higher rating.
Step 4: Make any applicable age adjustment to the functional impairment rating for the spine by applying Table 3.6.1.
The functional impairment rating obtained in Step 4 is to be age adjusted by applying Table 3.6.1. Unlike the situation which applies to the upper and lower limbs there is no maximum value of the impairment rating of the spine. Hence whatever the rating obtained by application of Table 3.6.1 is the rating to be given. (The reason is that the maximum rating for limbs is determined by reference to the rating given for amputation of the limb, but there is no such thing as amputation of the spine.)
Step 5: Determine if any Other Impairment rating applies to the spine.
The Other Impairment ratings of the spine are those due to crush fractures of the vertebrae.
Other Impairment Table 3.3.3 | 
|
CRUSH FRACTURES OF THE VERTEBRAE |
Impairment Ratings | Criteria |
NIL | |
TWO | Crush fracture with minor compression (less than 25%) only. |
FIVE | Crush fracture of one vertebra (compression of 25%-50%). |
TEN | - Crush fracture of a single vertebra with more than 50% compression.
- Crush fracture of two or more vertebrae with more than 25% compression of each.
|
| Where applicable, two ratings are to be selected from this table — one for the cervical spine and one for the thoraco-lumbar spine. |
| | |
Step 6: Compare the impairment rating obtained in Step 4 with the impairment rating obtained in Step 5. Take the higher rating.
After applying Chapter 19 (Partially Contributing Impairment), the functional impairment rating due to loss of range of movement of the spine is to be compared with the functional impairment due to any crush fractures.
The higher of these two ratings is the final functional impairment rating for the cervical or thoraco-lumbar spine, as the case may be.
The assessment of other effects of spinal conditions.
If a spinal condition causes an effect on limb function, then that effect on limb function is also to be assessed under Parts 3.1 or 3.2 of this chapter (together with the effect of any other accepted conditions contributing to loss of function of the same limb); and if a spinal condition causes a sensory loss, then that sensory loss is also to be assessed under Table 5.4 (together with the effect of any other accepted conditions contributing to that sensory loss).
For example, if a spinal condition which causes a reduced range of spinal movement also interferes with the proper function of the limbs, then a rating from Table 3.3.1 may be combined with a rating from Table 3.1.2 or 3.2.2.
A Cervical Spine Worksheet is provided at page 71.
A Thoraco-Lumbar Spine Worksheet is provided at page 72.
PART 3.4: RESTING JOINT PAIN
An additional rating is to be given from Table 3.4.1 for certain joint pain. This table is to be applied only for frequent joint pain that continues to affect a joint when the joint is no longer in use: for example, pain in the knees continuing for a significant period after ceasing walking and standing, or pain in the shoulders persisting for a significant period after ceasing some task such as hanging out the washing. Pain that limits range of movement or distance that can be walked is already assessed elsewhere (Tables 3.2.1 and 3.2.2).
Table 3.4.1 may be applied for pain in both the upper limbs and lower limbs and intervertebral joints. Only one selection may be made from this table for pain in any joint or combination of joints. However, the table is not to be applied to rate sciatic pain. Sciatic pain is to be rated by applying Table 3.2.2.
Other Impairment Table 3.4.1 | 
|
RESTING JOINT PAIN |
Impairment Ratings | Criteria |
NIL | Pain in any joint, or combination of joints, that is not usually present at rest. |
TWO | - Pain in any joint, or combination of joints, that is often present at rest but which is mild.
- Pain in the back that limits comfortable sitting to less than 30 minutes at a time.
|
FIVE | - Pain in any joint, or combination of joints, that is often present at rest but which improves after several hours rest or responds to medication or to therapeutic measures.
- Pain in the back that limits comfortable sitting to less than 10 minutes at a time.
|
TEN | Severe pain in any joint, or combination of joints, that is often present at rest but which does not respond adequately to medication or to therapeutic measures. |
FIFTEEN | Severe pain in any joint, or combination of joints, that is always present at rest but which does not respond adequately to medication or to therapeutic measures and which regularly interferes with sleep. |
| Only one selection is to be made from this table for pain in any joint or combination of joints. |
| | |
PART 3.5: RANGES OF JOINT MOVEMENT
Table 3.5.1 is a table of “average” or “normal” values. It is to be used to assist in the estimation of loss of range of joint movement. Range of movement is usually measured by simple visual assessment, and is based on active joint movement. Because estimates of range of movement are required only to the nearest quarter of normal full range of movement, the use of a goniometer is not essential.
A global assessment is based on the measurement and averaging of movements in all planes. Functionally more important planes of movement (Table 3.5.1) are given more emphasis in this assessment. The total loss of range of movement should be estimated to the nearest quarter of the normal range of movement.
Estimates of range of movement may be made using the joint on the opposite side for comparison, provided that the opposite side is not affected by injury or disease. If both sides are affected the accepted normal range of movement given in Table 3.5.1 can be used as a reference.
The angles in brackets represent the position of function. This information is required when considering whether an ankylosis is in a favourable position or not.
Procedural Table 3.5.1 | 
|
AVERAGE RANGES OF JOINT MOVEMENTS |
Joint | Average Range of Joint Movement (degrees) |
Shoulder | Abduction (45º) * 150º Forward elevation (30º) * 150º External Rotation (20º) * 90º | Adduction 30º Backward 40º Internal 40º |
Elbow | Flexion (100º) * 150º Supination (0º) 80º | Extension 0º Pronation 80º |
Wrist | Dorsiflexion (30º) * 60º Ulnar Deviation (0º) 30º | Palmar Flexion • 70º Radial 20º |
Hip | Flexion (25º) 100º Abduction (0º) * 40º Internal Rotation (0º) * 40º | Extension 30º Adduction 20º External 50º |
Knee | Flexion (10º) * 150º | Extension 0º |
Ankle | Dorsiflexion (0º) * 20º Inversion (0º) 30º | Plantar Flexion • 40º Eversion 20º |
Cervical | Flexion (0º) * 45º | Extension • 45º |
Spine | Right Lateral Flexion (0º) 45º Right Rotation (0º) * 80º | Left Lateral Flexion 45º Left Rotation • 80º |
Thoraco- Lumbar Spine | Flexion (0º) * 90º Right Lateral Flexion (0º) 30º Right Rotation (0º) 30º | Extension 30º Left Lateral Flexion 30º Left Rotation 30º |
| *Functionally most important movements |
| | | |
PART 3.6: SPINE AND LIMBS AGE ADJUSTMENT
Table 3.6.1 converts the impairment rating for the measured loss of musculoskeletal function to an age adjusted impairment rating.
Table 3.6.1 | 
|
SPINE AND LIMBS AGE ADJUSTMENT |
Rating | Less than | | | Age | | | Greater than |
36 | 36–45 | 46–55 | 56–65 | 66–75 | 76–85 | 85 |
0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 |
3 | 4 | 3 | 3 | 3 | 2 | 2 | 2 |
4 | 5 | 4 | 4 | 4 | 3 | 3 | 2 |
5 | 6 | 6 | 5 | 5 | 4 | 4 | 3 |
6 | 7 | 7 | 6 | 5 | 5 | 4 | 4 |
7 | 8 | 8 | 7 | 6 | 6 | 5 | 4 |
8 | 10 | 9 | 8 | 7 | 6 | 6 | 5 |
9 | 11 | 10 | 9 | 8 | 7 | 6 | 5 |
10 | 12 | 11 | 10 | 9 | 8 | 7 | 6 |
11 | 13 | 12 | 11 | 10 | 9 | 8 | 7 |
12 | 14 | 13 | 12 | 11 | 10 | 8 | 7 |
13 | 16 | 14 | 13 | 12 | 10 | 9 | 8 |
14 | 17 | 15 | 14 | 13 | 11 | 10 | 8 |
15 | 18 | 17 | 15 | 14 | 12 | 11 | 9 |
16 | 19 | 18 | 16 | 14 | 13 | 11 | 10 |
17 | 20 | 19 | 17 | 15 | 14 | 12 | 10 |
18 | 22 | 20 | 18 | 16 | 14 | 13 | 11 |
19 | 23 | 21 | 19 | 17 | 15 | 13 | 11 |
20 | 24 | 22 | 20 | 18 | 16 | 14 | 12 |
21 | 25 | 23 | 21 | 19 | 17 | 15 | 13 |
22 | 26 | 24 | 22 | 20 | 18 | 15 | 13 |
23 | 28 | 25 | 23 | 21 | 18 | 16 | 14 |
24 | 29 | 26 | 24 | 22 | 19 | 17 | 14 |
25 | 30 | 28 | 25 | 23 | 20 | 18 | 15 |
26 | 31 | 29 | 26 | 23 | 21 | 18 | 16 |
27 | 32 | 30 | 27 | 24 | 22 | 19 | 16 |
28 | 34 | 31 | 28 | 25 | 22 | 20 | 17 |
29 | 35 | 32 | 29 | 26 | 23 | 20 | 17 |
30 | 36 | 33 | 30 | 27 | 24 | 21 | 18 |
31 | 37 | 34 | 31 | 28 | 25 | 22 | 19 |
32 | 38 | 35 | 32 | 29 | 26 | 22 | 19 |
33 | 40 | 36 | 33 | 30 | 26 | 23 | 20 |
34 | 41 | 37 | 34 | 31 | 27 | 24 | 20 |
| | | | | | | | | |
Table 3.6.1 (continued) | 
|
SPINE AND LIMBS AGE ADJUSTMENT continued |
Rating | Less than | | | Age | | Greater than |
36 | 36–45 | 46–55 | 56–65 | 66–75 | 76–85 | 85 |
35 | 42 | 39 | 35 | 32 | 28 | 25 | 21 |
36 | 43 | 40 | 36 | 32 | 29 | 25 | 22 |
37 | 44 | 41 | 37 | 33 | 30 | 26 | 22 |
38 | 46 | 42 | 38 | 34 | 30 | 27 | 23 |
39 | 47 | 43 | 39 | 35 | 31 | 27 | 23 |
40 | 48 | 44 | 40 | 36 | 32 | 28 | 24 |
41 | 49 | 45 | 41 | 37 | 33 | 29 | 25 |
42 | 50 | 46 | 42 | 38 | 34 | 29 | 25 |
43 | 52 | 47 | 43 | 39 | 34 | 30 | 26 |
44 | 53 | 48 | 44 | 40 | 35 | 31 | 26 |
45 | 54 | 50 | 45 | 41 | 36 | 32 | 27 |
46 | 55 | 51 | 46 | 41 | 37 | 32 | 28 |
47 | 56 | 52 | 47 | 42 | 38 | 33 | 28 |
48 | 58 | 53 | 48 | 43 | 38 | 34 | 29 |
49 | 59 | 54 | 49 | 44 | 39 | 34 | 29 |
50 | 60 | 55 | 50 | 45 | 40 | 35 | 30 |
51 | 61 | 56 | 51 | 46 | 41 | 36 | 31 |
52 | 62 | 57 | 52 | 47 | 42 | 36 | 31 |
53 | 64 | 58 | 53 | 48 | 42 | 37 | 32 |
54 | 65 | 59 | 54 | 49 | 43 | 38 | 32 |
55 | 66 | 61 | 55 | 50 | 44 | 39 | 33 |
56 | 67 | 62 | 56 | 50 | 45 | 39 | 34 |
57 | 68 | 63 | 57 | 51 | 46 | 40 | 34 |
58 | 70 | 64 | 58 | 52 | 46 | 41 | 35 |
59 | 71 | 65 | 59 | 53 | 47 | 41 | 35 |
60 | 72 | 66 | 60 | 54 | 48 | 42 | 36 |
61 | 73 | 67 | 61 | 55 | 49 | 43 | 37 |
62 | 74 | 68 | 62 | 56 | 50 | 43 | 37 |
63 | 76 | 69 | 63 | 57 | 50 | 44 | 38 |
64 | 77 | 70 | 64 | 58 | 51 | 45 | 38 |
65 | 78 | 72 | 65 | 59 | 52 | 46 | 39 |
66 | 79 | 73 | 66 | 59 | 53 | 46 | 40 |
67 | 80 | 74 | 67 | 60 | 54 | 47 | 40 |
68 | 82 | 75 | 68 | 61 | 54 | 48 | 41 |
69 | 83 | 76 | 69 | 62 | 55 | 48 | 41 |
70 | 84 | 77 | 70 | 63 | 56 | 49 | 42 |
| | | | | | | | | | | | | |
Table 3.6.1 is to be applied only to impairment ratings derived from Tables 3.1.1, 3.1.2, 3.2.1, 3.3.1, and 3.3.2.
Table 3.6.1 is not to be applied to impairment ratings derived from Tables 3.1.3, 3.1.4, 3.2.2, 3.2.3, 3.2.4, 3.3.3, or 3.4.1.
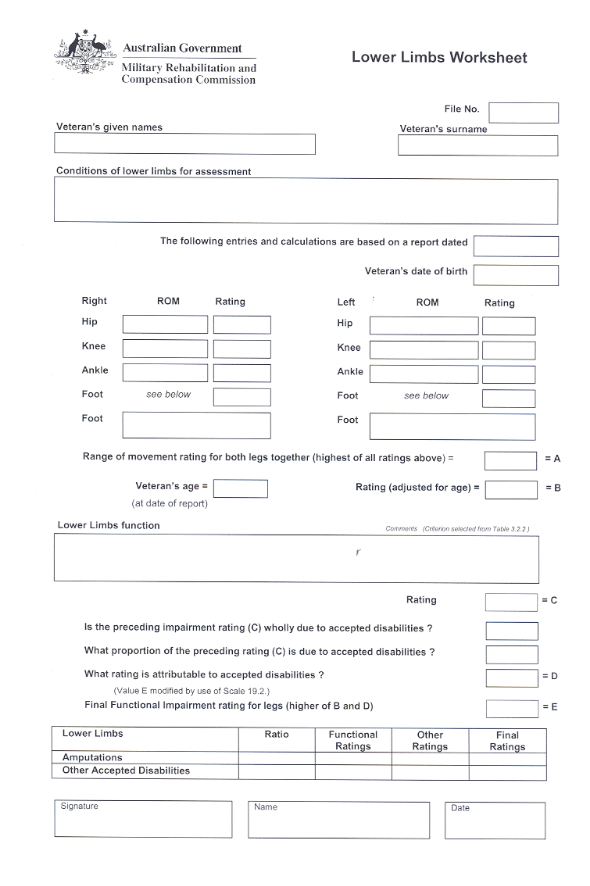


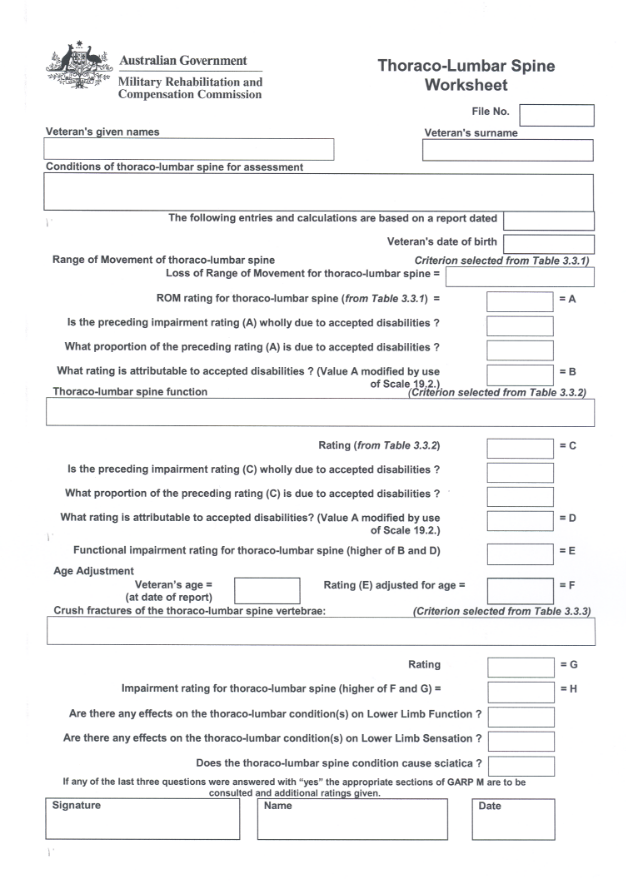
CHAPTER 4
EMOTIONAL AND BEHAVIOURAL
INTRODUCTION
This chapter is only to be applied to assess the emotional and behavioural consequences of accepted psychiatric conditions.
Only one final rating is to be determined using this chapter for any psychiatric condition or combination of psychiatric conditions. If one or more of the veteran’s psychiatric conditions are not accepted conditions, Chapter 19 (Partially Contributing Impairment) is to be applied.
The emotional and behavioural effects of other accepted non-psychiatric conditions are incorporated in the impairment ratings throughout the Guide and may also be taken into account when assessing lifestyle. Where the emotional and behavioural effects of other accepted conditions are such that they warrant a separate psychiatric diagnosis, that psychiatric condition may only be assessed under this chapter if the condition has been accepted as war-caused or defence-caused.
When applying the tables in this chapter, only the effects of the psychiatric condition are to be taken into account. For example, inability to work, reduced participation in recreational activities, and increased family conflict may all be present but not necessarily be consequences of the psychiatric condition.
Some conditions that affect emotional and behavioural function may have symptoms that are intermittent in nature. In these circumstances, Chapter 15 (Intermittent Impairment) should be used, and the rating obtained under that chapter compared with the rating obtained from this chapter. The higher rating is to be taken.
Somatic effects
Psychiatric disease may also be associated with somatic effects such as headache, dyspepsia and psychogenic impotence. If somatic effects occur, they are to be given separate ratings using the respective system-specific tables. It must be clearly established that the somatic effects are part of the psychiatric condition and do not constitute or form part of a separate disease or injury. Conditions in which stress may be implicated as an aetiological agent are not rated under this chapter. These are considered to be separate entitlement issues.
Substance abuse
Substance abuse is to be assessed using Chapter 4 of this Guide. (For purposes of this chapter “substance abuse” includes “substance dependence”.) Chapter 4 is also to be used if substance abuse has been diagnosed under a different, but still psychiatric, diagnostic label.
If substance abuse is an accepted condition in its own right, it is to be assessed by applying Tables 4.1 to 4.8.
If substance abuse is not an accepted condition in its own right but the veteran has an accepted psychiatric condition and substance abuse is a clinical feature of that condition, then substance abuse is to be assessed as part of the accepted psychiatric condition (by applying Tables 4.1 to 4.8) only if the substance abuse was present and part of the veteran’s psychiatric condition when it was originally accepted.
If substance abuse is a clinical feature of the veteran’s accepted psychiatric condition during the assessment period but was not present and part of that condition when it was originally accepted, then substance abuse can only be assessed if it is claimed and accepted as war-caused or defence-caused.
See also the Emotional and Behavioural Medical Impairment Worksheet at pages 83-84.
Calculation of the impairment rating for psychiatric conditions
Follow the steps below to calculate the impairment rating of accepted psychiatric conditions:
(Each step is elaborated in the following pages.)
STEP 1 | Determine an impairment rating from each of Tables 4.1 to 4.8. | Page 74 |
STEP 2 | Find the highest three impairment ratings from Tables 4.3 to 4.8. | Page 74 |
STEP 3 | Add together: - the impairment rating from Table 4.1;
- the rating from Table 4.2; and
the three impairment ratings obtained at Step 2. | Page 75 |
STEP 4 | If the veteran has non-accepted psychiatric conditions, apply Chapter 19 (Partially Contributing Impairment). | Page 75 |
Step 1: Determine a rating from each of Tables 4.1 to 4.8.
Each table addresses a different parameter of psychiatric functioning. The various parameters are described in text placed below the tables.
The examples given in the descriptions of the parameters are not exhaustive. Similar factors may be considered.
While there is some overlap between the various categories, the purpose of considering the condition under the eight headings is to ensure that a wide range of the possible effects of the psychiatric condition are taken into account in arriving at a final impairment rating for the psychiatric condition.
Step 2: Find the three highest impairment ratings from Tables 4.3 to 4.8.
If all or some of the highest impairment ratings are the same, then it does not matter which of these ratings is chosen. For example, if a veteran rates 2, 2, 2, 2, 2 and 2 from Tables 4.3 to 4.8, then the three highest are 2, 2 and 2. If a veteran rates 6, 2, 2, 2, 0 and 0 from Tables 4.3 to 4.8, then the three highest are 6, 2 and 2.
Not all of the criteria in the tables will apply equally to all veterans with accepted psychiatric conditions. For example, Table 4.5 will apply to a different extent to different veterans, depending on their domestic arrangements. Criteria in Table 4.8 will also vary in their application, depending on whether the veteran is receiving treatment. In order to ensure equity in assessment across a broad range of veterans, there are six tables but only the three highest ratings are taken into the assessment.
Step 3: Add together the impairment rating from Table 4.1, the impairment rating from Table 4.2, and the three impairment ratings obtained at Step 2.
Determine the arithmetic sum of the impairment rating from Table 4.1, the impairment rating from Table 4.2, and the three impairment ratings obtained in Step 2, by adding together the five ratings. Chapter 18 (Combined Values Chart) is not to be applied in this process. If the veteran has no non-accepted psychiatric conditions then the impairment rating obtained by adding the five ratings is the final impairment rating for accepted psychiatric condition(s).
Step 4: If the veteran has non-accepted psychiatric conditions, apply Chapter 19 (Partially Contributing Impairment).
Functional Loss Table 4.1 | 
|
SUBJECTIVE DISTRESS | |
Impairment Ratings | General description and outcome |
NIL | Intermittent emotional and behavioural changes that fall within the normal range of human experience. |
TWO | Occasional symptoms causing minor distress. The veteran can easily distract himself or herself from the distress on most occasions. |
THREE | Recurring symptoms causing mild distress. The veteran can distract himself or herself from the distress on most occasions. |
SIX | Frequent symptoms causing moderate distress. The veteran will sometimes be unable to distract himself or herself from the distress. |
TEN | Very frequent symptoms causing moderate distress. The veteran will often be unable to distract himself or herself from the distress. |
FIFTEEN | Persistent symptoms causing considerable distress. Relief for the veteran from that distress is difficult to achieve even with a high level of support and re-assurance. |
TWENTY | Persistent symptoms causing profound distress. The veteran can rarely distract himself or herself from the distress even with a high level of support and reassurance. |
TWENTY-FOUR | Continuous symptoms causing overwhelming distress. The veteran cannot distract himself or herself from the distress even with a high level of support and reassurance. |
| One rating is to be selected from this table for the subjective distress due to the accepted psychiatric condition being assessed. |
| | | |
Subjective distress is the distress that is experienced by the veteran. It is the equivalent of the symptom complex experienced by a veteran with a physical condition.
Examples include feelings of anxiety, fear or depression, flashbacks, intrusive thoughts, loss of concentration, nightmares and hallucinations.
Functional Loss
Table 4.2 | 
|
MANIFEST DISTRESS | |
Impairment Ratings | General description and outcome |
NIL | Nil, minimal, or rare signs of distress. |
TWO | Disturbances of behaviour, emotion or thinking are occasionally noticeable. |
THREE | Distress is sometimes apparent, and/or the veteran’s pre-occupation with the symptoms is sometimes noticeable to astute observers or persons familiar with the veteran. |
SIX | Distress is apparent, and/or the veteran’s pre-occupation with the symptoms is noticeable to astute observers or persons familiar with the veteran. |
TEN | Obvious distress and pre-occupation with the symptoms is evident to casual observers and even persons unfamiliar with the veteran. |
FIFTEEN | Obvious continual distress. |
TWENTY | Distress that draws attention to the veteran. |
TWENTY- FOUR | All pervasive distress. |
| One rating is to be selected from this table for the manifest distress due to the accepted psychiatric condition being assessed. |
| | | |
Manifest distress is the manifestation of the distress that others observe in the veteran. It is the equivalent of the signs observed in a physical condition.
Examples include preoccupation, manic behaviour, inappropriate actions, restless pacing, nervous sweating, tremor, bursts of anger, pressured speech, perseveration, inability to follow a conversation, vocalisations during nightmares, compulsive or excessive drinking and compulsive gambling.
Functional Loss Table 4.3 | 
|
FUNCTIONAL EFFECTS | |
Impairment Ratings | General description and outcome |
NIL | Minimal or no interferences with most aspects of living. |
ONE | Minor interference with function in some everyday situations. |
TWO | Moderate interference with function in some everyday situations. |
THREE | Moderate interference with functions in many everyday situations. |
FIVE | Marked interference with function in many everyday situations. |
SIX | The veteran may be able to continue to function in everyday situations, but with gross restrictions. |
EIGHT | Profound psychiatric impairment. Virtually all recreational, social or otherwise purposeful activities abandoned. |
| One rating is to be selected from this table for the functional effects of the accepted psychiatric condition being assessed. |
| | | |
Functional effects are the effects of the condition on the veteran’s ability to function in a non-specific environment.
Relevant factors include the veteran’s ability to deal with personal hygiene, to prepare and consume food, to use electrical appliances, to find one’s way around, to return safely home after going to the shops etc, to avoid common dangers (such as in crossing the road), to remember the location and use of ordinary objects, the method of catching public transport etc.
Functional Loss Table 4.4 | 
|
OCCUPATION | |
Impairment Ratings | General description and outcome |
NIL | Minimal or no interference with work or occupation. |
ONE | Exacerbation of symptoms may cause occasional days off work. |
TWO | Short periods (more than one day at a time) of absence from work. |
THREE | Long periods (weeks or months) of absence from work. |
FIVE | An employed veteran will have major difficulties at work, which may be manifested by job modification or restriction of career opportunities. The disorder may contribute to the loss of a job. |
SIX | The veteran may be unable to work or may still be working, but with marked loss of time and/or loss of productivity at work leading to loss of original vocation. |
EIGHT | The veteran cannot work. |
| One rating is to be selected from this table for the occupational effects of the accepted psychiatric condition being assessed. |
| | | |
Occupation. This table relates to the effect of the psychiatric condition on the veteran’s ability to work.
Relevant factors include ability to concentrate on a task, ability to work with others, ability to take instructions from a supervisor and ability to interact appropriately with clients.
The criteria for gaining impairment ratings under Table 4.4 are different from the criteria of eligibility for benefits under sections 23, 24, and 25 of the Act. For purposes of applying Table 4.4, only the impairment from accepted psychiatric condition(s) of the veteran is to be taken into account.
Functional Loss Table 4.5 | 
|
DOMESTIC SITUATION | |
Impairment Ratings | General description and outcome |
NIL | Minimal or no effect on ordinary family life. |
ONE | Occasional friction with family members. |
TWO | Frequent discord with family members. |
THREE | Frequent conflict with family members. |
FIVE | Continual conflict with family members. |
SIX | Family functioning is deteriorating, and estrangement or divorce are a likely consequence. |
EIGHT | Virtually non-existent family life because of conflict with family members. |
| One rating is to be selected from this table for the domestic effects of the accepted psychiatric condition being assessed. |
| | | |
Domestic situation. This tables relates to the effect of the psychiatric condition on the veteran’s ability to continue or form domestic interpersonal relationships.
Relevant factors include the ability to maintain usual relationships with other family members and recognition of usual domestic relationships.
Functional Loss Table 4.6 | 
|
SOCIAL INTERACTION | |
Impairment Ratings | General description and outcome |
NIL | Minimal or no effect on ordinary social contacts. |
ONE | Occasional friction with colleagues and friends. |
TWO | Minor reduction in social interaction. |
THREE | Significant reduction in social interaction. |
FIVE | Substantial reduction in social interaction. |
SIX | General social withdrawal. |
EIGHT | Negligible social contact. |
| One rating is to be selected from this table for the social effects of the accepted psychiatric condition being assessed. |
| | | |
Social interaction. This table relates to the effect of the psychiatric condition on the veteran’s ability to continue or form interpersonal relationships with friends other than close family members and to interact with people in a casual way as required in social circumstances.
Relevant factors include ability to react appropriately to people in different roles; to follow the thread and purpose of a conversation; to restrict conversation to appropriate topics and to respond suitably to remarks.
Functional Loss Table 4.7 | 
|
LEISURE ACTIVITIES | |
Impairment Ratings | General description and outcome |
NIL | Minimal or no effect on leisure activities. |
ONE | Some loss of interest in activities previously enjoyed. |
TWO | Some reduction in recreational activities. |
THREE | Significant reduction in recreational activities. |
FIVE | Loss of interest in most recreational pursuits. |
SIX | Substantial reduction in most recreational pursuits. |
EIGHT | Virtually all recreational activities abandoned. |
| One rating is to be selected from this table for the recreational effects of the accepted psychiatric condition being assessed. |
| | | |
Leisure activities. This table relates to the effect of the psychiatric condition on the veteran’s ability to enjoy previously pleasurable activities.
Relevant factors include decreased ability to concentrate, decreased ability to understand complex activity (for example how to do crossword puzzles, how to play cards and sports, or to follow the plot of a movie or book), loss of interest in games and sports, perhaps even the inability to remember the purpose or rules of a game. (Inability to concentrate or remember may lead to embarrassment with avoidance of the activity.)
Functional Loss Table 4.8 | 
|
CURRENT THERAPY | |
Impairment Ratings | General description and outcome |
NIL | No regular treatment sought or recommended. |
ONE | Medical therapy or some supportive treatment from LMO may be required, and if not commenced, may be recognised as being of use. |
TWO | Psychiatric treatment, at least in the form of medication or psychotherapy, has been tried (or recommended), and/or some occasional supportive therapy given at an outpatient level or by an LMO or specialist and/or a friend or other person (eg a member of the clergy) has acted in a supportive role or as a sounding board. |
THREE | Psychiatric treatment, at least in the form of medication or psychotherapy, has been used (or deemed necessary), and/or periods of regular supportive therapy at an outpatient level or similar. |
FIVE | Need for intensive specialist psychiatric treatment on an outpatient basis, including medication and/or in-patient hospital care for short periods. |
SIX | Longer periods of in-patient hospital care are necessary. Long term psychotropic drug regimes or ECT is being undertaken. |
EIGHT | Continuous psychiatric treatment is essential, with a need for long periods in hospital and marked social support. |
| One rating is to be selected from this table for the treatment effects of the accepted psychiatric condition being assessed. |
| | | |
Current therapy is the treatment that is being given or has been recommended for the veteran’s psychiatric condition.
Such treatment includes but is not limited to medication such as hypnotics and sedatives, counselling, group therapy, hospitalisation, or ECT. The treatment may be administered or overseen by a psychiatrist, a general practitioner, a psychologist or other health workers. The term “therapy” also includes assistance to the veteran given by his or her spouse, or other close relatives, or friends, or clergy.
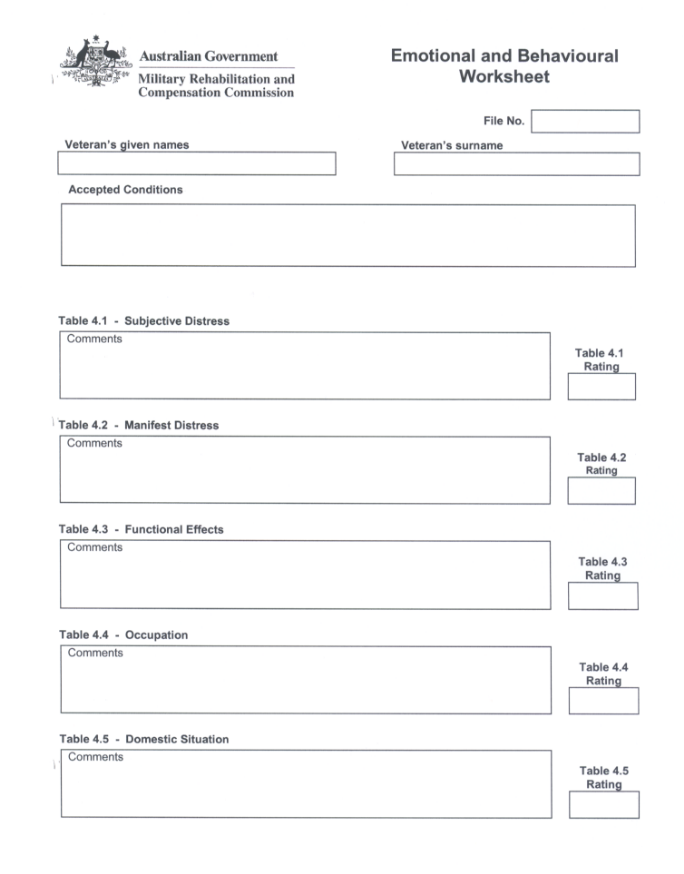
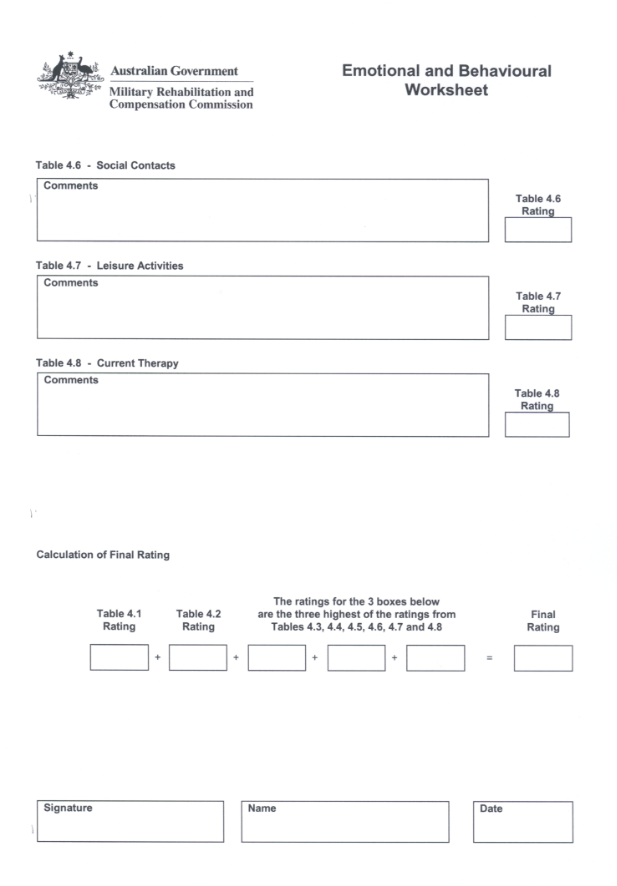
CHAPTER 5
NEUROLOGICAL IMPAIRMENT
INTRODUCTION
Loss of function tables (Tables 5.1–5.5)
Neurological impairment is measured by reference to multiple functions, many of which are rated using tables in other chapters. The additional functions considered in this chapter are:
- cognitive function (Table 5.1);
- communication (Tables 5.2 and 5.3); and
- sensory function (Table 5.4).
Ratings from one functional loss table are to be combined with ratings from any other table for a different loss of function from the same condition. Ratings from functional loss tables are not to be combined with ratings from Other Impairment tables for the same condition.
Other Impairment table (Table 5.6)
Table 5.6 lists specific impairment ratings for a variety of neurological conditions which are based on prognosis and, in some cases, pain. When ratings for the same condition can be made from Table 5.6 and a functional loss table, the higher rating is to be chosen.
Calculation of the impairment rating for an accepted neurological condition
Follow the steps below to determine the impairment rating for neurological conditions:
(Each step is elaborated in the following pages.)
STEP 1 | Determine an impairment rating for functional loss from the accepted neurological condition, by applying Tables 5.1, 5.2, 5.3, 5.4, and 5.5, as applicable. | Page 86 |
STEP 2 | Determine an impairment rating for functional loss from the accepted neurological condition, by applying other applicable chapters of this Guide. | Page 92 |
STEP 3 | Determine a rating for Other Impairment from the accepted neurological condition, by applying Table 5.6 as applicable. | Page 93 |
STEP 4 | (Omit this step if no rating was given in Step 3.) Combine the ratings obtained in Step 1 and Step 2, by applying Chapter 18 (Combined Values Chart). Compare the resultant combined rating with the rating obtained in Step 3. Take the higher rating. | Page 93 |
Step 1: Determine an impairment rating for functional loss from the accepted neurological condition, by applying Tables 5.1, 5.2, 5.3, 5.4, and 5.5, as applicable.
Cognitive function
“Cognition” means “the faculty of knowledge”. The cognitive function deals with such aspects of knowledge as acquisition (learning), retention and recall (memory), and use (reasoning and problem-solving).
Table 5.1 is applied only if an organic brain condition has been diagnosed. It is not to be applied to assess general mental capacity in a veteran with a condition of another body system unrelated to the brain condition. The impairment rating must relate only to cognitive deficits that were not present before the onset of the condition. Psychiatric conditions are to be assessed by applying Chapter 4 (Emotional and Behavioural).
Self-reports of deteriorating mental function must be interpreted with caution. Organic brain disease is often associated with a lack of insight or a tendency to deny failing abilities. Self-reported complaints about poor memory may be more closely related to depressive symptoms than to true memory deficits. If there is doubt about the nature or extent of the deficit, formal psychometric testing may be required.
Table 5.1 addresses memory and new learning ability as well as reasoning and problem-solving abilities. This requires:
- adequate levels of motivation and attention;
- restraint of impulsive tendencies;
- ability to organise, categorise and shift responses;
- use of feedback to modify behaviour; and
- capacity to evaluate final performance.
The ratings reflect increasing grades of severity.
Functional Loss Table 5.1 | 
|
LOSS OF NEUROLOGICAL FUNCTION: COGNITION |
Impairment Ratings | Criteria |
NIL | - Negligible impairment: reasoning is comparable with that of peers.
|
| - Memory similar to that of peers: written notes, etc., used in the manner of busy people of all ages.
|
TEN | - Mild impairment: appropriate use is made of accumulated knowledge and reasonable judgement is shown in routine daily activities most of the time. Difficulties are apparent in new circumstances.
- Mild but demonstrable impairment of memory: misplaces objects, and has increased difficulty in remembering names and appointments. Can learn, although at a slower rate than previously. Impairment has little impact on everyday activity because of compensation through reliance on written notes, schedules, checklists and spouse.
|
TWENTY- FIVE | - Moderate impairment of memory: has frequent difficulty in recalling details of recent experiences; frequently misplaces objects; fails to follow through with intentions or obligations; tends to get lost more easily in unfamiliar areas. Compensation through use of aids, eg. lists and diaries, is adequate.
- Moderate impairment of problem solving ability, relies on accumulated knowledge. Suffers significant disadvantage in circumstances requiring complex decision-making or non-routine activities, i.e. when past decision-making is not directly relevant. Has reduced initiative, spontaneity, and capacity for abstract thinking.
|
FORTY | Symptoms as above, but more frequent and severe. Is partially able to compensate, but unable to function with complete independence, and needs some supervision. |
SIXTY | - Severe impairment: has difficulty in carrying out basic activities such as sequencing the steps needed for dressing and for preparing meals.
- Planning/organisational ability is reduced. Is unable to function independently in new or complex situations. Shows markedly reduced initiative and spontaneity, and perseverative thinking.
- Severe memory deficiency: is unable to retain any information about recent experiences. New learning is not possible after attention has been directed elsewhere. Is unable to work or live independently, needing supervision to avoid harm, e.g. from fire caused by forgetting to put out cigarettes or to turn off appliances. Has extreme difficulty in keeping track of finances, scheduled activities, social relationships, etc.
|
SEVENTY | - Gross impairment: is unable to initiate and sustain activities without supervision. Supervision and prompting are required for virtually all daily activity. Is unable to plan a course of action for the simplest activity.
- Gross amnesic syndrome: is unable to acquire or recall new information. Constant supervision and care are required. Unable to recognise family, own reflection in mirror, etc. Is disoriented in familiar surroundings.
|
| | |
Communication
Communication has two elements: comprehension and expression. “Comprehension” means “understanding”. It includes understanding of speech and gestures, recognition of sights and sounds, spatial and temporal orientation. “Expression” is the capacity to convey the content of one’s mind to others.
Comprehension and expression are to be rated separately, by applying Tables 5.2 and 5.3 respectively. Impairment ratings from these tables are to be combined when criteria from both are applicable. Impairment ratings from these tables are not to include communication deficits that were present before the onset of the condition.
Tables 5.2 and 5.3 are to be applied to rate neurological or neuromuscular conditions as well as local lesions involving the mechanisms of speech production. Communication may also be restricted by vision loss, hearing loss, or loss of hand function. Ratings are then to be made from Chapter 8, Chapter 7, or Chapter 3 respectively, instead of Tables 5.2 and 5.3.
Comprehension
Table 5.2 is to be applied to rate limitation of auditory or visual comprehension. Only one impairment rating is to be given from this table. If more than one criterion is applicable that which results in the higher rating is to be chosen.
Expression
Table 5.3 is to be applied to rate limitation of speech production, as well as written and unspoken methods of expression. Only one impairment rating is to be made from this table. If more than one criterion is applicable, that which results in the higher rating is to be chosen.
Evaluation of speech production takes into account:
- audibility: the ability to speak loudly enough to be heard;
- intelligibility: the ability to articulate and to link phonetic units of speech with sufficient accuracy to be understood;
- functional efficiency: the ability to speak quickly enough, and to sustain the rate for a period; and
- retrieval and manipulation of language elements: expression of ideas.
Functional Loss Table 5.2 | 
|
LOSS OF NEUROLOGICAL FUNCTION: COMPREHENSION |
Impairment Ratings | Criteria |
NIL | Normal or nearly normal comprehension. |
FIVE | Can understand movies, radio programs or group discussions, but with some difficulty. Comprehension is good in most situations, but understanding is difficult in large groups, or when tired and upset. Has difficulty coping with rapid changes of topic. |
TEN | - Can understand speech face-to-face, but confusion or fatigue occurs rapidly in any group. Is unable to cope with rapid change in topic, or with complex topics: is able to grasp the meaning of TV serials, but not more complex ideas.
- Mild dyslexia: is able to grasp the meaning of basic newspaper and magazine articles, but has difficulty understanding details. Is unable to follow the storyline in books.
|
TWENTY- FIVE | - Can understand only simple sentences, and follow simple conversion when some points are repeated
- Moderate dyslexia: reading comprehension is limited to sentences and short paragraphs. Can follow simple two-to-three line instructions, and cope with shopping (and other) lists, but nothing more complex.
|
FORTY | - Can understand only single words. Shows some understanding of slowly-spoken simple sentences from context and gesture, although frequent repetition is needed.
- Severe dyslexia: is able to read single words, to match words to pictures and to read labels and signs, but is unable to read instructions.
|
FIFTY | - Unable to understand simple instructions or yes/no questions, even with gesture.
- Unable to read single words, labels or signs.
|
| Ratings from one Functional Loss table may be combined with ratings from any other table for a different loss of function. Ratings from Functional Loss tables are not to be combined with ratings from Other Impairment tables for the same condition. |
| | |
Functional Loss Table 5.3 | 
|
LOSS OF NEUROLOGICAL FUNCTION: EXPRESSION |
Impairment Ratings | Criteria |
NIL | Normal or nearly normal expression. |
FIVE | Speech is of sufficient intensity and vocal quality for most everyday needs, eg: normal speech, but unable to shout; or needs to repeat self at times; or is unable to produce some phonetic units; or speech is sustained over a 10-minute period, but with difficulty that includes hesitation and word-retrieval problems; or is permanently hoarse. |
TEN | - Speech is of sufficient intensity and vocal quality for many of the needs of everyday speech, eg:
is adequate with low background noise, but is heard with some difficulty in vehicles or public places; or has many inaccuracies, but is easily understood by strangers; or is slow or discontinuous, conveying the distinct impression of difficulty. - Converses in simple sentences on familiar topics, although word-finding problems are frequent, and has difficulty in explaining long or complex ideas.
- Has mild dysgraphia: is unable to cope with more than short letters (about five lines) or postcards, which show both grammatical and spelling errors.
|
TWENTY | - Speech is of sufficient intensity and vocal quality for some of the needs of everyday speech, eg:
is adequate under quiet conditions, but is heard with great difficulty against any background noise; voice fades rapidly; or is understood by family and friends, but is difficult for strangers; or needs frequent repetition; or speech is sustained for short period only: fatigues rapidly. - Has moderate dysgraphia: is unable to write more than short sentences which include frequent spelling errors, eg. has difficulty filling in bank forms.
|
THIRTY | - Speech is of sufficient intensity and vocal quality for only a few of the needs of everyday speech, eg:
is reduced to a whisper at best: inaudible over the telephone; or can produce only a few phonetic units approximating some words, but these are not intelligible if the context is unknown; or can produce only short phrases or single words: speech flow is not maintained, or is too slow to be useful. - Is unable to initiate conversation, but, with considerable effort, is able to respond in short simple sentences or phrases.
- Has severe dysgraphia: is able to write only some recognisable words, eg: items for a shopping list, or names of family.
|
FORTY | - Has no speech production, but is able to use non-verbal means of expression.
- Is limited to single words or familiar social or stereotyped phrases requiring considerable listener inference.
- Has agraphia: no functional writing ability, although is able to copy or write much-practiced sequences, such as own name.
|
| Ratings from one Functional Loss table may be combined with ratings from any other table for a different loss of function. Ratings from Functional Loss tables are not to be combined with ratings from Other Impairment tables for the same condition. |
| | |
“Total Loss of Speech” is also mentioned in Table 24.1 (Degree of Incapacity for Specific Disabilities) in Chapter 24.
Sensory function
Table 5.4 is to be applied to rate sensory loss only. Lesions of nerves or nerve roots may also cause motor loss, which is to be rated independently by applying Chapter 3. Ratings may be made for sensory loss in the distribution of either a dermatome or a peripheral nerve, but not both for the same loss.
“Partial loss” refers either to a loss of less than the complete distribution of the nerve, or to altered sensation. Peripheral neuropathies with a “glove and stocking distribution” and “happy feet” are examples of this.
Functional Loss Table 5.4 | 
|
LOSS OF NEUROLOGICAL FUNCTION: SENSORY NERVES |
| | Impairment Ratings | | |
| Partial Unilateral Loss | Total Unilateral or Partial Bilateral Loss | Total Bilateral Loss | |
Dermatome | | | | |
C2-3 (together) | 0 | 5 | 10 | |
C6&7 (together) | 5 | 10 | 20 | |
C8 | 0 | 5 | 10 | |
L5&S1 (together) | 0 | 5 | 10 | |
S2&3&4 (together) | 0 | 5 | 10 | |
Hemianaesthesia (central) | 15 | 30 | — | |
Peripheral Nerve | | | | |
Greater auricular | 0 | 5 | 10 | |
Median | 5 | 10 | 20 | |
Ulnar | 0 | 5 | 10 | |
Radial | 0 | 0 | 0 | |
Posterior femoral cutaneous | 0 | 5 | 10 | |
Sciatic | 0 | 5 | 10 | |
Tibial (medial popliteal) | 0 | 5 | 10 | |
Pudendal | 0 | 5 | 10 | |
| | | | | |
Ratings from one Functional Loss table may be combined with ratings from any other table for a different loss of function. Ratings from Functional Loss tables are not to be combined with ratings from Other Impairment tables for the same condition.
Cranial nerves
Although related anatomically, cranial nerves represent diverse functions which are to be rated elsewhere in most cases. Sometimes no alternative tables exist, and a rating relating to loss of motor or sensory function is given.
Ratings from Table 5.5 can be combined with ratings from other tables relating to neurological function, but not with ratings from Table 5.6 for the same condition. The ratings listed are for complete loss of function. If partial losses exist the ratings are to be reduced proportionately.
Functional Loss Table 5.5 | 
|
LOSS OF NEUROLOGICAL FUNCTION: CRANIAL NERVES |
Cranial Nerve | Function | Assessment to be made by application of: | Complete Unilateral Loss | Complete Bilateral Loss |
I | Smell | | 0 | 5 |
II | Vision | Chapter 8 | | |
III, IV, VI | Eye movement | Chapter 8 | | |
V Trigeminal (sensory) | Ophthalmic | | | |
| division | | 5 | 10 |
| Maxillary | | | |
| division | | 5 | 10 |
| Mandibular | | | |
| division | | 5 | 10 |
| Chewing | Chapter 6 | | |
| Speech | Table 5.3 | | |
VII | Taste | | 0 | 5 |
| Facial expression | | 10 | 20 |
| Chewing | Chapter 6 | | |
| Speech | Table 5.3 | | |
VIII | Hearing | Chapter 7 | | |
| Balance | Chapters 15 or 16 | | |
IX, X, XI, XII | Swallowing | Chapter 6 | | |
| Speech | Table 5.3 | | |
XI | Shoulder Elevation | | 5 | 10 |
| | | | | |
Ratings from one Functional Loss table may be combined with ratings from any other table for a different loss of function. Ratings from Functional Loss tables are not to be combined with ratings from Other Impairment tables for the same condition.
Step 2: Determine an impairment rating for functional loss from the accepted neurological condition, by applying other applicable chapters of this Guide.
Assessment of conditions of the central and peripheral nervous system may require the application of tables from Chapter 3 (upper and lower limb function), Chapter 6 (eating and swallowing, faecal continence), Chapter 7 (hearing), Chapter 8 (vision), Chapter 9 (urinary continence), and Chapter 10 (sexual function). A neurological rating may involve the combination of multiple ratings, each relating to the loss of a different function. Cerebrovascular accidents, for example, may require ratings for hemiparesis of the upper limb, hemiparesis of the lower limb, hemianopia and dysphasia.
Step 3: Determine a rating for Other Impairment from the accepted neurological condition, by applying Table 5.6 as applicable.
Neurological Other Impairment
Most neurological conditions are associated with a readily identifiable functional deficit. Table 5.6 is to be applied to rate those conditions where such deficit is minimal, and yet a significant neurological condition exists. Many of the conditions referred to in Table 5.6 may result in significant loss of function. Ratings from Table 5.6 and the functional loss table are to be compared, and the higher rating is to be chosen.
Functional Loss Table 5.6 | 
|
NEUROLOGICAL OTHER IMPAIRMENT |
Impairment Ratings | Criteria |
NIL | - Headaches of any type, infrequent and easily controlled.
- History of epilepsy no longer necessitating medication.
|
FIVE | - Documented cerebrovascular disease, eg. history of transient ischaemic attacks; cerebrovascular accident with good return of function; pathological narrowing of arteries demonstrated with Doppler studies or angiography (but not calcification shown on plain X-ray).
- Aneurysms (not surgically corrected).
- Tics, hemifacial spasm.
- Epilepsy requiring daily medication.
|
TEN | - Progressively deteriorating neurological disorders associated with significantly reduced life expectancy, eg. multiple sclerosis, Alzheimer’s disease.
- Tic douloureux occurs intermittently.
|
TWENTY | - Rapidly progressive neurological disorders associated with significantly reduced life expectancy, eg. motor neurone disease.
- Tic douloureux occurs frequently.
|
| Ratings from this table and the Functional Loss table are to be compared and the higher rating is to be chosen — see Step 4. |
| | |
Chapter 15 (Intermittent Impairment) may be applied to rate cases with more frequent or severe episodes.
Step 4: (Omit this step if no rating was given in Step 3.) Combine the ratings obtained in Steps 1 and 2, by applying Chapter 18 (Combined Values Chart). Compare the resultant rating with the rating obtained in Step 3. Take the higher. This is the final impairment rating for the accepted neurological condition.
CHAPTER 6
GASTROINTESTINAL IMPAIRMENT
This chapter consists of 2 parts:
Part 6.1 — Diseases of the digestive system
Part 6.2 — Abdominal wall hernias and obesity
PART 6.1: DISEASES OF THE DIGESTIVE SYSTEM
Diseases of the digestive system include conditions of the alimentary tract and of the accessory organs of digestion: liver, pancreas and gall bladder.
Loss of function (Tables 6.1.1, 6.1.2 and 6.1.3)
Gastrointestinal impairment is measured by loss of the abilities to ingest food, to maintain nutrition and to excrete the waste products of digestion. Impairment of these functions will be manifested by:
- difficulty in chewing and swallowing;
- nutritional deficiency and loss of weight; and
- faecal incontinence or constipation.
Impairment of each function is to be rated independently of the others. Separate ratings are to be given for each affected function.
If the gastrointestinal loss of function is due to a malignant condition, the step-by-step instructions in Chapter 14 (Malignant Conditions) are to be followed.
If the gastrointestinal loss of function is intermittent in nature or has a significant intermittent component, Chapter 15 (Intermittent Impairment) is to be applied.
If the gastrointestinal loss of function is very severe or causes marked debility, Chapter 16 (Activities of Daily Living) is to be applied.
In particular, severely impaired liver function is to be rated by reference to Chapter 16 (Activities of Daily Living).
Other Impairment (Tables 6.1.4 to 6.1.12)
Tables 6.1.4 to 6.1.12 give specific impairment ratings for various gastrointestinal conditions, based largely on the presence of symptoms. Each of the nine tables refers to a different region or aspect of the gastrointestinal tract or to one of the associated organs of digestion. If, for the same gastro-intestinal condition, ratings can be given both from one of the Functional Loss tables and from a gastrointestinal Other Impairment table, the higher rating is to be chosen.
If multiple accepted conditions contribute to any of the ratings obtained from any of Tables 6.1.1, 6.1.2 or 6.1.3, Chapter 20 (Apportionment) is to be applied as required before making any comparison with a rating from one of the gastrointestinal Other Impairment tables.
Calculation of the impairment rating for gastrointestinal conditions
Follow the steps below to calculate the impairment due to accepted gastrointestinal conditions.
(Each step is elaborated in the following pages.)
STEP 1 | Determine one or more ratings for loss of gastrointestinal function. | Page 95 |
STEP 2 | Determine any Other Impairment ratings that are applicable. | Page 98 |
STEP 3 | Compare the functional impairment rating with the relevant Other Impairment rating. Take the higher rating. | Page 102 |
Step 1: Determine one or more ratings for loss of gastrointestinal function.
There are three tables relating to gastrointestinal functional loss:
| Loss of gastrointestinal function: ingestion of food |
| Loss of gastrointestinal function: maintenance of nutrition |
| Loss of gastrointestinal function: faecal excretion |
A gastrointestinal condition may cause a loss of function under more than one of the above tables. In that case a rating is to be selected from each applicable table.
If more than one condition is present, a rating is to be selected from each of the applicable tables. However, only one rating is to be selected from each table irrespective of the number of conditions that contribute to the functional impairment that is being assessed by applying that table.
If a non-accepted condition or non-accepted conditions contribute to the rating selected from a table, Chapter 19 (Partially Contributing Impairment) is to be applied.
Functional Loss Table 6.1.1 | 
|
LOSS OF GASTROINTESTINAL FUNCTION: INGESTION OF FOOD |
Impairment Ratings | Criteria |
NIL | Some difficulty in chewing or swallowing, but only minor or occasional restriction of diet and there is no weight loss. |
FIVE | Significant difficulty in chewing or swallowing, but diet is not grossly restricted and there is no weight loss. |
TEN | - Difficulty in chewing or swallowing that limits diet to soft or semi-solid foods.
- Constant dysphagia requiring dilation two or three times a year.
|
TWENTY | Diet limited to liquid or to pureed food because of difficulty in chewing or swallowing. |
THIRTY | Constant dysphagia necessitating dilation six times or more a year. |
| Only one rating is to be selected from this table for any condition or combination of conditions. |
| | |
To calculate the percentage loss of weight for the purposes of Table 6.1.2 follow the substeps below.
Substep 1A | Determine the veteran’s weight before the beginning of the gastro-intestinal condition (irrespective of when the condition was first diagnosed or accepted). This is the “premorbid weight”. |
Substep 1B | Determine the veteran’s weight at the relevant time in the assessment period. |
Substep 1C | If the weight obtained in substep 1B is equal to, or greater than, the premorbid weight, no impairment rating based on involuntary weight loss can be given from Table 6.1.2. If the weight obtained in substep 1B is less than the premorbid weight, express the difference as a percentage of the premorbid weight. The result is the “percentage loss of weight”. |
Substep 1D | Determine whether the percentage loss of weight is due to the accepted gastrointestinal condition being assessed. If it is, then the percentage loss of weight may be used in applying Table 6.1.2. If the percentage loss of weight is not due to the accepted gastro-intestinal condition being assessed, then no impairment rating based on involuntary loss of weight can be given from Table 6.1.2. |
Substep 1E | If non-accepted conditions contribute to the percentage loss of weight, Chapter 19 (Partially Contributing Impairment) is to be applied. |
Functional Loss Table 6.1.2 | 
|
LOSS OF GASTROINTESTINAL FUNCTION: MAINTENANCE OF NUTRITION |
Impairment Ratings | Criteria |
NIL | Minor or no modification to diet, eg. high fibre diet or necessity to avoid certain foodstuffs. |
TWO | Malabsorption well controlled with appropriate replacement therapy. |
FIVE | - Prescribed exclusion diet or major dietary restrictions, eg. gluten-free diet.
- Laboratory evidence of malabsorption or nutritional deficiency despite therapy (including dietary restriction), but no signs or symptoms.
|
TEN | Laboratory evidence of malabsorption together with some signs or symptoms. |
TWENTY | Involuntary weight loss of 10% or more with evidence of active disease and minor symptoms only. |
THIRTY | Involuntary weight loss of 10% or more with evidence of active disease and associated with local symptoms or mild systemic symptoms. |
FORTY | - Involuntary weight loss of 20% or more with evidence of active disease.
- Ileostomy, jejunostomy, oesophagostomy or gastrostomy.
|
SIXTY | Involuntary weight loss of 20% or more with evidence of active disease and associated with severe, frequent local symptoms and systemic symptoms, eg. fever, malaise, anaemia. |
| Only one rating is to be selected from this table for any condition or combination of conditions. |
| | |
Functional Loss Table 6.1.3 | 
|
LOSS OF GASTROINTESTINAL FUNCTION: FAECAL EXCRETION |
Impairment Ratings | Criteria |
NIL | |
TWO | Persistent constipation. |
FIVE | Minor faecal incontinence associated with occasional soiling. |
TEN | Faecal soiling necessitating frequent changes of underwear, or a precautionary incontinence pad. |
TWENTY | Faecal incontinence necessitating use of incontinence pads on most days. |
THIRTY | - Faecal incontinence necessitating several changes of incontinence pads on most days.
- Colostomy.
|
FIFTY | Complete faecal incontinence. |
| Only one rating is to be selected from this table. |
| | |
Step 2: Determine any Other Impairment ratings that are applicable.
Determine which of the Other Impairment tables apply to the accepted gastrointestinal condition and select the appropriate impairment rating from each.
There are nine gastrointestinal Other Impairment tables:
| Oral cavity and oesophagus |
| Non-ulcer dyspepsia, nausea and vomiting |
| Peptic ulcers: duodenal or gastric ulcers |
| Effects of past gastric surgery |
| Disorders of the large and small bowel |
| Disorders of the anus and rectum |
| Liver |
| Pancreas |
| Gall bladder |
A gastrointestinal condition may attract an Other Impairment rating under more than one of the above tables. In that case a rating is to be selected from each applicable table.
Only one impairment rating is to be selected from each of the gastrointestinal Other Impairment tables for each condition or combination of conditions. If more than one rating from any table is applicable, the higher or highest rating is to be selected.
Other Impairment Table 6.1.4 | 
|
ORAL CAVITY AND OESOPHAGUS |
Impairment Ratings | Criteria |
NIL | - Oral disorders causing no problems or minimal difficulties in chewing.
- Asymptomatic hiatus hernia.
- Halitosis.
|
TWO | Reflux, mild or occasional symptoms with or without prophylactic treatment. |
FIVE | Reflux, with or without oesophagitis: frequent minor symptoms necessitating frequent use of antacids or use of H2 receptor antagonist medication. |
TEN | Oesophagitis: active disease with moderate symptoms on most days, despite regular use of H2 receptor antagonist medication. |
TWENTY | Oesophagitis, proven endoscopically: active disease with complications, eg. Barrett’s epithelium, blood loss, aspiration or stricture. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
Other Impairment Table 6.1.5 | 
|
NON-ULCER DYSPEPSIA, NAUSEA AND VOMITING |
Impairment Ratings | Criteria |
NIL | Non-ulcer dyspepsia, nausea or vomiting: infrequent and mild. |
FIVE | Non-ulcer dyspepsia, nausea or vomiting: mild to moderate, necessitating some medication on most days. |
TEN | Non-ulcer dyspepsia, nausea or vomiting: moderate symptoms, necessitating daily full-dose medication. |
TWENTY | Non-ulcer dyspepsia or vomiting: severe, not controlled despite medication, and causing weight loss of 10% or more. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
Other Impairment Table 6.1.6 | 
|
PEPTIC ULCERS: DUODENAL OR GASTRIC ULCERS |
Impairment Ratings | Criteria |
NIL | Past history of peptic ulcer: currently inactive and asymptomatic, with or without maintenance treatment. |
FIVE | Peptic ulcer: with intermittent symptoms necessitating ongoing maintenance treatment. |
TEN | Peptic ulcer: active disease with moderate symptoms on most days, despite regular H2 receptor antagonist or proton pump inhibitor medication. |
TWENTY | Peptic ulcer: proven endoscopically: active disease with complications and troublesome daily symptoms, eg. bleeding or outlet obstruction. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
For a gastric ulcer that has been surgically removed apply Table 6.1.7.
Other Impairment Table 6.1.7 | 
|
EFFECTS OF PAST GASTRIC SURGERY |
Impairment Ratings | Criteria |
NIL | Past gastric surgery, currently asymptomatic. |
FIVE | Past gastric surgery with intermittent dyspepsia and/or mild dumping syndrome. |
TEN | Past gastric surgery with frequent dyspepsia and/or dumping syndrome. |
TWENTY | Past gastric surgery with severe dyspepsia and/or dumping syndrome on most days. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
Severe cases of dumping syndrome may be rated by applying Chapter 15 (Intermittent Impairment).
Other Impairment Table 6.1.8 | 
|
DISORDERS OF THE LARGE AND SMALL BOWEL |
Impairment Ratings | Criteria |
NIL | Bowel disorder, eg. irritable bowel, diverticulosis: infrequent and minor symptoms such as constipation, or intermittent diarrhoea and abdominal cramps which respond to dietary treatment. |
FIVE | Bowel disorder: frequent moderate symptoms necessitating regular medication. |
TEN | Bowel disorder: marked symptoms, such as regular diarrhoea and frequent abdominal pain, partially controlled by full-dose medication. |
TWENTY | Bowel disorder: diarrhoea and abdominal pain on most days, with no response to medication and considerable interference with daily routine. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
Other Impairment Table 6.1.9 | 
|
DISORDERS OF THE ANUS AND RECTUM |
Impairment Ratings | Criteria |
NIL | - Anal disorder: infrequent and minor symptoms, eg. haemorrhoids, anal fissures, controlled by medication.
- Mild to moderate pruritus ani.
|
FIVE | - Anal disorder: moderate symptoms on most days, necessitating regular medication for control.
- Marked pruritus ani, with daily symptoms and evidence of excoriation.
|
TEN | Anal disorder: marked to severe symptoms despite regular treatment. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
Other Impairment Table 6.1.10 | 
|
LIVER |
Impairment Ratings | Criteria |
NIL | - Abnormality of liver function tests, but otherwise asymptomatic.
- Acute hepatitis (resolved).
|
TWO | Chronic persistent hepatitis. |
FIVE | Signs of chronic liver disease, but no evidence of portal hypertension. |
TEN | - Chronic liver disease with evidence of portal hypertension.
- Chronic active hepatitis.
|
TWENTY | Chronic liver disease with history of variceal bleeding or encephalopathy. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
Other Impairment Table 6.1.11 | 
|
PANCREAS |
Impairment Ratings | Criteria |
NIL | Pancreatic disease, with no symptoms. |
TWO | Pancreatic disease, with mild infrequent symptoms. |
TEN | Chronic pancreatitis with ongoing intermittent attacks of abdominal pain and/or steatorrhoea. |
TWENTY | Chronic pancreatitis with frequent attacks of abdominal pain and steatorrhoea, or two or more admissions to hospital within the past year. |
| | |
More frequent exacerbations of pancreatic disease can be rated by applying Chapter 15 (Intermittent Impairment).
Other Impairment Table 6.1.12 | 
|
GALL-BLADDER |
Impairment Ratings | Criteria |
NIL | - Gall-bladder disease with no symptoms.
- Cholecystectomy currently asymptomatic.
|
TWO | Gall-bladder disease with mild infrequent symptoms. |
FIVE | - Post-cholecystectomy syndrome.
- Two or more attacks of gall-bladder disease necessitating hospital admission within the past year.
|
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
More frequent exacerbations of gall bladder disease can be rated by applying Chapter 15 (Intermittent Impairment).
Step 3: Compare the functional impairment rating with the relevant Other Impairment rating. Take the higher rating.
This step determines the final impairment rating for the gastrointestinal condition. Select one of the following substeps depending on the circumstances:
Substep 3A | If, for any condition, only one rating has been obtained in Step 1 and only one rating has been obtained in Step 2, compare the ratings. Take the higher rating. This is the final rating for that gastrointestinal condition. |
Substep 3B | If, for any condition, only one rating has been obtained in Step 1 but more than one rating has been obtained in Step 2, combine the ratings for that condition obtained in Step 2 using Chapter 18 (Combined Values Chart). Compare the rating for that condition obtained in Step 1 with the combined value of the ratings for that condition obtained in Step 2. Take the higher rating. This is the final rating for that gastrointestinal condition. For the purpose of the final combining of all values, if the higher value is made up of a combination of ratings, then the component ratings are to be used. |
Substep 3C | If, for any condition, more than one rating has been obtained in Step 1 but only one rating has been obtained in Step 2, combine the ratings for that condition obtained in Step 1 by applying Chapter 18 (Combined Values Chart). Compare the combined value of the ratings for that condition obtained in Step 1 with the rating obtained in Step 2. Take the higher rating. This is the final rating for that gastrointestinal condition. For the purpose of the final combining of all values, if the higher value is made up of a combination of ratings, then the component ratings are to be used. |
Substep 3D | If, for any condition, more than one rating has been obtained in Step 1 and more than one rating has been obtained in Step 2, combine the ratings for that condition obtained in Step 1 by applying Chapter 18 (Combined Values Chart) and separately combine the ratings for that condition obtained in Step 2 by applying Chapter 18 (Combined Values Chart). Compare the combined value of the ratings for that condition obtained in Step 1 with the combined value of the ratings for that condition obtained in Step 2. Take the higher rating. This is the final rating for that gastrointestinal condition. For the purpose of the final combining of all values, if the higher value is made up of a combination of ratings, then the component ratings are to be applied. |
PART 6.2: ABDOMINAL WALL HERNIAS AND OBESITY
Impairment ratings obtained from Tables 6.2.1 and 6.2.2 are not to be compared with any other tables but are to be included in the final combining of all ratings.
Functional Loss Table 6.2.1 | 
|
ABDOMINAL WALL HERNIAS |
Impairment Ratings | Criteria |
NIL | Inguinal or ventral hernia surgically repaired. |
TWO | Inguinal or ventral hernia easily reducible. |
FIVE | Inguinal or ventral hernia not easily reduced and resulting in mild symptoms. |
TEN | Large inguinal or ventral hernia resulting in frequent symptoms. |
| An impairment rating is to be selected from this table for each accepted inguinal and ventral hernia. |
| | |
Functional Loss Table 6.2.2 | 
|
OBESITY |
Impairment Ratings | Criteria |
NIL | Body mass index equal to or below 30. |
FIVE | Body mass index above 30. |
| | |
Body mass index is given by the formula:
Body mass index | = | (weight in kg) (height in m)2 |
Table 6.2.2 is to be applied only if obesity is an accepted condition or if obesity is an integral feature of an accepted condition.
CHAPTER 7
EAR, NOSE, AND THROAT IMPAIRMENT
This chapter contains two parts:
Part 7.1 — Hearing Loss and Tinnitus
Part 7.2 — Ear, Nose, and Throat
PART 7.1: HEARING LOSS AND TINNITUS
Because it causes a single loss of function, accepted hearing loss is to be assessed as if it were a single condition even if the loss is described under several diagnostic terms. For example, a veteran who has accepted conditions of both “right conductive deafness” and “left conductive deafness” will have them rated as if the conditions had been described as “bilateral conductive deafness”.
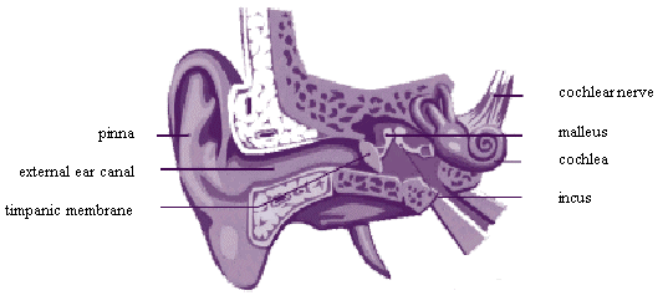
Only a single impairment rating may be made from Part 7.1 for accepted hearing loss irrespective of how many diagnostic terms have been used in describing the hearing loss.
However, a second impairment rating may be made from Part 7.1 (Table 7.1.11) for tinnitus if appropriate.
Definitions
For the purposes of this chapter:
“Air Conduction” | is the manner in which sound transmitted through the air reaches the inner ear in the normal way. |
“APHL” or “Accepted Percentage Hearing Loss” | is the percentage of total hearing that the veteran has lost due to accepted deafness. It is found by summing the losses at each of 6 important frequencies. |
“Bone conduction” | is the manner in which sound is heard when the source of sound is placed directly over any bony part of the hearer’s cranium. In such a case the sound is conducted to the inner ear through the bones of the skull. |
“HTL” or “Hearing Threshold Level” | is, for any given frequency, the volume (loudness) of the faintest sound that the veteran can hear. For each frequency, there will be a hearing threshold level for the right ear and a hearing threshold level for the left ear. Hearing threshold levels can be determined using either bone or air conduction information. |
“Presbyacusis” | is the normal loss of hearing which accompanies ageing. |
“TBHL” or “Total Bilateral Hearing Loss” | is the percentage of total hearing which the veteran has lost from all conditions whether accepted or not. |
Calculation of the impairment rating for accepted hearing loss
Follow the steps below to calculate the accepted hearing loss.
(Each of these steps is elaborated in the following pages.)
STEP 1 | Apply Table 7.1.1 to determine the type of accepted hearing loss. | Page 107 |
STEP 2 | Determine whether the audiogram is reliable and suitable for hearing loss calculations. | Page 108 |
STEP 3 | Calculate the APHL. | Page 109 |
STEP 4 | Determine what age adjustment (if any) must be subtracted from the APHL. Subtract it. | Page 120 |
STEP 5 | Determine the functional impairment rating by applying Formula 7.1. If the paired organs policy does not apply, this will be the final impairment rating for loss of hearing. | Page 122 |
STEP 6 | Determine if the paired organs policy applies by applying Table 7.1.10. If the policy applies, calculate the adjusted impairment rating. | Page 122 |
Hearing Worksheets
A set of Hearing Worksheets, at the end of this chapter (pages 127 to 131), is designed to facilitate the calculation of impairment due to accepted hearing loss. When performing a hearing loss assessment, the assessor should use the appropriate worksheet.
These worksheets may also be of assistance in gaining an understanding of the procedures set out in this chapter.
Step 1: Use Table 7.1.1 to determine the type of accepted hearing loss.
For the purpose of assessment, every type of accepted hearing loss is considered to consist of one or more of the following four components:
- right sensorineural deafness;
- left sensorineural deafness;
- right conductive deafness; and
- left conductive deafness.
Fifteen different types of accepted hearing loss are recognised. Each consists of one or more of the above four components. The 15 types of possible accepted hearing loss are listed in Table 7.1.1 below. Every accepted hearing loss or combination of hearing losses will be found to be equivalent to one of the types of hearing loss listed in Table 7.1.1.
Procedural Table 7.1.1 | 
|
TYPES OF ACCEPTED HEARING LOSS |
Type 1 | Bilateral mixed deafness |
Type 2 | Right mixed deafness |
Type 3 | Left mixed deafness |
Type 4 | Bilateral sensorineural deafness |
Type 5 | Bilateral sensorineural deafness with right conductive deafness |
Type 6 | Bilateral sensorineural deafness with left conductive deafness |
Type 7 | Bilateral conductive deafness |
Type 8 | Bilateral conductive deafness with right sensorineural deafness |
Type 9 | Bilateral conductive deafness with left sensorineural deafness |
Type 10 | Left conductive deafness with right sensorineural deafness |
Type 11 | Right conductive deafness with left sensorineural deafness |
Type 12 | Right conductive deafness |
Type 13 | Right sensorineural deafness |
Type 14 | Left sensorineural deafness |
Type 15 | Left conductive deafness |
| A single selection to cover the veteran’s accepted hearing loss is to be made from this table, ignoring the non-accepted hearing losses at this stage. |
| | |
Step 2: Determine whether the audiogram is reliable and suitable for hearing loss calculations.
The audiogram
Assessment of hearing impairment requires a pure tone audiogram. For the purposes of assessment of impairment, hearing loss is to be measured without the benefit of any hearing aid. Measurements of the hearing threshold level (HTL) should be taken at each of the following frequencies:
500 Hz, 1000 Hz, 1500 Hz, 2000 Hz, 3000 Hz, and 4000 Hz
Ideally, the audiogram should include both air conduction HTLs and masked bone conduction HTLs at each of these frequencies.
The four criteria for a reliable audiogram
1. The date of the audiogram must be appropriate to the period of assessment.
The audiogram should not be more than six months older than the relevant time in the assessment period to which the information is to be applied. If there is a specific assertion that the veteran’s hearing has deteriorated within the last six months, then the audiogram should not be more than six weeks old at the time of assessment.
2. The frequencies tested should be appropriate.
Measurements of HTL should be available for each of the frequencies mentioned above (that is, 500 Hz, 1000 Hz, 1500 Hz, 2000 Hz, 3000 Hz, and 4000 Hz).
If HTL measurements are missing at one or two frequencies, the missing values can be estimated (interpolation) by inspection of the audiogram, by applying knowledge of the type of hearing loss, and by examination of other audiograms. If the nature and extent of missing information in an audiogram are considered to be such that interpolation would not be sufficiently accurate, the audiogram should be repeated. If the deficient audiogram is recent, the new audiogram is to be used in its place. The new audiogram may also be used to assist in interpolation of an older, deficient audiogram.
3. Bone conduction HTLs should be available when necessary.
An audiogram showing both bone conduction and air conduction HTLs should be used for the assessment of all types of accepted hearing loss unless the total accepted hearing loss is equivalent to:
- Bilateral mixed deafness;
- Right mixed deafness;
- Left mixed deafness;
- Bilateral conductive deafness with right sensorineural deafness; or
- Bilateral conductive deafness with left sensorineural deafness,
for each of which only air conduction HTLs are required; or unless it is not practicable or appropriate to obtain bone conduction HTL values.
Reasons why it may not be practicable or appropriate to obtain bone conduction HTL values include the following:
- the veteran cannot reasonably attend a clinic where bone conduction HTL values can be measured;
- the veteran’s other conditions are of such a degree that it will make no appreciable difference to the final assessment; or
- an ENT specialist or an audiologist has reported that:
no air-bone gap is present;
no conductive hearing loss is present; or
Rinné’s test is positive.
In such circumstances only air conduction HTLs need to be obtained.
4. The nature of the audiogram should be appropriate.
The nature (that is, general shape) of the audiogram should be consistent with the known hearing loss affecting the veteran and should also be consistent with other information (eg, old audiograms) concerning the veteran.
If the nature of the audiogram is not appropriate, the audiogram should be repeated or the veteran referred to an ENT specialist to clarify the situation.
Step 3: Calculate the APHL.
There are six scales labelled 7.1.3 to 7.1.8. Each scale corresponds to a different frequency of sound. Table 7.1.3 relates to 500 Hz, Table 7.1.4 relates to 1000 Hz, Table 7.1.5 relates to 1500 Hz, and so on according to their labels.
Look up HTLs for 500Hz in Table 7.1.3 to give the loss at 500 Hz.
Look up HTLs for 1000Hz in Table 7.1.4 to give the loss at 1000 Hz
Look up HTLs for 1500Hz in Table 7.1.5 to give the loss at 1500 Hz
Look up HTLs for 2000Hz in Table 7.1.6 to give the loss at 2000 Hz
Look up HTLs for 3000Hz in Table 7.1.7 to give the loss at 3000 Hz
Look up HTLs for 4000Hz in Table 7.1.8 to give the loss at 4000 Hz
This process gives rise to six frequency-specific losses. These six frequency-specific losses are summed to give the APHL for the relevant type of accepted deafness.
The calculations are best set out in a tabular form as below:
Accepted Hearing Loss
FREQ | Hearing Levels (dB) | Loss |
(Hz) | Right | Left | (%) |
500 | | | |
1000 | | | |
1500 | | | |
2000 | | | |
3000 | | | |
4000 | | | |
The figures to be entered in the columns headed “Right” and “Left” will be obtained from the audiogram.
The figures to be entered in the column headed “Loss (%)” are to be obtained by applying Tables 7.1.3 to 7.1.8. (A different scale is used for each row of the calculation.)
The figures in the column headed “Loss (%)” are then to be added up to give the APHL.
The Accepted Percentage Hearing Loss for different types of deafness can be calculated by using air conduction, bone conduction, various combinations of the two or a special formula. The relevant rules are summarised in Table 7.1.2 and in the text which follows it. (The “types” mentioned in Table 7.1.2 refer to the combination of hearing losses as described in the preceding text and not necessarily to named accepted conditions.)
Table 7.1.2 sets out which HTLs (air or bone) from the audiogram are to used in calculating APHL.
Procedural Table 7.1.2 | 
|
TYPES OF AUDIOGRAM TO BE USED |
| For Right HTL use: | For Left HTL use: |
Type 1 | Bilateral mixed deafness | Air | Air |
Type 2 | Right mixed deafness | Air | 0 (zeros) |
Type 3 | Left mixed deafness | 0 (zeros) | Air |
Type 4 | Bilateral sensorineural deafness | Bone | Bone |
Type 5 | Bilateral sensorineural deafness with right conductive deafness | Air | Bone |
Type 6 | Bilateral sensorineural deafness with left conductive deafness | Bone | Air |
Type 7 | Bilateral conductive deafness | See Substep 3A | |
Type 8 | Bilateral conductive deafness with right sensorineural deafness | Air | Air |
Type 9 | Bilateral conductive deafness with left sensorineural deafness | Air | Air |
Type 10 | Left conductive deafness with right sensorineural deafness | Bone | Air |
Type 11 | Right conductive deafness with left sensorineural deafness | Air | Bone |
Type 12 | Right conductive deafness | See Substep 3A | |
Type 13 | Right sensorineural deafness | Bone | 0 (zeros) |
Type 14 | Left sensorineural deafness | 0 (zeros) | Bone |
Type 15 | Left conductive deafness | See Substep 3A | |
| | | | |
Information and instructions concerning the use of bone HTLs are to be found on the next page, and apply in all cases where “Bone” appears in this table or in which reference is made to Substep 3A.
Information and instructions concerning the use of bone HTLs
1. Whenever the use of bone conduction HTL values is specified but if it is not practicable or appropriate to obtain bone conduction HTL values as a result of any of the reasons described on page 108, air conduction HTL values may be used instead.
2. Threshold of Reliability.
Bone conduction HTLs in excess of 60 deciBels are generally unreliable. At the 500 Hz frequency, bone conduction HTLs in excess of 45 deciBels are unreliable.
Thus a set of thresholds of reliability for bone HTLs is defined as follows:
for 500 Hz 45 deciBels
for 1000 Hz 60 deciBels
for 1500 Hz 60 deciBels
for 2000 Hz 60 deciBels
for 3000 Hz 60 deciBels
for 4000 Hz 60 deciBels
Figures in excess of the threshold of reliability for bone conduction are not used in calculating the impairment due to hearing loss.
For sensorineural hearing loss, whenever the bone conduction HTL exceeds the threshold of reliability, the air conduction HTL for that frequency and side is to be used instead of the bone conduction HTL.
For conductive hearing loss, whenever the bone conduction HTL exceeds the threshold of reliability, the threshold figure for that frequency and side is to be used instead of the bone conduction HTL.
The above arrangement gives to the veteran the benefit of any doubt relating to the intrinsic unreliability of bone HTLs.
Substep 3A: Calculation of accepted hearing loss for types 7, 12, and 15.
Substep 3A applies to these types of accepted hearing loss:
- Type 7 Bilateral Conductive deafness
- Type 12 Right Conductive deafness
- Type 15 Left Conductive deafness.
For each type, one of two methods is to be used:
Method 1 is to be applied if both air and bone conduction HTLs are available. In this case both the air and bone conduction HTLs are calculated and a formula is applied. In calculating the bone conduction HTL, if the bone conduction HTL exceeds the threshold of reliability, the threshold figure for that frequency and side is to be used instead of the bone conduction HTL.
The terms “air conduction PLH (Percentage Loss of Hearing)” and “bone conduction PLH” are used in the formulas. These are calculated in a way similar to that in which APHL is calculated for other types of deafness.
Method 2 is to be applied if only air conduction HTLs are available and if it is not practicable or appropriate to obtain bone conduction HTL values as a result of any of the reasons described on page 108.
Type 7. Bilateral conductive deafness
Method 1 (to be applied if both air and bone conduction HTLs are available):
First:
Air Conduction PLH is to be calculated using right and left air conduction HTL values, and
Bone Conduction PLH is to be calculated using right and left bone conduction HTL values.
Next:
Using the air conduction and bone conduction PLHs, the PLH for bilateral conductive deafness is calculated by applying the following formula:
Conductive PLH = | (A - B) × 100 100 - B |
(where “A” is air conduction PLH, and “B” is bone conduction PLH).
No adjustment for age is to be applied to the results of applying the formula. That result is the age adjusted PLH for bilateral conductive deafness.
Go to Step 5 (on page 122).
Method 2 (to be applied if only air conduction HTLs are available and if it is not practicable or appropriate to obtain bone conduction HTL values as a result of any of the reasons described on page 108.
PLH is to be calculated using measured right and left air conduction HTL values. The formula is not applied and so age adjustment is required.
Go to Step 4 (on page 120).
Type 12. Right conductive deafness
Method 1 (to be applied if both air and bone conduction HTLs are available):
First:
Air Conduction PLH is to be calculated using right air conduction HTL values and taking the left air conduction HTL values all to be zero; and
Bone Conduction PLH is to be calculated using right bone conduction HTL values and taking the left bone conduction HTL values all to be zero.
Next:
Using the air conduction and bone conduction PLHs, the PLH for right conductive deafness is calculated by applying the following formula:
Conductive PLH = | (A - B) × 100 100 - B |
(where “A” is air conduction PLH, and “B” is bone conduction PLH).
No adjustment for age is to be applied to the results of applying the formula. That result is the age adjusted PLH for right conductive deafness.
Go to Step 5 (on page 122).
Method 2 (to be applied if only air conduction HTLs are available and if it is not practicable or appropriate to obtain bone conduction HTL values as a result of any of the reasons described on page 108).
PLH is to be calculated using right air conduction HTL values and taking the left air conduction HTL values all to be zero. The formula is not applied and so age adjustment is required.
Go to Step 4 (on page 120).
Type 15. Left conductive deafness
Method 1 (to be applied if both air and bone conduction HTLs are available):
First:
Air Conduction PLH is to be calculated using left air conduction HTL values and taking the right air conduction HTL values all to be zero; and
Bone Conduction PLH is to be calculated using left bone conduction HTL values and taking the right bone conduction HTL values all to be zero.
Next:
Using the air conduction and bone conduction PLHs, the PLH for right conductive deafness is calculated applying the following formula:
Conductive PLH = | (A - B) × 100 100 - B |
(where “A” is air conduction PLH, and “B” is bone conduction PLH)
No adjustment for age is to be applied to the results of applying the formula. That result is the age adjusted PLH for left conductive deafness.
Go to Step 5 (on page 122).
Method 2 (to be applied if only air conduction HTLs are available and if it is not practicable or appropriate to obtain bone conduction HTL values as a result of any of the reasons described on page 108).
PLH is to be calculated using left air conduction HTL values and taking the right air conduction HTL values all to be zero. The formula is not applied and so age adjustment is required.
Go to Step 4 (on page 120).
Table 7.1.3
500 Hz | 
|
Values of percentage of loss of hearing corresponding to given hearing threshold levels in the better and worse ear at 500 Hz |
HTL — Better ear |
| | <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
<=15 | 0.0 | | | | | | | | | | | | | | | | |
20 | 0.4 | 0.6 | | | | | | | | | | | | | | | |
25 | 0.6 | 1.0 | 1.4 | | | | | | | | | | | | | | |
30 | 1.0 | 1.4 | 2.0 | 2.8 | | | | | | | | | | | | | |
35 | 1.3 | 1.8 | 2.5 | 3.4 | 4.5 | | | | | | | | | | | | |
40 | 1.7 | 2.2 | 3.0 | 3.9 | 5.1 | 6.4 | | | | | | | | | | | |
45 | 2.0 | 2.6 | 3.4 | 4.3 | 5.5 | 6.8 | 8.1 | | | | | | | | | | |
50 | 2.3 | 2.9 | 3.7 | 4.7 | 5.8 | 7.1 | 8.4 | 9.7 | | | | | | | | | |
55 | 2.5 | 3.2 | 4.0 | 5.0 | 6.1 | 7.3 | 8.6 | 9.9 | 11.2 | | | | | | | | |
60 | 2.7 | 3.4 | 4.2 | 5.2 | 6.3 | 7.5 | 8.8 | 10.0 | 11.3 | 12.6 | | | | | | | |
65 | 2.8 | 3.5 | 4.4 | 5.4 | 6.5 | 7.7 | 8.9 | 10.2 | 11.5 | 12.7 | 14.0 | | | | | | |
70 | 2.9 | 3.7 | 4.5 | 5.5 | 6.6 | 7.8 | 9.1 | 10.3 | 11.6 | 12.9 | 14.2 | 15.5 | | | | | |
75 | 3.0 | 3.8 | 4.7 | 5.7 | 6.8 | 8.0 | 9.2 | 10.5 | 11.8 | 13.1 | 14.5 | 15.7 | 16.9 | | | | |
80 | 3.1 | 3.9 | 4.8 | 5.8 | 6.9 | 8.1 | 9.3 | 10.6 | 12.0 | 13.3 | 14.7 | 16.0 | 17.2 | 18.2 | | | |
85 | 3.2 | 4.0 | 4.9 | 5.9 | 7.0 | 8.2 | 9.4 | 10.7 | 12.1 | 13.5 | 14.9 | 16.2 | 17.4 | 18.4 | 19.1 | | |
90 | 3.4 | 4.1 | 5.0 | 6.0 | 7.1 | 8.3 | 9.5 | 10.8 | 12.2 | 13.6 | 15.0 | 16.3 | 17.6 | 18.5 | 19.2 | 19.7 | |
>=95 | 3.4 | 4.2 | 5.1 | 6.1 | 7.1 | 8.3 | 9.5 | 10.8 | 12.2 | 13.6 | 15.0 | 16.4 | 17.6 | 18.6 | 19.3 | 19.7 | 20.0 |
| <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
| | | | | | | | | | | | | | | | | | | |
Note: the worse ear is the one with the higher value HTL!
Table 7.1.4
1000 Hz | 
|
Values of percentage of loss of hearing corresponding to given hearing threshold levels in the better and worse ear at 1000 Hz |
HTL — Better ear |
| | <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
<=15 | 0.0 | | | | | | | | | | | | | | | | |
20 | 0.5 | 0.8 | | | | | | | | | | | | | | | |
25 | 0.8 | 1.2 | 1.8 | | | | | | | | | | | | | | |
30 | 1.2 | 1.7 | 2.5 | 3.5 | | | | | | | | | | | | | |
35 | 1.7 | 2.3 | 3.1 | 4.3 | 5.7 | | | | | | | | | | | | |
40 | 2.1 | 2.8 | 3.7 | 4.9 | 6.3 | 8.0 | | | | | | | | | | | |
45 | 2.5 | 3.3 | 4.2 | 5.4 | 6.9 | 8.5 | 10.2 | | | | | | | | | | |
50 | 2.8 | 3.6 | 4.7 | 5.9 | 7.3 | 8.8 | 10.5 | 12.1 | | | | | | | | | |
55 | 3.1 | 3.9 | 5.0 | 6.2 | 7.6 | 9.1 | 10.7 | 12.4 | 14.0 | | | | | | | | |
60 | 3.3 | 4.2 | 5.3 | 6.5 | 7.9 | 9.4 | 11.0 | 12.6 | 14.2 | 15.7 | | | | | | | |
65 | 3.5 | 4.4 | 5.5 | 6.7 | 8.1 | 9.6 | 11.2 | 12.8 | 14.4 | 15.9 | 17.5 | | | | | | |
70 | 3.7 | 4.6 | 5.7 | 6.9 | 8.3 | 9.8 | 11.3 | 12.9 | 14.6 | 16.2 | 17.8 | 19.4 | | | | | |
75 | 3.8 | 4.7 | 5.8 | 7.1 | 8.5 | 10.0 | 11.5 | 13.1 | 14.8 | 16.4 | 18.1 | 19.7 | 21.1 | | | | |
80 | 3.9 | 4.9 | 6.0 | 7.3 | 8.6 | 10.1 | 11.7 | 13.3 | 15.0 | 16.7 | 18.4 | 20.0 | 21.5 | 22.7 | | | |
85 | 4.1 | 5.0 | 6.2 | 7.4 | 8.8 | 10.3 | 11.8 | 13.4 | 15.1 | 16.9 | 18.6 | 20.3 | 21.7 | 23.0 | 23.9 | | |
90 | 4.2 | 5.2 | 6.3 | 7.5 | 8.9 | 10.3 | 11.9 | 13.5 | 15.2 | 17.0 | 18.7 | 20.4 | 21.9 | 23.2 | 24.1 | 24.6 | |
>=95 | 4.3 | 5.3 | 6.4 | 7.6 | 8.9 | 10.3 | 11.9 | 13.5 | 15.2 | 17.0 | 18.7 | 20.5 | 22.0 | 23.3 | 24.2 | 24.7 | 25.0 |
| <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
| | | | | | | | | | | | | | | | | | | |
Note: the worse ear is the one with the higher value HTL!
Table 7.1.5
1500 Hz | 
|
Values of percentage of loss of hearing corresponding to given hearing threshold levels in the better and worse ear at 1500 Hz |
HTL — Better ear |
| | <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
<=15 | 0.0 | | | | | | | | | | | | | | | | |
20 | 0.4 | 0.6 | | | | | | | | | | | | | | | |
25 | 0.6 | 1.0 | 1.4 | | | | | | | | | | | | | | |
30 | 1.0 | 1.4 | 2.0 | 2.8 | | | | | | | | | | | | | |
35 | 1.3 | 1.8 | 2.5 | 3.4 | 4.5 | | | | | | | | | | | | |
40 | 1.7 | 2.2 | 3.0 | 3.9 | 5.1 | 6.4 | | | | | | | | | | | |
45 | 2.0 | 2.6 | 3.4 | 4.3 | 5.5 | 6.8 | 8.1 | | | | | | | | | | |
50 | 2.3 | 2.9 | 3.7 | 4.7 | 5.8 | 7.1 | 8.4 | 9.7 | | | | | | | | | |
55 | 2.5 | 3.2 | 4.0 | 5.0 | 6.1 | 7.3 | 8.6 | 9.9 | 11.2 | | | | | | | | |
60 | 2.7 | 3.4 | 4.2 | 5.2 | 6.3 | 7.5 | 8.8 | 10.0 | 11.3 | 12.6 | | | | | | | |
65 | 2.8 | 3.5 | 4.4 | 5.4 | 6.5 | 7.7 | 8.9 | 10.2 | 11.5 | 12.7 | 14.0 | | | | | | |
70 | 2.9 | 3.7 | 4.5 | 5.5 | 6.6 | 7.8 | 9.1 | 10.3 | 11.6 | 12.9 | 14.2 | 15.5 | | | | | |
75 | 3.0 | 3.8 | 4.7 | 5.7 | 6.8 | 8.0 | 9.2 | 10.5 | 11.8 | 13.1 | 14.5 | 15.7 | 16.9 | | | | |
80 | 3.1 | 3.9 | 4.8 | 5.8 | 6.9 | 8.1 | 9.3 | 10.6 | 12.0 | 13.3 | 14.7 | 16.0 | 17.2 | 18.2 | | | |
85 | 3.2 | 4.0 | 4.9 | 5.9 | 7.0 | 8.2 | 9.4 | 10.7 | 12.1 | 13.5 | 14.9 | 16.2 | 17.4 | 18.4 | 19.1 | | |
90 | 3.4 | 4.1 | 5.0 | 6.0 | 7.1 | 8.3 | 9.5 | 10.8 | 12.2 | 13.6 | 15.0 | 16.3 | 17.6 | 18.5 | 19.2 | 19.7 | |
>=95 | 3.4 | 4.2 | 5.1 | 6.1 | 7.1 | 8.3 | 9.5 | 10.8 | 12.2 | 13.6 | 15.0 | 16.4 | 17.6 | 18.6 | 19.3 | 19.7 | 20.0 |
| <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
| | | | | | | | | | | | | | | | | | | |
Note: the worse ear is the one with the higher value HTL!
Scale 7.1.6
2000 Hz | 
|
Values of percentage of loss of hearing corresponding to given hearing threshold levels in the better and worse ear at 2000 Hz |
HTL — Better ear |
| | <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
<=15 | 0.0 | | | | | | | | | | | | | | | | |
20 | 0.3 | 0.5 | | | | | | | | | | | | | | | |
25 | 0.5 | 0.7 | 1.1 | | | | | | | | | | | | | | |
30 | 0.7 | 1.0 | 1.5 | 2.1 | | | | | | | | | | | | | |
35 | 1.0 | 1.4 | 1.9 | 2.5 | 3.4 | | | | | | | | | | | | |
40 | 1.3 | 1.7 | 2.2 | 2.9 | 3.8 | 4.8 | | | | | | | | | | | |
45 | 1.5 | 1.9 | 2.5 | 3.3 | 4.1 | 5.1 | 6.1 | | | | | | | | | | |
50 | 1.7 | 2.2 | 2.8 | 3.5 | 4.4 | 5.3 | 6.3 | 7.3 | | | | | | | | | |
55 | 1.9 | 2.4 | 3.0 | 3.7 | 4.6 | 5.5 | 6.4 | 7.4 | 8.4 | | | | | | | | |
60 | 2.0 | 2.5 | 3.1 | 3.9 | 4.7 | 5.6 | 6.6 | 7.5 | 8.5 | 9.4 | | | | | | | |
65 | 2.1 | 2.6 | 3.3 | 4.0 | 4.9 | 5.7 | 6.7 | 7.6 | 8.6 | 9.6 | 10.5 | | | | | | |
70 | 2.2 | 2.7 | 3.4 | 4.1 | 5.0 | 5.9 | 6.8 | 7.8 | 8.7 | 9.7 | 10.7 | 11.6 | | | | | |
75 | 2.3 | 2.8 | 3.5 | 4.3 | 5.1 | 6.0 | 6.9 | 7.9 | 8.9 | 9.9 | 10.8 | 11.8 | 12.7 | | | | |
80 | 2.4 | 2.9 | 3.6 | 4.4 | 5.2 | 6.1 | 7.0 | 8.0 | 9.0 | 10.0 | 11.0 | 12.0 | 12.9 | 13.6 | | | |
85 | 2.4 | 3.0 | 3.7 | 4.4 | 5.3 | 6.1 | 7.1 | 8.1 | 9.1 | 10.1 | 11.1 | 12.1 | 13.0 | 13.8 | 14.3 | | |
90 | 2.5 | 3.1 | 3.8 | 4.5 | 5.3 | 6.2 | 7.1 | 8.1 | 9.1 | 10.2 | 11.2 | 12.2 | 13.2 | 13.9 | 14.4 | 14.8 | |
>=95 | 2.6 | 3.2 | 3.8 | 4.6 | 5.4 | 6.2 | 7.1 | 8.1 | 9.1 | 10.2 | 11.3 | 12.3 | 13.2 | 14.0 | 14.5 | 14.8 | 15.0 |
| <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
| | | | | | | | | | | | | | | | | | | |
Note: the worse ear is the one with the higher value HTL!
Table 7.1.7 3000 Hz | 
|
Values of percentage of loss of hearing corresponding to given hearing threshold levels in the better and worse ear at 3000 Hz |
HTL — Better ear |
| | <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
<=15 | 0.0 | | | | | | | | | | | | | | | | |
20 | 0.2 | 0.3 | | | | | | | | | | | | | | | |
25 | 0.3 | 0.5 | 0.7 | | | | | | | | | | | | | | |
30 | 0.5 | 0.7 | 1.0 | 1.4 | | | | | | | | | | | | | |
35 | 0.7 | 0.9 | 1.2 | 1.7 | 2.3 | | | | | | | | | | | | |
40 | 0.8 | 1.1 | 1.5 | 2.0 | 2.5 | 3.2 | | | | | | | | | | | |
45 | 1.0 | 1.3 | 1.7 | 2.2 | 2.7 | 3.4 | 4.1 | | | | | | | | | | |
50 | 1.1 | 1.4 | 1.9 | 2.3 | 2.9 | 3.5 | 4.2 | 4.8 | | | | | | | | | |
55 | 1.2 | 1.6 | 2.0 | 2.5 | 3.0 | 3.6 | 4.3 | 4.9 | 5.6 | | | | | | | | |
60 | 1.3 | 1.7 | 2.1 | 2.6 | 3.1 | 3.7 | 4.4 | 5.0 | 5.6 | 6.3 | | | | | | | |
65 | 1.4 | 1.8 | 2.2 | 2.7 | 3.2 | 3.8 | 4.4 | 5.1 | 5.7 | 6.4 | 7.0 | | | | | | |
70 | 1.5 | 1.8 | 2.3 | 2.8 | 3.3 | 3.9 | 4.5 | 5.2 | 5.8 | 6.5 | 7.1 | 7.7 | | | | | |
75 | 1.5 | 1.9 | 2.3 | 2.8 | 3.4 | 4.0 | 4.6 | 5.2 | 5.9 | 6.6 | 7.2 | 7.8 | 8.4 | | | | |
80 | 1.6 | 2.0 | 2.4 | 2.9 | 3.4 | 4.0 | 4.7 | 5.3 | 6.0 | 6.6 | 7.3 | 8.0 | 8.6 | 9.1 | | | |
85 | 1.6 | 2.0 | 2.5 | 3.0 | 3.5 | 4.1 | 4.7 | 5.4 | 6.0 | 6.7 | 7.4 | 8.1 | 8.7 | 9.2 | 9.5 | | |
90 | 1.7 | 2.1 | 2.5 | 3.0 | 3.5 | 4.1 | 4.7 | 5.4 | 6.1 | 6.8 | 7.5 | 8.2 | 8.8 | 9.2 | 9.6 | 9.8 | |
>=95 | 1.7 | 2.1 | 2.6 | 3.0 | 3.6 | 4.1 | 4.7 | 5.4 | 6.1 | 6.8 | 7.5 | 8.2 | 8.8 | 9.3 | 9.6 | 9.8 | 10.0 |
| <=15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
Note: the worse ear is the one with the higher value HTL!
Table 7.1.8 4000 Hz | 
|
Values of percentage of loss of hearing corresponding to given hearing threshold levels in the better and worse ear at 4000 Hz |
HTL — Better ear |
| | <=20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
<=20 | 0.0 | | | | | | | | | | | | | | | |
25 | 0.2 | 0.3 | | | | | | | | | | | | | | |
30 | 0.3 | 0.5 | 0.8 | | | | | | | | | | | | | |
35 | 0.5 | 0.7 | 1.0 | 1.5 | | | | | | | | | | | | |
40 | 0.6 | 0.9 | 1.3 | 1.8 | 2.5 | | | | | | | | | | | |
45 | 0.8 | 1.1 | 1.5 | 2.1 | 2.7 | 3.5 | | | | | | | | | | |
50 | 0.9 | 1.3 | 1.7 | 2.3 | 2.9 | 3.6 | 4.4 | | | | | | | | | |
55 | 1.0 | 1.4 | 1.9 | 2.4 | 3.1 | 3.8 | 4.5 | 5.2 | | | | | | | | |
60 | 1.2 | 1.5 | 2.0 | 2.6 | 3.2 | 3.9 | 4.6 | 5.3 | 6.0 | | | | | | | |
65 | 1.2 | 1.6 | 2.1 | 2.7 | 3.3 | 3.9 | 4.6 | 5.3 | 6.0 | 6.7 | | | | | | |
70 | 1.3 | 1.7 | 2.2 | 2.7 | 3.4 | 4.0 | 4.7 | 5.4 | 6.1 | 6.8 | 7.5 | | | | | |
75 | 1.4 | 1.8 | 2.3 | 2.8 | 3.4 | 4.1 | 4.8 | 5.5 | 6.2 | 6.9 | 7.6 | 8.2 | | | | |
80 | 1.4 | 1.9 | 2.3 | 2.9 | 3.5 | 4.2 | 4.9 | 5.6 | 6.3 | 7.0 | 7.7 | 8.4 | 8.9 | | | |
85 | 1.5 | 1.9 | 2.4 | 3.0 | 3.6 | 4.2 | 4.9 | 5.7 | 6.4 | 7.1 | 7.8 | 8.5 | 9.0 | 9.5 | | |
90 | 1.6 | 2.0 | 2.5 | 3.0 | 3.6 | 4.3 | 5.0 | 5.7 | 6.5 | 7.2 | 7.9 | 8.6 | 9.1 | 9.5 | 9.8 | |
>=95 | 1.6 | 2.0 | 2.5 | 3.1 | 3.7 | 4.3 | 5.0 | 5.7 | 6.5 | 7.2 | 8.0 | 8.7 | 9.2 | 9.6 | 9.8 | 10.0 |
| <=20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | >=95 |
Note: the worse ear is the one with the higher value HTL!
Step 4: Make any necessary age adjustment.
Calculate the veteran’s age (in completed years) at the date of the audiogram being used. For example, a veteran whose 67th birthday fell on the day after the audiogram was performed, was 66 on the date of the audiogram.
Determine the appropriate adjustment for presbyacusis from Table 7.1.9.
Table 7.1.9 includes different values for both males and females and has separate columns for bilateral accepted hearing losses and for unilateral accepted hearing losses.
The value obtained from Table 7.1.9 is subtracted from the PLH.
The tabular format below shows how the work can be set out. The “adjustment for presbyacusis” (obtained from Table 7.1.9) is to be subtracted from the APLH (obtained in Step 3). The result of this subtraction is the “age adjusted hearing loss”.
Accepted Hearing Loss
FREQ | Hearing Levels (dB) | Loss |
(Hz) | Right | Left | (%) |
500 | | | |
1000 | | | |
1500 | | | |
2000 | | | |
3000 | | | |
4000 | | | |
APHL | = | | |
adjustment for presbyacusis | = | | from Table 7.1.9 |
age adjusted hearing loss | = | | |
PLHB = Percentage bilateral loss of hearing due to age and is dependent upon both age and gender.
PLHU = Percentage unilateral loss of hearing due to age and is dependent upon both age and gender.
Table 7.1.9 | 
|
ADJUSTMENT FOR PRESBYACUSIS |
Age (in years) | Bilateral | Unilateral |
Males PLHB (percent) | Females PLHB (percent) | Males PLHU (percent) | Females PLHU (percent) |
below 60 | 0 | 0 | 0 | 0 |
60 | 0 | 0 | 0 | 0 |
61 | 0.1 | 0 | 0 | 0 |
62 | 0.2 | 0 | 0 | 0 |
63 | 0.4 | 0 | 0.1 | 0 |
64 | 0.6 | 0 | 0.1 | 0 |
65 | 0.8 | 0 | 0.1 | 0 |
66 | 1.0 | 0 | 0.2 | 0 |
67 | 1.3 | 0. | 0.2 | 0 |
68 | 1.7 | 0 | 0.3 | 0 |
69 | 2.0 | 0 | 0.3 | 0 |
70 | 2.4 | 0 | 0.4 | 0 |
71 | 2.9 | 0 | 0.5 | 0 |
72 | 3.3 | 0 | 0.6 | 0 |
73 | 3.8 | 0 | 0.6 | 0 |
74 | 4.4 | 0.2 | 0.7 | 0 |
75 | 4.9 | 0.4 | 0.8 | 0.1 |
76 | 5.5 | 0.6 | 0.9 | 0.1 |
77 | 6.2 | 0.8 | 1.0 | 0.1 |
78 | 6.8 | 1.1 | 1.2 | 0.2 |
79 | 7.5 | 1.4 | 1.3 | 0.2 |
80 | 8.3 | 1.7 | 1.4 | 0.3 |
81 | 9.0 | 2.1 | 1.5 | 0.4 |
82 | 9.8 | 2.5 | 1.7 | 0.4 |
83 | 10.7 | 2.9 | 1.8 | 0.5 |
84 | 11.5 | 3.4 | 2.0 | 0.6 |
85 | 12.5 | 3.9 | 2.1 | 0.7 |
above 85 | 12.5 | 3.9 | 2.1 | 0.7 |
| | | | | |
(The adjustments for presbyacusis in Table 7.1.9 have been modified from the adjustments provided by the National Acoustic Laboratories.)
“Age” means the veteran’s age in completed years at the date of the audiogram.
The “Bilateral” column applies if there is accepted hearing loss in both ears.
The “Unilateral” column applies if there is accepted hearing loss in only one ear.
Step 5: Determine the impairment rating for the accepted hearing loss using formula 7.1.
Formula 7.1— Loss of function: Hearing
Impairment rating = | age adjusted hearing loss 2 |
Results from Formula 7.1 are to be rounded to the nearest integer (whole number). Thus 2.4 would be rounded to 2, and 2.6 would be rounded to 3. If the calculation gives an answer exactly half way between two integers, the answer is rounded up, for example 2.5 is to be rounded to 3.
If the paired organs policy (see page 123) does not apply, Formula 7.1 gives the final impairment rating for loss of hearing. To determine whether the paired organs policy applies, proceed to Step 6.
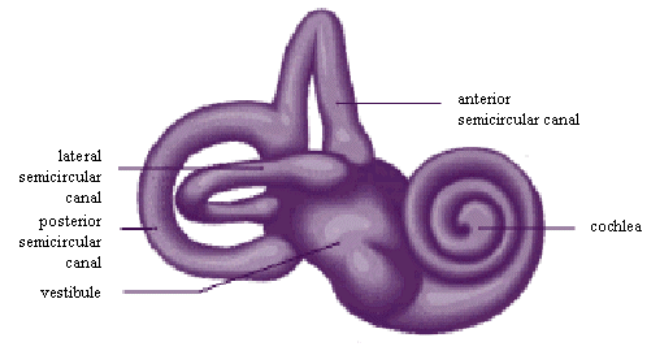
Step 6. Determine if the paired organs policy applies. If it applies, calculate the adjusted impairment rating.
Use Table 7.1.10 to determine if the paired organs policy applies.
Procedural Table 7.1.10 | 
|
PAIRED ORGANS POLICY |
Accepted Hearing Loss | Does the Paired Organs Policy apply? |
Type 1 | Bilateral mixed deafness | No |
Type 2 | Right mixed deafness | Yes |
Type 3 | Left mixed deafness | Yes |
Type 4 | Bilateral sensorineural deafness | No |
Type 5 | Bilateral sensorineural deafness with right conductive deafness | No |
Type 6 | Bilateral sensorineural deafness with left conductive deafness | No |
Type 7 | Bilateral conductive deafness | No |
Type 8 | Bilateral conductive deafness with right sensorineural deafness | No |
Type 9 | Bilateral conductive deafness with left sensorineural deafness | No |
Type 10 | Left conductive deafness with right sensorineural deafness | No |
Type 11 | Right conductive deafness with left sensorineural deafness | No |
Type 12 | Right conductive deafness | Yes |
Type 13 | Right sensorineural deafness | Yes |
Type 14 | Left sensorineural deafness | Yes |
Type 15 | Left conductive deafness | Yes |
| | | |
The paired organs policy is to be applied by doubling the impairment rating for the age-adjusted PLH for the accepted hearing loss and comparing that with the impairment rating equivalent to the total bilateral hearing loss. The lesser of the two is to be taken as the impairment rating (adjusted for the paired organs policy) for the accepted hearing loss.
The paired organs policy is the subject of Chapter 21.
Tinnitus is to be assessed if:
- tinnitus is an accepted condition in its own right; or
- tinnitus is present and any of the fifteen types of hearing loss is an accepted condition for the ear in which tinnitus is present.
Tinnitus is not to be assessed when it is a rejected condition.
Irrespective of whether there are any non-accepted conditions contributing to the tinnitus, the rating is not to be moderated by applying Chapter 19 (Partially Contributing Impairment).
If impairment ratings are obtained for hearing loss and tinnitus both are to be included in the final combining of all impairment ratings by applying Chapter 18 (Combined Values Chart).
To assess tinnitus, make the appropriate selection from Table 7.1.11 below.
Functional Loss Table 7.1.11 | 
|
TINNITUS |
Impairment Ratings | Criteria |
NIL | No tinnitus or occasional tinnitus. |
TWO | Very mild tinnitus: not present every day. |
FIVE | Tinnitus every day, but tolerable for much of the time. |
TEN | Severe tinnitus, eg of similar severity to that requiring a masking device, present every day. |
FIFTEEN | Very severe tinnitus, present every day, causing distraction, loss of concentration and extreme discomfort, and regularly interfering with sleep. |
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
PART 7.2: EAR, NOSE, AND THROAT
The three tables in this Part are all Other Impairment tables.
Impairment of speech is to be assessed by applying Chapter 5 (Neurological Impairment).
Loss of balance is commonly paroxysmal and is usually best rated by applying Chapter 15 (Intermittent Impairment).
Loss of taste and loss of smell are to be assessed by applying Chapter 5 (Neurological Impairment).
Other Impairment Table 7.2.1 | 
|
EARS |
Impairment Ratings | Criteria |
NIL | Intermittent otalgia, intermittent otorrhoea, or both. |
TWO | Otitis externa. |
FIVE | - Otalgia every day, but tolerable for much of the time.
- Continuous otorrhoea.
|
TEN | Frequent severe otalgia. |
| Only one rating is to be selected from this table for any condition or combination of conditions. |
| | |
If accepted conditions affect both ears, they are to be rated together and only a single rating is to be given for them.
Chapter 15 (Intermittent Impairment) may be applied for more severe or frequent aural conditions.
UPPER RESPIRATORY TRACT AND NASAL CONDITIONS
Other Impairment Table 7.2.2 | 
|
UPPER RESPIRATORY TRACT AND NASAL CONDITIONS |
Impairment Ratings | Criteria |
NIL | Intermittent post-nasal discharge, rhinorrhoea and/or sneezing. |
TWO | Recurrent upper respiratory tract infection. |
FIVE | Symptoms of rhinitis and sinusitis or both which are not relieved by medication and which occur for more than 4 months every year. |
| Only one rating is to be selected from this table for any condition or combination of conditions. |
| | |
Chapter 15 (Intermittent Impairment) may be applied for upper respiratory tract and nasal conditions which are sufficiently severe or frequent.
THROAT
Other Impairment Table 7.2.3 | 
|
THROAT |
Impairment Ratings | Criteria |
NIL | No tracheostomy. |
TWO | A tracheostomy that has been closed. |
TWENTY | Permanent tracheostomy. |
| | |
INDEX TO HEARING IMPAIRMENT WORKSHEETS
| | Worksheet Numbers |
Type No | Total accepted hearing loss | Air alone | Air & Bone |
1 | Bilateral mixed deafness | 2 | N/A |
2 | Right mixed deafness | 3 | N/A |
3 | Left mixed deafness | 3 | N/A |
4 | Bilateral sensorineural deafness | SND | SND |
5 | Bilateral sensorineural deafness with Right conductive deafness | 2 | N/A |
6 | Bilateral sensorineural deafness with Left conductive deafness | 2 | N/A |
7 | Bilateral conductive deafness | 2 | 4 |
8 | Bilateral conductive deafness with Right sensorineural deafness | 2 | N/A |
9 | Bilateral conductive deafness with Left sensorineural deafness | 2 | N/A |
10 | Left conductive deafness with Right sensorineural deafness | 2 | NWP |
11 | Right conductive deafness with Left sensorineural deafness | 2 | NWP |
12 | Right conductive deafness | 3 | 5 |
13 | Right sensorineural deafness | 3 | NWP |
14 | Left sensorineural deafness | 3 | NWP |
15 | Left conductive deafness | 3 | 5 |
| SND | = | sensorineural deafness |
| N/A | = | not applicable |
| NWP | = | no worksheet provided |
The Type Numbers in the left hand column refer to types of accepted hearing loss as defined in Table 7.1.1 of the Guide.
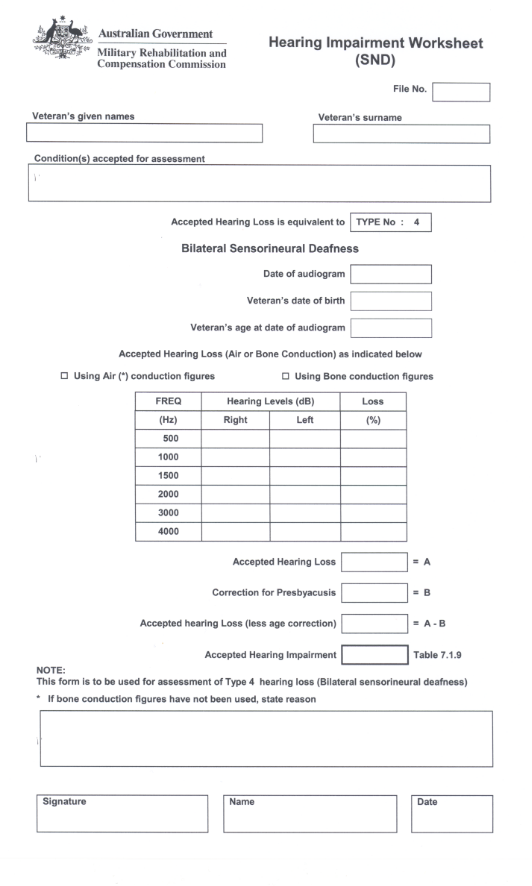
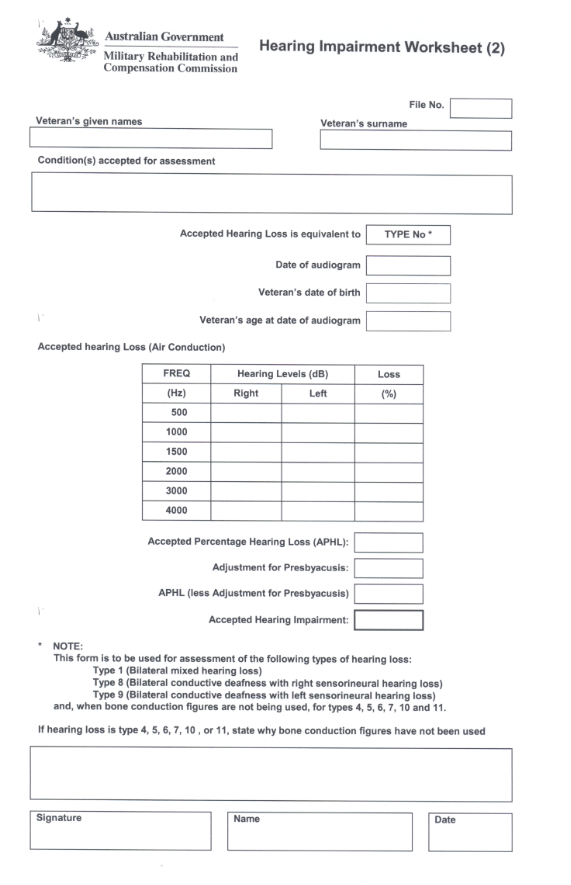
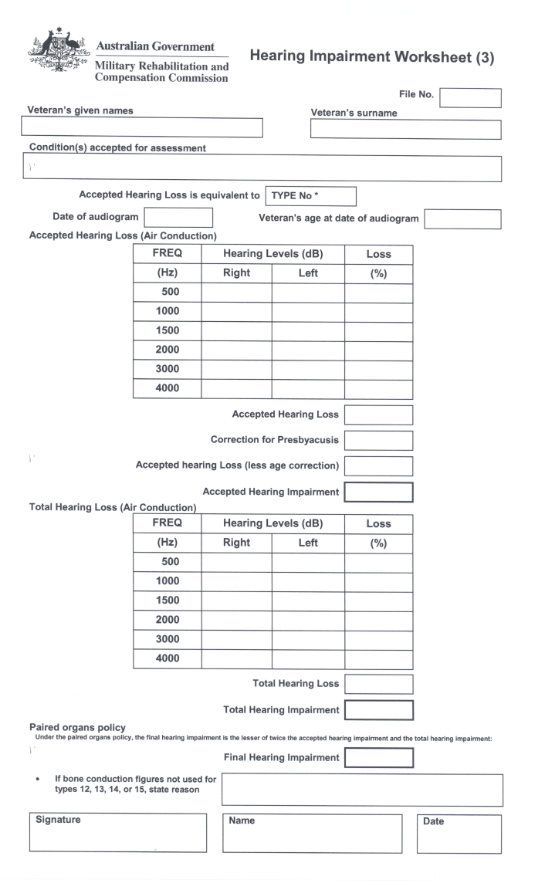
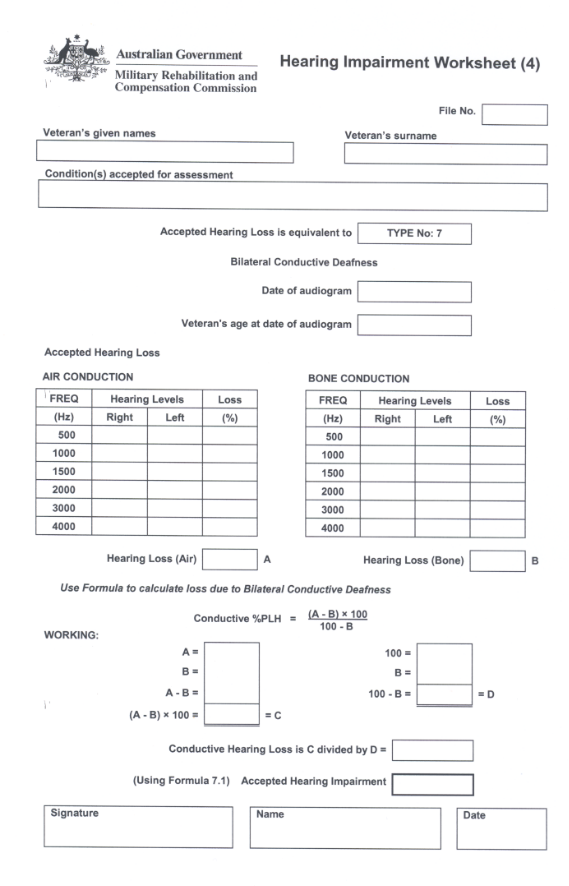
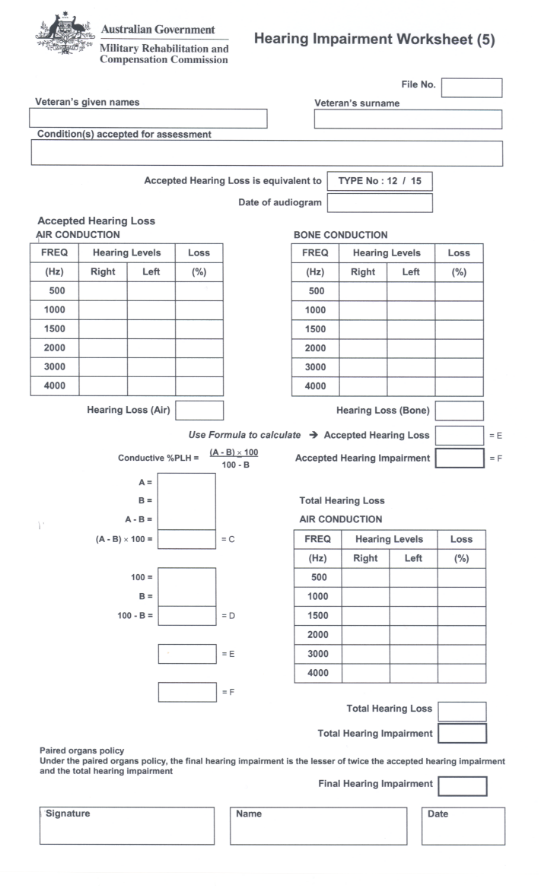
CHAPTER 8
VISUAL IMPAIRMENT
This chapter contains two parts:
Part 8.1 — Impairment of Visual Function
Part 8.2 — Other Ocular Impairment
INTRODUCTION
Part 8.1 is to be applied to assess:
- any condition, such as refractive error, that is actually affecting visual function; and
- any condition, such as glaucoma or cataracts, that in the normal course of its progression would be likely to affect visual function.
Part 8.2 is to be applied to assess such conditions of the eye and the surrounding structures as may lead to discomfort or inconvenience, such as conjunctivitis and conditions of the eyelid, without actually or usually affecting visual function.
PART 8.1: IMPAIRMENT OF VISUAL FUNCTION
Loss of function
Visual function is to be measured by reference to:
- corrected visual acuity (Table 8.1.1 or Table 8.1.3); and
- visual field defects (Figures 8a and 8b); and
- miscellaneous function (Table 8.1.2).
The following steps take into account the fact that normal vision is a binocular function.
Calculation of the impairment rating for loss of visual function
Follow the steps below to calculate the impairment rating due to accepted loss of visual function.
(Each step is elaborated in the following pages.)
STEP 1 | If there is any accepted refractive error, determine the monocular assessment for each eye based on corrected visual acuity. | Page 133 | |
STEP 2 | If there is any accepted condition causing a visual field defect, determine the monocular assessment for each eye affected by the accepted condition. | Page 133 | |
STEP 3 | Determine the monocular assessment for each eye from the Miscellaneous Visual Function Table (Table 8.1.2) as the result of any accepted condition. | Page 134 |
STEP 4 | For each eye separately, combine the ratings obtained in Steps 1, 2, and 3 by applying Chapter 18 (Combined Values Chart). | Page 134 |
STEP 5 | Combine the two combined monocular impairment ratings obtained in Step 4 by applying Table 8.1.3. | Page 135 |
| | | |
Step 1: If there is any accepted refractive error, determine the monocular assessment for each eye based on corrected visual acuity.
All assessments of visual acuity are to be based on corrected visual acuity, that is, the visual acuity as measured when the veteran is wearing glasses or contact lenses correctly prescribed. No additional impairment rating is to be given for the need to wear corrective lenses.
A separate monocular assessment is to be determined for each eye.
If only one eye has a refractive error, or if only one eye is to be assessed, the monocular assessment of the eye is to be determined by applying Table 8.1.1 and the assessment for visual acuity for the other eye is to be taken as nil. (These assessments will ultimately be combined by applying Table 8.1.3.)
Functional Loss Table 8.1.1 | 
|
MONOCULAR ASSESSMENTS FOR CORRECTED VISUAL ACUITY |
Visual acuity |
| 6/6 | 6/9 | 6/12 | 6/18 | 6/24 | 6/30 | 6/36 | 6/48 | 6/60 | 3/60 | Blind* |
Monocular Assessment |
| 0 | 10 | 20 | 30 | 40 | 50 | 60 | 70 | 80 | 90 | 100 |
* In applying the above table, if the veteran’s visual acuity in either eye is such that he or she is only capable of counting fingers or of perceiving the difference between light and darkness with that eye, then he or she is to be taken as “blind” in the eye so affected. |
| | | | | | | | | | | | |
Step 2: If there is any accepted condition causing a visual field defect, determine the monocular assessment for each eye affected by the accepted condition.
Any condition (such as glaucoma) which could cause loss of visual field is to be assessed by measuring that loss. For glaucoma without field loss refer to Table 8.1.2.
Loss of visual field is to be measured either by a manual or a computerised method, using the Esterman grid (Figures 8A and 8B).
Methods of measuring visual field loss
If the field has been defined by a manual method such as a Bjerrum screen with a 5/1000 white target or a Humphrey bowl at 10dB or less, a transparency of the Esterman grid is placed over the map of the visual field. Those dots that fall wholly or partially within the area of field loss are counted, and the number of dots so counted is to be taken as the monocular assessment for the field loss of that eye.
If the field has been defined by the Humphrey computerised method, a transparency of the appropriate Esterman grid is placed over the graytone field map of the eye being assessed. The graytones represent varying degrees of diminished response to visual stimuli. Count those dots that fall wholly or partially within the area of the graytone field map corresponding to the three darkest intensities of the set of ten graytones in the key accompanying the field map. The number of dots so counted is to be taken as the monocular assessment of the field loss of that eye.
If the field has been defined by a computerised method other than the Humphrey method, a transparency of the appropriate Esterman grid is placed over the graytone field map of the eye being assessed. The graytones represent varying degrees of diminished response to visual stimuli. Count those dots that fall wholly or partly within the area of the graytone field map corresponding to the equivalent of 10dB or less of the intensities of the set of ten graytones in the key accompanying the field map. The number of dots so counted is to be taken as the monocular assessment of the field loss of that eye.
Step 3: Determine the monocular assessment for each eye from Table 8.1.2 as the result of any accepted condition.
Only one criterion is to be selected from Table 8.1.2. If more than one criterion could be selected, the criterion resulting in the higher or highest monocular assessment is to be chosen. The single assessment is then included in both monocular assessments. (See below.)
As the criteria in Table 8.1.2 refer to binocular functions, the assessment is included in both monocular assessments. For example, the assessment for unilateral aphakia is to be included in both monocular assessments.
Step 4: For each eye separately, combine the ratings obtained in Steps 1, 2 and 3 by applying Chapter 18 (Combined Values Chart).
Having followed Steps 1, 2 and 3, up to three monocular assessments will have been obtained for each eye depending on the particular accepted visual conditions affecting the veteran.
For example, there may be for the right eye:
- an assessment for corrected visual acuity;
- an assessment for a visual field defect; and
- an assessment for a miscellaneous visual defect.
For each eye separately, these three assessments are to be combined as if they were impairment ratings, by applying Chapter 18 (Combined Values Chart) in accordance with the steps in that chapter. The resulting value is to be rounded to the nearest multiple of 5. This is known as the combined monocular impairment rating for that eye.
Step 5: Combine the two combined monocular impairment ratings obtained in Step 4 by applying Table 8.1.3.
Binocular impairment rating
After a combined monocular impairment rating has been made for each eye, the two ratings are to be combined by applying Table 8.1.3. The value obtained is known as the binocular impairment rating.
Figure 8a - ESTERMAN GRID: LEFT EYE
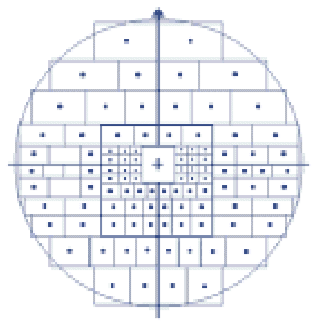
Figure 8b - ESTERMAN GRID: RIGHT EYE
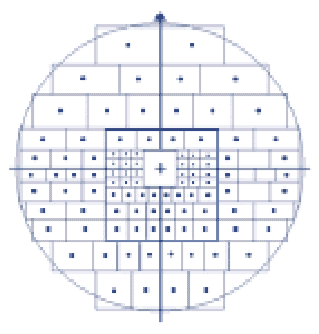
Functional Loss Table 8.1.2 | 
|
MISCELLANEOUS VISUAL FUNCTION |
Visual Disturbance | Monocular Assessment |
Heterophoria | 0 |
Nystagmus without diplopia | 0 |
Cataract with no loss of visual acuity | 2 |
Glaucoma without loss of visual fields | 2 |
Bilateral intraocular lens | 5 |
Unilateral intraocular lens | 5 |
Bilateral aphakia | 5 |
Unilateral aphakia | 10 |
Loss of stereopsis in absence of heterotropia | 5 |
Heterotropia with diplopia one quadrant of upward gaze | 5 |
Heterotropia without diplopia near vision only | 5 |
Heterotropia with diplopia one quadrant of downward gaze | 10 |
Heterotropia without diplopia all directions of gaze | 10 |
Heterotropia with diplopia one direction of sideways gaze | 10 |
Heterotropia with diplopia all directions of upward gaze | 10 |
Heterotropia with diplopia all directions of downward gaze | 15 |
Heterotropia with diplopia both directions of sideways gaze | 15 |
Heterotropia with diplopia all range of near vision | 15 |
Heterotropia with diplopia all directions of gaze | 25 |
Gaze defects vertical | 10 |
Gaze defects horizontal | 10 |
Gaze defects vertical and horizontal | 25 |
Only one criterion may be selected from this table. If the accepted condition satisfies more than one criterion, the criterion resulting in the higher rating is to be chosen. The single rating is then included in both monocular assessments. |
| | |
The combined monocular impairment ratings obtained in Step 4 are those values found in the shaded area of Table 8.1.3. The values for the better and worse eye are to be taken from the values in the shaded regions along the horizontal and vertical axes respectively.
For convenience, Table 8.1.3 incorporates Table 8.1.1 along both its axes. The figures in italics give the possible losses of visual acuity. The values in the shaded area immediately beside or above the figures in italics give the corresponding monocular assessment.
If the only condition affecting visual function is decreased visual acuity, the visual acuities for the better and the worse eye respectively can be read from the values in italics along the horizontal and vertical axes respectively.
Paired organs policy
If an accepted condition affects one eye only, the paired organs policy may apply (see Chapter 21).
Visual Impairment Worksheet
To ensure a consistent and clear record of the use of the tables, the Visual Impairment Worksheet (at page 141) should be used when assessing visual impairment.
A Visual Impairment Worksheet is used when assessing impairment involving visual field or miscellaneous visual conditions.
Functional Loss Table 8.1.3 | 
| |
LOSS OF VISUAL FUNCTION | |
| 6/6 | 0 | 0 | | | | | | | | | | | | | | | | | | | | |
| 5 | 0 | 5 | | | | | | | | | | | | | | | | | | | |
6/9 | 10 | 5 | 5 | 10 | | | | | | | | | | | | | | | | | | |
| 15 | 5 | 10 | 10 | 15 | | | | | | | | | | | | | | | | | |
6/12 | 20 | 5 | 10 | 10 | 15 | 20 | | | | | | | | | | | | | | | | |
| 25 | 5 | 10 | 15 | 15 | 20 | 25 | | | | | | | | | | | | | | | |
6/18 | 30 | 10 | 10 | 15 | 20 | 20 | 25 | 30 | | | | | | | | | | | | | | |
| 35 | 10 | 10 | 15 | 20 | 25 | 25 | 30 | 35 | | | | | | | | | | | | | |
6/24 | 40 | 10 | 15 | 15 | 20 | 25 | 25 | 30 | 35 | 40 | | | | | | | | | | | | |
| 45 | 10 | 15 | 20 | 20 | 25 | 30 | 30 | 35 | 40 | 40 | | | | | | | | | | | |
6/30 | 50 | 10 | 15 | 20 | 25 | 25 | 30 | 35 | 35 | 40 | 45 | 45 | | | | | | | | | | |
| 55 | 15 | 15 | 20 | 25 | 25 | 30 | 35 | 40 | 40 | 45 | 50 | 50 | | | | | | | | | |
6/36 | 60 | 15 | 20 | 20 | 25 | 30 | 30 | 35 | 40 | 40 | 45 | 50 | 55 | 55 | | | | | | | | |
| 65 | 15 | 20 | 25 | 25 | 30 | 35 | 35 | 40 | 45 | 45 | 50 | 55 | 60 | 60 | | | | | | | |
6/48 | 70 | 20 | 20 | 25 | 25 | 30 | 35 | 40 | 40 | 45 | 50 | 50 | 55 | 60 | 60 | 65 | | | | | | |
| 75 | 20 | 20 | 25 | 30 | 30 | 35 | 40 | 40 | 45 | 50 | 55 | 55 | 60 | 65 | 65 | 70 | | | | | |
6/60 | 80 | 20 | 25 | 25 | 30 | 35 | 35 | 40 | 45 | 45 | 50 | 55 | 60 | 60 | 65 | 70 | 70 | 75 | | | | |
| 85 | 20 | 25 | 25 | 30 | 35 | 40 | 40 | 45 | 50 | 50 | 55 | 60 | 60 | 65 | 70 | 75 | 75 | 80 | | | |
3/60 | 90 | 20 | 25 | 30 | 30 | 35 | 40 | 40 | 45 | 50 | 55 | 55 | 60 | 65 | 65 | 70 | 75 | 80 | 80 | 85 | | |
| 95 | 25 | 25 | 30 | 35 | 35 | 40 | 45 | 45 | 50 | 55 | 60 | 60 | 65 | 70 | 70 | 75 | 80 | 85 | 85 | 85 | |
Blind | 100 | 25 | 25 | 30 | 35 | 40 | 40 | 45 | 50 | 50 | 55 | 60 | 60 | 65 | 70 | 75 | 75 | 80 | 85 | 85 | 85 | 85 |
| | 0 | 5 | 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | 95 | 100 |
| | 6/6 | | 6/9 | | 6/12 | | 6/18 | | 6/24 | | 6/30 | | 6/36 | | 6/48 | | 6/60 | | 3/60 | | Blind |
Monocular Assessement of Better Eye | |
In applying this table, if the veteran’s visual acuity in either eye is such that he or she is only capable of counting fingers or of perceiving the difference between light and darkness with that eye, then the veteran is to be taken as “blind” in the eye so affected. | |
| | | | | | | | | | | | | | | | | | | | | | | | | |
PART 8.2: OTHER OCULAR IMPAIRMENT
Other Impairment
Table 8.2.1 lists impairment ratings for a variety of ocular conditions. The ratings are based on the presence of symptoms and of inconvenience. Ratings from Table 8.2.1 are not to be combined with ratings from Table 8.1.3 for the same condition. If the same condition can be rated from both tables, the higher rating is to be chosen.
Other Impairment Table 8.2.1 | 
|
OCULAR IMPAIRMENT |
Impairment Ratings | Criteria |
NIL | Occasional conjunctivitis. |
TWO | Intermittent conjunctivitis - at least 6 separate episodes per year. |
FIVE | - Constant but mild irritation of eyes resulting in symptoms and signs, eg, chronic conjunctivitis or blepharoconjunctivitis, persistent photo-phobia, epiphora.
- Disorders resulting in dry eyes necessitating regular, daily use of eye drops.
- Uncorrected ectropion or entropion.
- Ptosis or tarsorrhaphy resulting in continuous but partial closure of the eye.
|
TEN | Symptoms and signs of severe eye irritation, present all of the time. |
Ratings from this table are not to be combined with ratings from Table 8.1.3 for the same condition. When the same condition can be rated from both tables, the higher rating is to be chosen. |
| | |
CHAPTER 9
RENAL AND URINARY TRACT FUNCTION
This chapter contains two parts:
INTRODUCTION
Renal function and urinary tract function are to be assessed separately. Only one rating is to be given for impairment of renal function. If appropriate, two ratings may be given for lower urinary tract conditions — one for conditions of urinary excretion and one for lower urinary tract infections.
Renal impairment is to be assessed under Tables 9.1.1 and 9.1.2. If an impairment may be assessed from both tables, the higher of the two is to be selected.
Loss of kidney function may also be assessed by applying Chapter 16 (Activities of Daily Living), which may sometimes be more appropriate than applying Table 9.1.1 and Table 9.1.2.
Calculation of the impairment rating for loss of renal function
Follow the steps below to calculate the impairment rating due to an accepted loss of renal function.
(Each step is elaborated in the following pages.)
STEP 1 | Determine a functional impairment rating for renal impairment by applying Table 9.1.1. | Page 143 |
STEP 2 | Determine an Other Impairment rating for renal impairment. | Page 144 |
STEP 3 | Compare the ratings obtained in Steps 1 and 2. Take the higher rating. | Page 144 |
STEP 4 | If the renal disease is causing generalised effects, apply Chapter 16 (Activities of Daily Living) to determine a rating. | Page 144 |
STEP 5 | If a rating has been obtained in Step 4, compare it with the rating obtained in Step 3. Take the higher rating. | Page 144 |
Step 1: Determine a functional impairment rating for renal impairment using Table 9.1.1.
Functional Loss Table 9.1.1 | 
|
LOSS OF RENAL FUNCTION |
Impairment Ratings | Criteria |
NIL | Normal or insignificantly impaired renal function. |
TWENTY | Chronic renal failure with creatinine clearance of less than 20 mL/min. |
THIRTY | Chronic renal failure with creatinine clearance of less than 10 mL/min. |
SIXTY | Ongoing peritoneal dialysis or haemodialysis. |
| Only one rating is to be selected from this table. |
| | |
Creatinine clearance may be estimated either by analysis of a 24 hour urine collection or from the serum creatinine level by applying the following formulae.
Males:
Creatinine clearance (mL/min) | = | (140–Age) × Weight (kg) 800 × Serum creatinine level (mmol/L) |
Females:
Creatinine clearance (mL/min) | = | (140–Age) × Weight (kg) × 0.85 800 × Serum creatinine level (mmol/L) |
Direct measurements of creatinine clearance are more accurate than estimates of creatinine clearance by applying the appropriate formulae. If both measurements are available that which better reflects the current status of the veteran’s health during the period of assessment is to be used.
Step 2: Determine an Other Impairment rating for renal impairment using Table 9.1.2.
Other Impairment Table 9.1.2 | 
|
RENAL OTHER IMPAIRMENT |
Impairment Ratings | Criteria |
NIL | - Glomerulonephritis, or other kidney disease, with good prognosis.
- Acute pyelonephritis with no current symptoms.
|
TWO | Asymptomatic renal stones. |
FIVE | - Nephrectomy.
- Glomerulonephritis likely to cause chronic renal failure in 5–10 years.
- Any disorder of upper urinary tract resulting in recurrent pyelonephritis, or hydronephrosis within past 12 months.
|
TEN | Glomerulonephritis likely to cause chronic renal failure in less than five years. |
TWENTY | - Renal transplant.
- Glomerulonephritis likely to progress to chronic renal failure in less than six months.
|
| Only one rating is to be selected from this table for any condition or combination of conditions. If more than one rating is applicable, the higher rating is to be selected. |
| | |
Step 3: Compare the ratings obtained in Steps 1 and 2. Take the higher rating.
Step 4: If the renal disease is causing generalised effects, apply Chapter 16 (Activities of Daily Living) to determine a rating.
Step 5: If a rating has been obtained in Step 4, compare it with the rating obtained in Step 3. Take the higher rating.
PART 9.2: LOWER URINARY TRACT FUNCTION
A rating for urinary excretion and one for lower urinary tract infections may be determined under this Part.
Calculation of the impairment rating for loss of lower urinary tract function
Follow the steps below to calculate the impairment rating due to an accepted loss of lower urinary function.
(Each step is elaborated in the following pages.)
STEP 1 | Determine an impairment rating for impairment of urinary excretion if appropriate by applying Table 9.2.1. | Page 145 |
STEP 2 | Determine an impairment rating for lower urinary tract infections impairment if appropriate. | Page 145 |
STEP 3 | If the lower urinary tract condition causes impairment of an intermittent nature, combine the ratings determined in Steps 1 and 2, by applying Chapter 18 (Combined Values Chart). | Page 146 |
STEP 4 | If the lower urinary tract condition causes impairment of an intermittent nature, determine a rating for the condition by applying Chapter 15 (Intermittent Impairment). | Page 146 |
STEP 5 | If the lower urinary tract condition causes impairment of an intermittent nature, compare the ratings obtained in Steps 3 and 4. Take the higher rating. | Page 146 |
Step 1: Determine an impairment rating for impairment of urinary excretion if appropriate by applying Table 9.2.1.
Step 2: Determine an impairment rating for lower urinary tract infections impairment if appropriate by applying Table 9.2.2.
The ratings obtained in Steps 1 and 2 are not to be compared or combined at this stage but are to be included in the final combining of all ratings, except if the condition causes impairment of an intermittent nature.
If the condition does not cause impairment of an intermittent nature, the assessment of an impairment rating for the condition ceases at this point. If the condition causes impairment of an intermittent nature, proceed to Step 3.
Step 3: If the lower urinary tract condition causes impairment of an intermittent nature, combine the ratings determined in Steps 1 and 2 by applying Chapter 18 (Combined Values Chart).
Step 4: If the lower urinary tract condition causes impairment of an intermittent nature, determine a rating for the condition by applying Chapter 15 (Intermittent Impairment).
Step 5: If the lower urinary tract condition causes impairment of an intermittent nature, compare the ratings obtained in Steps 3 and 4. Take the higher rating.
If the rating obtained in Step 3 is higher than that obtained in Step 4, the impairment rating obtained in Step 1 and the impairment rating obtained in Step 2 are to be included in the final combining of all impairment ratings.
Functional Loss Table 9.2.1 | 
|
URINARY EXCRETION |
Impairment Ratings | Criteria |
NIL | - Occasional stress incontinence; infrequent and small amounts of urine lost, and incontinence pad not needed.
- Mild symptoms of bladder outlet or urethral obstruction, eg. hesitancy, or poor stream.
|
FIVE | - Bladder outlet or urethral obstruction as above, but with more severe symptoms such as urge frequency, nocturia, or recurrent urinary tract infections.
- Minor stress incontinence, needing use of 1–2 incontinence pads a day.
- Mild urge incontinence, but rarely unable to find a toilet in time.
- Any disorder of lower urinary tract resulting in recurrent pyelonephritis, or hydronephrosis within past 12 months.
|
TEN | - Moderate stress incontinence, needing several incontinence pads a day.
- Urethral stricture, necessitating passage of sounds at internals of three months or less.
|
FIFTEEN | - Frequent and severe stress incontinence causing significant embarrassment and some avoidance of social activities and public places.
- Loss of voluntary control of bladder, but satisfactory emptying achieved by triggering of reflex activity, suprapubic pressure or Valsalva manoeuvre. No incontinence aid needed.
|
TWENTY | Loss of voluntary control of bladder necessitating intermittent catheterisation. |
THIRTY | - Urinary diversion, eg, ileal conduit, sigmoid conduit, ureterosigmoidostomy.
- Dribbling incontinence needing frequent change of incontinence pads, or a collection device, eg. condom catheter.
|
FORTY | |
| | |
Functional Loss Table 9.2.2 | 
|
LOWER URINARY TRACT INFECTIONS |
Impairment Ratings | Criteria |
NIL | Occasional urinary tract infections. |
FIVE | Recurrent cystitis causing frequent symptoms. |
| | |
CHAPTER 10
SEXUAL FUNCTION, REPRODUCTION, AND BREASTS
This chapter contains three parts:
Part 10.2 — Reproduction
Part 10.3 — Breasts
INTRODUCTION
Each part of this chapter contains separate tables for males and females. Ratings may be obtained from one or more parts, depending on the conditions to be assessed.
Many conditions of the female reproductive system, such as premenstrual tension and dysmenorhoea, occur on a cyclical basis and should be rated by applying Chapter 15 (Intermittent Impairment). When such conditions are successfully controlled by use of the contraceptive pill, a rating of zero is to be given.
It is also recognised that servicewomen may use the contraceptive pill to free themselves from such cyclical problems. In itself this is not a condition. However, if the use of the contraceptive pill causes significant side effects and if these side effects are accepted as being war-caused or defence-caused conditions, they should be rated from whatever section applies to them according to their nature.
Some conditions related to the reproductive organs, or to the effects of the sexual hormones, or which are more common in one sex than the other (such as osteoporosis), are not specifically mentioned in this chapter. Such conditions should be rated from the relevant part of the Guide according to their nature.
PART 10.1: SEXUAL FUNCTION
Calculation of the impairment rating for loss of sexual function
Follow the steps below to calculate the impairment rating due to an accepted loss of sexual function.
(Each step is elaborated in the following pages.)
STEP 1 | (Omit this step if you are assessing an accepted condition of a female veteran.) Determine a functional impairment rating for loss of sexual function from Table 10.1.1. | Page 149 |
STEP 2 | (Omit this step if you are assessing an accepted condition of a male veteran.) Determine a functional impairment rating for loss of sexual function from Table 10.1.2. | Page 150 |
STEP 3 | (Omit this step if you are assessing an accepted condition of a male veteran.) Determine a functional impairment rating for loss of sexual function from Table 10.1.3. | Page 150 |
Step 1: (Omit this step if you are assessing an accepted condition of a female veteran.) Determine a functional impairment rating for loss of sexual function in male veterans from Table 10.1.1.
Although impotence may be a symptom or effect of more than one accepted condition, only one rating is to be given for impotence.
The rating from Table 10.1.1 is the final rating for loss of sexual function in male veterans. The rating obtained from Table 10.1.1 is not to be compared or combined with any other rating at this stage, but is to be included in the final combining of all ratings.
Functional Loss Table 10.1.1 | 
|
SEXUAL FUNCTION: MALE |
Age at onset | Less than 30 | 30 to 39 | 40 to 64 | 65 to 74 | 75 to 84 | 85 and older |
Circumcision | 0 | 0 | 0 | 0 | 0 | 0 |
Scarring of penis | 2 | 2 | 2 | 2 | 2 | 2 |
Peyronie’s disease | 2 | 2 | 2 | 2 | 2 | 2 |
Impotence (not ameliorated by surgical treatment) | 25 | 20 | 15 | 10 | 5 | 2 |
Impotence (ameliorated by surgical treatment) | 15 | 15 | 10 | 5 | 2 | 0 |
Severe post-ejaculatory pain | 20 | 20 | 15 | 10 | 5 | 2 |
Loss of all or most of penis | 30 | 25 | 20 | 15 | 10 | 10 |
Loss of part of penis without significant interference with function | 5 | 5 | 5 | 5 | 5 | 5 |
| Only one rating is to be selected from this table. |
| | | | | | | | |
For the purposes of Table 10.1.1
“Impotence” means the persistent inability to attain an erection of sufficient strength to achieve intromission.
“Severe post-ejaculatory pain” means post-ejaculatory pain of such a degree as to cause complete or almost complete avoidance of sexual activity.
Step 2: (Omit this step if you are assessing an accepted condition of a male veteran.) Determine a functional impairment rating for loss of sexual function in female veterans from Table 10.1.2.
Functional Loss Table 10.1.2 | 
|
SEXUAL FUNCTION: FEMALE |
Impairment Ratings | Criteria |
NIL | Persistent inability to participate in vaginal intercourse onset at age 75 or older. |
FIVE | Persistent inability to participate in vaginal intercourse onset at age 65–74. |
TEN | Persistent inability to participate in vaginal intercourse onset at age 40–64. |
TWENTY | Persistent inability to participate in vaginal intercourse onset at age less than 40. |
TWENTY- FIVE | Persistent inability to participate in vaginal intercourse onset at age less than 30. |
| Only one rating is to be selected from this table. |
| | |
For the purposes of Table 10.1.2:
“persistent inability” means the woman is unable to participate in vaginal intercourse on most occasions because of physical obstruction of the vagina or its entrance or because of vaginismus or because of dyspareunia.
Ratings may be given from each of Tables 10.1.2 and 10.1.3 if appropriate. The rating obtained from Table 10.1.2 is not to be compared or combined with any other rating at this stage, but is to be included in the final combining of all ratings.
Step 3: (Omit this step if you are assessing an accepted condition of a male veteran.) Determine a functional impairment rating for loss of sexual function in female veterans from Table 10.1.3.
Functional Loss Table 10.1.3 | 
|
SEXUAL FUNCTION: FEMALE |
Impairment Ratings | Criteria |
NIL | No impairment of sexual sensation. |
TWO | Diminished sexual sensation. |
FIVE | Inability to achieve a climax at age less than 40. |
TEN | Inability to achieve a climax at age less than 30. |
| Clitoridectomy at age less than 40. |
FIFTEEN | Vulvectomy at age less than 40. |
TWENTY | Clitoridectomy at age less than 30. |
TWENTY- FIVE | Vulvectomy at age less than 30. |
| Only one rating is to be selected from this table. |
| | |
Ratings may be given from each of Tables 10.1.2 and 10.1.3 if appropriate. The rating obtained from Table 10.1.3 is not to be compared or combined with any other rating at this stage, but is to be included in the final combining of all ratings.
Calculation of the impairment rating for loss of reproductive function
Follow the steps below to calculate the impairment rating due to an accepted loss of reproductive function.
(Each step is elaborated in the following pages.)
STEP 1 | (Omit this step if you are assessing an accepted condition of a female veteran.) Determine a functional impairment rating for loss of reproductive function from Table 10.2.1. | Page 154 |
STEP 2 | (Omit this step if you are assessing an accepted condition of a male veteran.) | |
For the purposes of this chapter:
“infertility” means:
for females —
the condition in which a woman is unable to achieve a pregnancy resulting in a viable infant because of a gynaecological condition that prevents her becoming pregnant or maintaining a pregnancy to term; or
the situation of a woman who has been given medical advice that she should not become pregnant and who consequently does not give birth to a viable child either because of risk to her life; or the danger of seriously compromising her health; or serious and significant risk to the potential child. (The latter circumstance may arise if the woman has had radiotherapy for a malignant condition.)
for males —
the condition in which a man is unable to achieve a pregnancy in a woman.
“reduced fertility” means:
for females —
the situation of a woman who has sought medical help in order to become pregnant and who has been given such help in the form of IVF, GIFT, or a similar procedure or hormonal stimuli and who as a result of such procedures does become pregnant; or
the situation of a woman who has been advised that she is infertile and who, as a result, has adopted a child and who then, and only after that, has conceived.
(A woman is to be taken to be infertile if, despite such procedures, she remains unable to become pregnant. She will also be taken to be infertile until such time as she gives birth to a viable infant.)
for males —
the situation of a man who has sought medical help in order to enable him to father a child as a result of conditions such as a low sperm count or impotence or other related condition and who, with his partner, has been given such help in the form of IVF, GIFT, or a similar procedure or hormonal stimuli and who as a result of such procedures does succeed in becoming the biological father of a viable infant; or
the situation of a man who has been advised that he is infertile and who, as a result, with his partner, has adopted a child and who then, and only after that, has become the biological father of a viable infant in the normal way.
The impairment rating for reduced fertility is given to compensate veterans for the delay they and their partners will have incurred in starting their family as a result of waiting for investigations and in undergoing the procedures and for the stress of hormone therapy which places a considerable emotional stress on both partners and a specific physiological stress on the female.
The fertility problem should only be assessed as “infertility” under this Guide if it prevents the veteran from having children that the veteran would otherwise have had. It is for a medical practitioner to diagnose whether a fertility condition is present. The veteran must advise whether the fertility condition prevented the birth of a child that otherwise the veteran would have parented.
If the veteran is of the opinion that the fertility condition did not actually prevent the veteran from having a child, the condition is to be assessed at the same rate as reduced fertility.
Cervical incompetence is to be rated in the same way as are problems of fertility.
Step 1: (Omit this step if you are assessing an accepted condition of a female veteran.) Determine a functional impairment rating for loss of reproductive function in male veterans from Table 10.2.1.
Functional Loss Table 10.2.1 | 
|
REPRODUCTIVE FUNCTION: MALE |
Impairment Ratings | Criteria |
NIL | Varicocele or hydrocele, associated with no or negligible symptoms. |
TWO | Infertility with onset at age 55 or older. |
FIVE | - Varicocele or hydrocele sufficient to cause enlargement of scrotum, and daily symptoms.
- Loss of one testis at any age.
- Infertility with onset at age 45–54.
- Reduced fertility with onset at age less than 45.
|
TEN | - Infertility with onset at age less than 45.
- Loss of both testes at age 45 or older.
|
FIFTEEN | - Loss of both testes at age 31 to 45.
- Infertility with onset at age 30 or less.
|
TWENTY | Loss of both testes at age 30 or less. |
| Only one rating is to be selected from this table. |
| | |
This is the final rating for loss of reproductive function in male veterans. The rating obtained from Table 10.2.1 is not to be compared or combined with any other rating at this stage, but is to be included in the final combining of all ratings.
While impotence would render it difficult for a man to father a child in the normal way, it would neither necessarily nor usually render him infertile.
Step 2: (Omit this step if you are assessing an accepted condition of a male veteran.) Determine a functional impairment rating for loss of reproductive function in female veterans from Table 10.2.2.
Functional Loss Table 10.2.2 | 
|
REPRODUCTIVE FUNCTION: FEMALE |
Impairment Ratings | Criteria |
NIL | - Elective tubal ligation.
- Infertility with onset at or after natural menopause.
|
TWO | - Amenorrhoea in a pre-menopausal woman.
- Infertility with onset at age 45 or older in a pre-menopausal woman.
|
FIVE | - Reduced fertility with onset at age less than 45 in a pre-menopausal woman.
- Removal of one ovary at age less than 45.
- Recurrent salpingitis.
- Cervical incompetence.
- Endometriosis.
- Severe menorrhagia.
|
TEN | - Infertility with onset at age less than 45 in a pre-menopausal woman.
- Removal of ovaries without hysterectomy at age less than 45.
|
FIFTEEN | - Hysterectomy without removal of ovaries at age less than 45.
- Infertility with onset at age 30 or less in a pre-menopausal woman.
|
TWENTY | Hysterectomy with removal of ovaries at age less than 45. |
| Only one rating is to be selected from this table. |
| | |
Amenorrhoea by itself is to be rated at 2 points. However amenorrhoea will generally be a symptom of some other condition, such as infertility, in which case a rating is to be given for infertility and that rating is to be compared with the rating for amenorrhoea. The higher rating is to be taken.
Endometriosis may be assessed by applying Table 10.2.2, or by assessment of its effect on fertility or sexual function, or by applying Chapter 15 (Intermittent Impairment). If ratings are given from both this chapter and Chapter 15, the ratings are to be compared and the higher is to be taken.
This is the final rating for loss of reproductive function in female veterans. The rating obtained from Table 10.2.2 is not to be compared or combined with any other rating at this stage, but is to be included in the final combining of all ratings.
For those conditions of the female reproductive system that occur on a cyclical basis, Chapter 15 (Intermittent Impairment) is to be applied.
A rating given for mastectomy under this Part is not the final rating for cancer of the breast. The steps to be followed in assessing cancer of the breast are given below, for convenience. In following these steps it is essential to apply both Chapter 14 and the tables in this Part.
Calculation of the impairment rating for cancer of the breast
Follow the steps below to calculate the impairment rating due to breast cancer.
Steps 2 to 6 are elaborated in Chapter 14 (Malignant Conditions).
STEP 1 | Find the applicable rating for the relevant mastectomy or other surgical procedure (Tables 10.3.1 or 10.3.2). |
STEP 2 | Determine any applicable ratings for other effects of surgery (for example, effects on the use of the arm). |
STEP 3 | Determine any applicable ratings for the effects of any chemotherapy or radiotherapy. |
STEP 4 | Determine any applicable ratings due to the effects of spread of the cancer. |
STEP 5 | Combine all the above ratings by applying Chapter 18 (Combined Values Chart). |
STEP 6 | Find the applicable rating from Chapter 14 (Malignant Conditions). |
STEP 7 | Compare the rating obtained in Step 5 with the rating obtained in Step 6. Take the higher rating. This is the final rating for cancer of the breast. |
Functional Loss Table 10.3.1 | 
|
BREASTS: FEMALE |
Impairment Ratings | Criteria |
NIL | No significant breast condition. |
FIVE | - Persistent mammary discharge.
- Total loss of sensation of one nipple.
- Partial bilateral loss of sensation over T4&5 dermatome.
- Lumpectomy.
- Partial unilateral mastectomy.
|
TEN | - Total loss of sensation of both nipples.
- Total bilateral loss of sensation over T4&5 dermatome.
|
FIFTEEN | Unilateral mastectomy. |
THIRTY | Bilateral mastectomy. |
| Only one rating is to be selected from this table. |
| | |
Functional Loss Table 10.3.2 | 
|
BREASTS: MALE |
Impairment Ratings | Criteria |
NIL | No significant breast condition. |
TWO | - Gynaecomastia.
- Unilateral mastectomy.
|
FIVE | - Persistent mammary discharge.
- Bilateral mastectomy.
|
| Only one rating is to be selected from this table. |
| | |
CHAPTER 11
SKIN IMPAIRMENT
INTRODUCTION
This chapter is to be applied in assessing skin conditions. Chapter 17 (Disfigurement and Social Impairment) is also to be applied to the assessment of skin conditions if appropriate.
For any relatively minor skin condition, the major consideration is whether it occurs on a more or less permanent basis or whether it occurs intermittently. If the condition occurs on an intermittent basis, the application of Chapter 15 (Intermittent Impairment) is to be considered.
For a more noticeable skin condition, consideration must also be given to whether it affects function or causes disfigurement. If the skin condition is responsible for a discrete loss of function in another system, the appropriate system-specific table is to be applied. For example, if there were loss of hand function as the result of a skin condition, Chapter 3 (Spine and Limbs) is to be applied.
For very severe skin conditions, loss of function is generally measured by reference to the whole person and may need to be rated under Table 16.2 in Chapter 16 (Activities of Daily Living).
Other Impairment (Table 11.1)
Table 11.1 lists specific impairment ratings for a variety of skin conditions based on inconvenience. One rating only is to be made from this table for any combination of conditions. When more than one criterion is applicable, that associated with the higher rating is chosen.
Impairment ratings from Table 11.1 are not to be combined with ratings from tables for loss of function for the same condition. If ratings can be made from more than one table the higher rating is to be chosen.
Reference to disfigurement is found in Chapter 17 (Disfigurement and Social Impairment).
Calculation of the impairment rating for skin conditions
Follow the steps below to calculate the impairment rating from accepted skin conditions:
(Each step is elaborated in the following pages.)
STEP 1 | Establish whether the skin condition causes any loss of function. | Page 159 |
STEP 2 | (Omit this step if is there is no relevant functional impairment.) Calculate the total functional impairment due to any accepted skin condition. | Page 159 |
STEP 3 | Calculate the Other Impairment rating for the accepted skin condition by applying Table 11.1. | Page 159 |
STEP 4 | (Omit this step if there is no relevant functional impairment.) Compare the impairment rating obtained in Step 2 with the impairment rating obtained in Step 3. Take the higher rating. | Page 159 |
Step 1: Establish whether the skin condition causes any loss of function.
Skin conditions may cause loss of function of hands by interfering with movement or sensation. They may cause loss of function of joints as a result of scarring and contractions which may limit or interfere with the movement at the joint. Skin conditions may cause conditions of the eyelids (for example, ectropion or entropion, or difficulties in closing or opening the eyes).
If any such effect of the accepted skin condition exists, this should be confirmed before applying Table 11.1.
Step 2: Calculate the impairment rating for the total functional loss from any accepted skin condition.
Depending on its nature and extent, functional loss may be assessed by:
- applying Chapter 16 (Activities of Daily Living);
- applying Chapter 15 (Intermittent Impairment), or
- applying one or more system specific tables.
The rating obtained from the table applied in assessing functional loss may need to be modified by:
- applying Chapter 19 (Partially Contributing Impairment) if there is some contribution from a non-accepted condition; or
- applying Chapter 20 (Apportionment) if there is some contribution from another accepted condition.
If ratings from Chapter 16, Chapter 15 and one or more system specific tables are possible, all three are not to be given. Instead, all attributable system specific ratings are to be combined and compared with any attributable rating from Chapter 16 and from Chapter 15. The veteran is to be given the highest of the attributable ratings from Chapter 16, Chapter 15 or the combined system specific ratings as the functional impairment rating for accepted skin conditions.
Step 3: Establish the Other Impairment rating for the accepted skin condition using Table 11.1.
Only one rating is to be given from Table 11.1 for any condition or combination of conditions.
Step 4: Compare the impairment rating obtained in Step 2 with the impairment rating obtained in Step 3. Take the higher rating.
This step determines the final impairment rating for accepted skin conditions.
At Step 2 allowance was made for the effect of any non-accepted skin condition and of any accepted condition which is not a skin condition on the functional loss from the accepted skin conditions. Compare the result obtained in Step 2 with the result obtained in Step 3. Take the higher of the two ratings. This is the final impairment rating for the accepted skin condition.
Other Impairment Table 11.1 | 
|
SKIN DISORDERS |
Impairment Ratings | Criteria |
NIL | - Skin disorder causing symptoms which are easily tolerated, or are present only for a short time each day.
- Skin disorder that is symptomatic for less than one week of the year.
- Asymptomatic skin disorder without need for medication.
- Solar skin lesions not requiring removal during the year.
- Male pattern baldness.
|
TWO | - Skin disorder than is symptomatic for less than four months of the year.
- Asymptomatic skin disorder but with need for medication.
- Solar skin lesions necessitating surgical removal (including cryotherapy and/or cautery) at least once in the year but less than four times a year.
|
FIVE | - Any skin disorder, or combination of disorders, causing symptoms that are not easily tolerated, and that are present for a significant part of the day for at least four months a year, eg. Psoriasis; eczema; tinea with persistent pruritus, despite treatment.
- Noticeable skin disorder, or combination of disorders, on face or hands, of such degree as would cause embarrassment to most people in unfamiliar social contexts.
- Visible skin disorder, or combination of disorders, on a part of the body other than face and hands, of such degree as would cause embarrassment or considerable inconvenience to most people in domestic or intimate situations or as would cause them to curtail sporting or recreational activities.
- Solar skin lesions necessitating surgical removal (including cryotherapy and/or cautery) three times a year or more, or the removal of at least ten lesions over the year.
- Alopecia (other than male pattern baldness).
|
TEN | - Skin disorders, or combination of disorders, resulting in significant loss of structural integrity of face, eg. total loss of pinna, skin graft, scar following trauma or burns.
- Severe and persistent pruritus causing difficulty in concentrating and loss of sleep.
- Persistent skin disorder, or combination of disorders, resulting in continuous signs and significant symptoms of moderate degree, present for most of the time.
|
FIFTEEN | - Permanent or persistent skin disorder or combination of disorders causing gross loss of structural integrity of face and extensive or extreme facial disfigurement.
- Severe and persistent ulcerative, weeping or suppurative skin disorders involving the greater part of both the face and the hands.
|
| Only one rating is to be selected from this table for any combination of conditions. |
| | |
CHAPTER 12
ENDOCRINE AND HAEMOPOIETIC IMPAIRMENT
This chapter contains two parts:
Part 12.1 — Loss of Endocrine Function
INTRODUCTION
Part 12.1 is to be applied to assess loss of function of the endocrine system. The endocrine system consists of all the glands and tissues which secrete hormones and the mechanisms by which the secretion of those hormones is regulated. The functions of the endocrine system are very diverse and include control of growth, of sexual function, of calcium metabolism and of the uptake of glucose by body cells.
Part 12.2 is to be applied to assess loss of haemopoietic function. The haemopoietic system consists of all the tissues, such as bone marrow and lymph nodes, that produce blood cells.
PART 12.1: THE ENDOCRINE SYSTEM
Many endocrine conditions will affect various other body systems. Hence, loss of endocrine function is established by assessing the effect of the condition on those other body systems. In very severe cases, where many body systems are affected, Table 16.2 in Chapter 16 (Activities of Daily Living) is to be applied to rate the loss of function.
In many cases, an endocrine condition will be under therapeutic control as a result of the use of continuous replacement therapy or the like. In these cases, the effect on other body systems may be minimal and the veteran’s principal inconvenience is that of undergoing the continuous therapy. This is to be assessed by applying the Other Impairment tables.
Calculation of the impairment rating for loss of endocrine function
Follow the steps below to calculate the impairment rating due to accepted loss of endocrine function.
(Each step is elaborated in the following pages.)
STEP 1 | Establish which body systems are affected by the accepted endocrine condition. | Page 162 |
STEP 2 | Determine an impairment rating for functional impairment of the affected body systems. | Page 162 |
STEP 3 | Determine an Other Impairment rating for the accepted endocrine condition. | Page 162 |
STEP 4 | Compare the total functional impairment rating of the affected body systems with the rating obtained in Step 3. Take the higher rating. | Page 162 |
STEP 5 | If recognisable episodes of increased impairment are superimposed on the underlying condition, also assess the endocrine condition under Chapter 15 (Intermittent Impairment). | Page 162 |
Step 1: Establish which body systems are affected by the accepted endocrine condition.
Many of the effects of loss of endocrine function are separate and recognisable diseases. For example, diabetes mellitus may lead to ischaemic heart disease. Such diseases, though quite possibly a consequence of the loss of endocrine function, are to be separately assessed under this Guide and are not to be taken into account in the calculation of the impairment rating for loss of endocrine function.
Step 2: Determine an impairment rating for functional impairment of the affected body systems.
Use the appropriate Functional Loss tables from other chapters in this Guide to determine the impairment rating.
Step 3: Determine an Other Impairment rating for the accepted endocrine condition.
There are two Other Impairment tables for loss of endocrine function. Table 12.1.1 is to be applied if assessing diabetes mellitus, while Table 12.1.2 is be applied if assessing any other endocrine condition. Both tables provide an impairment rating based on the type of treatment required by the veteran.
Step 4: Compare the total functional impairment rating of the affected body systems with the rating obtained in Step 3. Take the higher of these two ratings.
The rating obtained in Step 4 is to be included in the final combining of all ratings.
Step 5: If recognisable episodes of increased impairment are superimposed on the underlying condition, also assess the endocrine condition under Chapter 15 (Intermittent Impairment).
If recognisable episodes of increased impairment are superimposed on the underlying condition (for example, insulin-dependent diabetes with superimposed hypoglycaemic episodes), the endocrine condition is to be assessed under Chapter 15 (Intermittent Impairment). The rating from Chapter 15 and the rating obtained in Step 4 are to be included in the final combining of all ratings.
However, a rating from Chapter 15 is not to be combined with a rating from any other system-specific table for the same condition.
Other Impairment Table 12.1.1 | 
| |
DIABETES MELLITUS | |
Impairment Ratings | Criteria | |
NIL | Glycosuria or hyperglycaemia controlled by weight loss. | |
TWO | Gestational diabetes mellitus. | |
FIVE | - Diabetes mellitus necessitating dietary control.
| |
| - Diabetes mellitus controlled by use of oral hyperglycaemics.
| |
TEN | Diabetes mellitus controlled with insulin. | |
TWENTY | Diabetes mellitus uncontrolled. | |
| A rating from this table is to be selected when the endocrine disorder is not associated with loss of function. If an assessable loss of function occurs in another system the higher rating is to be chosen. The two are not to be combined. |
| | | |
For the purposes of Table 12.1.1, “Diabetes mellitus uncontrolled” means blood sugar level consistently 15 mmol/L or more, despite treatment.
Other Impairment Table 12.1.2 | 
|
ENDOCRINE DISORDERS (excluding Diabetes Mellitus) |
Impairment Ratings | Criteria |
NIL | An endocrine disorder controlled by regular oral medication taken less often than daily or by injections less often than once a month. |
TWO | - An endocrine disorder requiring daily oral medication.
- An endocrine disorder requiring regular injections not more often than once a month.
|
FIVE | An endocrine disorder requiring injections not more often than once a fortnight. |
TEN | An endocrine disorder requiring daily injections. |
| A rating from this table is to be selected when the endocrine disorder is not associated with loss of function. If an assessable loss of function occurs in another system the higher rating is to be chosen. The two are not to be combined. |
| | |
PART 12.2: THE HAEMOPOIETIC SYSTEM
Conditions of the haemopoietic system include anaemias, leukaemias and polycythaemia.
Haemopoietic conditions usually affect various other body systems, therefore loss of function for the condition is to be established by assessing the effect of the condition on those body systems. Some haemopoeitic conditions are also malignant conditions and may be assessed by applying Chapter 14 (Malignant Conditions). For very severe haemopoietic conditions, where many body systems are affected, Tables 16.1 and 16.2 in Chapter 16 (Activities of Daily Living) are also to be applied to rate the loss of function.
Many anaemias will respond adequately to replacement or supplemental therapy. For example, the hypochromic anaemia of iron deficiency will usually respond to dietary iron supplementation and pernicious anaemia will usually respond to parenteral Vitamin B12.
Calculation of the impairment rating for loss of haemopoietic function
Follow the steps below to calculate the impairment rating due to accepted loss of haemopoietic function:
(Each step is elaborated on the following page.)
STEP 1 | Establish which body systems are affected by the accepted haemopoietic condition. | Page 164 |
STEP 2 | Determine the impairment rating for functional impairment of the affected body systems. | Page 164 |
STEP 3 | Determine the impairment rating for the treatment requirements of the haemopoietic condition by applying Table 12.2.1. | Page 165 |
Step 1: Establish which body systems are affected by the accepted haemopoietic condition.
Haemopoietic conditions may affect the function of other body systems. For example, refractory anaemia may result in reduced effort tolerance.
Step 2: Determine the functional impairment of all body systems affected by the haemopoietic condition.
Apply the appropriate functional impairment table elsewhere in this Guide to assess the functional impairment arising from the haemopoietic condition. For example, in the case of refractory anaemia causing reduced effort tolerance, the reduced effort tolerance is to be assessed by use of the Effort Tolerance protocol in Chapter 1.
If non-accepted conditions have contributed to the impairment rating for any of the affected body systems, Chapter 19 (Partially Contributing Impairment) is to be applied.
The various functional impairment ratings are not combined at this stage but are to be included in the final combining of all impairment ratings.
Step 3: Determine the impairment rating for the treatment requirements of the accepted haemopoietic condition using Table 12.2.1.
The ratings obtained in Steps 2 and 3 are not to be combined at this stage but both are to be included in the final combining of all impairment ratings.
Other Impairment Table 12.2.1 | 
|
THE HAEMOPOIETIC SYSTEM: TREATMENT REQUIREMENTS* |
Impairment Ratings | Criteria |
NIL | Symptoms in remission and no active therapy indicated. |
TWO | Transfusion requirements: 2–3 units per 12–16 weeks. |
FIVE | - Intermittent combination cytotoxic therapy — one course every 3–4 weeks.
- Phlebotomy once every 4 weeks.
- Transfusion requirements: 2–3 units per 6 weeks.
|
TEN | - Phlebotomy more than once every 4 weeks.
- Transfusion requirements: 2–3 units per 4 weeks.
|
TWENTY | Transfusion requirements: 2–3 units per 2 weeks. |
| (*Additional to relevant body system assessment.) |
| | |
Part B: Non-System Specific Assessment
CHAPTER 13
NEGLIGIBLE IMPAIRMENT
INTRODUCTION
As every accepted condition is to be assessed, Table 13.1 provides a convenient method of rating any accepted condition which causes negligible impairment. Table 13.1 is to be applied only to conditions that cannot be conveniently classified under other chapters of this Guide and that would not attract a higher rating if they were classified under such chapters.
Determine the impairment rating for an accepted condition that causes negligible impairment
Follow the step below to calculate the negligible impairment due to an accepted condition.
Functional Loss Table 13.1 | 
|
NEGLIGIBLE IMPAIRMENT |
Impairment Rating | Criteria |
NIL | - An infectious disease from which the veteran has recovered with negligible after effects.
- An injury from which the veteran has recovered with negligible after effects.
- A condition causing no current impairment.
- condition from which the veteran has recovered with negligible after effects.
|
| | |
CHAPTER 14
MALIGNANT CONDITIONS
INTRODUCTION
Malignant conditions may affect one or more body systems.
Hence, any malignant condition can potentially be assessed by the following methods:
- by applying the system-specific tables contained in Chapters 1 to 12. A number of those tables may have to be consulted if the malignant condition causes multiple losses of function;
- by applying Chapter 14 which relates specifically to malignancies and which contains both a Functional Loss table and an Other Impairment table. These tables are designed to rate the malignant condition as a whole. The first table relates to loss of function in a general sense. The second table relates to reduced life expectancy which is regarded as an Other Impairment.
If the impairment rating from Chapter 14 is 70 points on the basis of either the malignant disorders functional table (Table 14.1) or the malignant disorders Other Impairment table (Table 14.2), there is no need to follow the steps set out in the following pages. If the rating from Chapter 14 is below 70 points, the steps are to be followed.
Determine the impairment rating for an accepted malignant condition
Follow the steps below to calculate the impairment due to an accepted malignant condition.
(Each of these steps is elaborated in the following pages.)
STEP 1 | Establish which body systems are affected by the malignant condition. | Page 168 |
STEP 2 | Determine the functional impairment ratings for the affected body systems. | Page 168 |
STEP 3 | Determine the total combined impairment rating for the various body system impairments attributable to the malignant condition. | Page 168 |
STEP 4 | Determine the impairment rating based on Table 14.1 (Malignant Disorders). | Page 168 |
STEP 5 | Determine the impairment rating based on Table 14.2 (Life Expectancy). | Page 169 |
STEP 6 | Compare the ratings obtained in Steps 4 and 5. Take the higher rating. | Page 170 |
STEP 7 | Compare the ratings obtained in Steps 3 and 6. Take the higher rating. | Page 170 |
STEP 8 | If the rating obtained in Step 3 is higher than that obtained in Step 6, separate the components of the rating obtained in Step 3 so that each can be included in the final combining of all ratings. | Page 171 |
Step 1: Establish which body systems are affected by the malignant condition.
Before a malignant condition is assessed, information regarding the extent of the condition must be available. Such information includes the site of the primary, the sites of any secondaries, the effects of any surgery and the effects of any radiotherapy or chemotherapy.
From that information the affected body systems can be established and the applicable chapters of this Guide applied.
For example, in the case of an accepted carcinoma of the rectum, there may be surgical resection of the rectum with a colostomy, secondary spread of the cancer to the lungs and spine, and radiotherapy with some resultant digestive disturbances. In such a case, Chapters 1, 3, and 6 of this Guide will have to be applied in Step 1 to arrive at an appropriate functional impairment rating.
Step 2: Determine the functional impairment ratings for the affected body systems.
Depending on the body systems that are affected by the malignant condition and its treatment, each of the relevant chapters of the Guide is to be used and appropriate ratings obtained.
If other accepted or non-accepted conditions also affect any of the same body systems, Chapter 19 (Partially Contributing Impairment) or Chapter 20 (Apportionment) may have to be applied depending upon the circumstances.
Step 3: Determine the total combined impairment rating for the various body system impairments attributable to the malignant condition.
The total combined impairment rating for the various body system impairments associated with the malignant condition is determined by combining the attributable impairment ratings by applying Chapter 18 (Combined Values Chart).
Unless the malignant condition is the only accepted condition, this combined rating is to be regarded as an intermediate rating only.
Step 4: Determine the impairment rating based on Table 14.1 (Malignant Disorders).
Apply Table 14.1 and find the relevant impairment rating for the entire set of effects which have arisen from the malignant disorder treatment, including surgical resection, chemotherapy and radiotherapy.
For the purposes of Table 14.1, “symptoms” encompasses the symptoms of both the malignant condition itself and the symptoms of the effects of its treatment.
If non-accepted conditions or accepted but non-malignant conditions have contributed to the impairment rating obtained from Table 14.1, Chapter 19 (Apportionment) or Chapter 20 (Partially Contributing Impairment) are to be applied depending on the circumstances of the case.
Step 5: Determine the impairment rating based on life expectancy.
If an impairment rating has not been determined on any previous occasion by applying Table 14.2 (Life Expectancy) or its predecessor in an earlier edition of this Guide, a rating is to be obtained from Table 14.2. If a rating has been obtained from Table 14.2 or its predecessor in an earlier edition of this Guide, on a previous occasion, that same rating is to be applied again in all further assessments of the condition.
Whenever possible, the rating from Table 14.2 is to be based on an estimate from an oncologist or other treating specialist of the veteran’s survival. If such information is unavailable, data from standard reference texts is to be applied to provide an estimate. Such an estimate is to be based on malignancies of the same type and degree of spread as that affecting the veteran.
Estimated life expectancy is projected from the time of diagnosis, or from any subsequent major staging procedure or operation. Thus, once a rating from Table 14.2 has been made it is not to be changed, unless subsequent findings indicate that the earlier prognosis was based on incorrect clinical information.
If the assessment is made posthumously, the rating from Table 14.2 is not to be modified to reflect the actual duration for which the veteran survived after diagnosis. The table is only to be used for predicted probability of survival.
Ratings from Table 14.2 are not to be updated to account for the natural progression of the disease. However, it is expected that ratings from Table 14.2 will come to be exceeded by ratings from Table 14.1 during this time.
Ratings from Table 14.2 are not to be reduced because of favourable response to treatment, or because of better than expected survival. However, if the condition is being rated for the first time more than five years after diagnosis, and the disorder is in remission or appears to be cured, the impairment rating from this table is not to exceed ten.
If the veteran has more than one malignant condition accepted, Table 14.2 is to be applied to each condition. Table 14.2 is not to be applied to a recurrence of an old (already diagnosed) condition.
Functional Loss Table 14.1 | 
|
MALIGNANT DISORDERS |
Impairment Ratings | Criteria |
NIL | Minor symptoms that are easily tolerated. |
TEN | Mild to moderate symptoms that are irritating or unpleasant but rarely prevent completion of any activity. Symptoms may cause loss of efficiency in some activities. |
TWENTY | More severe symptoms that are more distressing but prevent few everyday activities. Loss of efficiency is discernible in a good few activities. Self-care is unaffected and independence is retained. |
THIRTY-FIVE | Loss of efficiency discernible in many everyday activities. Some elements of self-care are restricted but, in most respects, independence is retained. |
FIFTY | Major restrictions in many everyday activities. Capacity for self-care is increasingly restricted, leading to partial dependence on others. |
SEVENTY | Most everyday activities are prevented. Dependent on others for most kinds of self-care. Able to be maintained at home with considerable assistance and frequent medical care. |
| | |
Functional Loss Table 14.2 | 
|
LIFE EXPECTANCY |
Impairment Ratings | Predicted Survival at the Time of Diagnosis or Staging Procedure |
NIL | Normal, or near-normal, five year survival. |
TEN | Five year survival less than 75% of normal. |
TWENTY | Five year survival less than 50% of normal. |
THIRTY-FIVE | Five year survival less than 25% of normal. |
FIFTY | One year survival less than 50% of normal. |
SEVENTY | One year survival less than 25% of normal. |
| | |
Step 6: Compare the ratings obtained in Steps 4 and 5. Take the higher rating.
The higher of these two ratings will be the rating for the malignant condition on the basis of this chapter.
Step 7: Compare the ratings obtained in Steps 3 and 6. Take the higher rating.
If the rating obtained in Step 3 is higher than that obtained in Step 6, go to Step 8.
If the rating obtained in Step 6 is higher than that obtained in Step 3, then the rating obtained in Step 6 becomes the final rating for the malignant condition and is to be included in the final combining of all ratings.
Step 8: If the rating obtained in Step 3 is higher than the rating obtained in Step 6, separate the components of the rating obtained in Step 3 so that each can be included in the final combining of all impairment ratings.
For example, in the case of an accepted carcinoma of the rectum postulated under Step 1, each of the ratings from Chapters 1, 3, and 6 of the Guide is to be separately included in the final combining of all impairment ratings.
CHAPTER 15
INTERMITTENT IMPAIRMENT
INTRODUCTION
Intermittent disorders are conditions:
- that remain at a low level of impairment between discrete episodes of increased impairment;
or
- where there is one basic type of impairment on which is superimposed episodes of significantly greater impairment of another type.
A sufferer from epilepsy who remains well between “fits” exemplifies the first type of intermittent disorder. A sufferer from Menière’s disease whose condition is characterised by deafness and occasional episodes of vertigo exemplifies the second type of intermittent disorder. The deafness may be regarded as the basic type of impairment and the episodes of vertigo may be regarded as the superimposed intermittent impairment. Both elements of the condition are to be assessed.
In this chapter, “attacks” refers to the episode may increased or superimposed impairment. Attacks are to be categorised by reference to their severity, duration and frequency:
- “severity of an attack” refers to the degree to which self-care and normal everyday activities are disrupted by the attack;
- “duration of an attack” refers to the average length of time for which an attack lasts, that is, seconds, minutes, hours or days; and
- “frequency of an attack” refers to the number of affected days in a year.
Intermittent disorders are also disorders that affect one or more body systems. For example, asthma is both an intermittent condition and a cardio-respiratory condition. Hence, potentially, any intermittent disorder can be assessed by either of two methods:
- by applying the system-specific tables contained in Chapters 1 to 12. Several of those tables should be used if the intermittent disorder causes multiple losses of function; or
- by applying this chapter.
In practice, except where the intermittent nature of the condition clearly overwhelms its system specific effects or vice versa, both methods are to be applied for rating the intermittent condition and the higher of those two ratings taken as the final rating for the intermittent condition.
Calculation of the impairment rating for an accepted intermittent condition
Follow the steps below to calculate the impairment rating due to an accepted intermittent condition:
(Each of these steps is elaborated in the following pages.)
STEP 1 | Establish which body systems are affected by the intermittent condition. | Page 173 |
STEP 2 | Determine the functional impairment ratings for the intermittent condition. | Page 173 |
STEP 3 | Determine the total combined impairment rating for the various body system impairments attributable to the intermittent condition. | Page 173 |
STEP 4 | Determine whether the attacks are of one or more significant types and group them accordingly. | Page 174 |
STEP 5 | Determine the rating for intermittent attack severity. | Page 174 |
STEP 6 | Determine the rating for the intermittent attack duration. | Page 174 |
STEP 7 | Determine the intermittent grading code for the intermittent attack. | Page 175 |
STEP 8 | Determine the impairment rating for the intermittent attack by reference to the number of affected days per year. | Page 175 |
STEP 9 | Compare the impairment ratings obtained in Step 3 and Step 8. Take the higher rating. | Page 176 |
STEP 10 | Determine the rating for the impairment resulting from the avoidance or preclusion of otherwise normal activities between attacks. | Page 176 |
Step 1: Establish which body systems the intermittent condition affects.
Before an intermittent condition is assessed, information regarding the extent of the condition must be available. From that information, the affected body systems are to be established and the applicable chapters of this Guide applied.
Step 2: Determine the functional impairment ratings attributable to the intermittent condition for each affected body system.
Use the relevant chapters and determine the appropriate rating.
Chapter 19 (Partially Contributing Impairment) or Chapter 20 (Apportionment) may also have to be applied to allow for the effect of other accepted conditions or non-accepted conditions respectively.
Step 3: Determine the total combined impairment rating for the various body system impairments attributable to the intermittent condition.
Combine the attributable impairment ratings obtained in Step 2 by applying Table 18.1 (Combined Values Chart) in Chapter 18.
The combined value so obtained is for use only in Step 9.
Step 4: Determine whether the attacks are of one or more significant types and group them accordingly.
If attacks vary in severity, duration or frequency, an average for each parameter is to be established except when the attacks fall naturally and very clearly into groups. In such cases separate the attacks into one or other of these groups. Determine the average severity, duration and frequency of the attacks in each group.
Perform the following four steps separately for each identified group of attacks.
Step 5: Determine the rating level for intermittent attack severity using Table 15.1.
Table 15.1 | 
|
INTERMITTENT ATTACK SEVERITY |
Level | Criteria |
0 | Minor symptoms that are easily tolerated. |
I | Mild to moderate symptoms that are irritating or unpleasant but that rarely prevent completion of any activity. Symptoms may cause loss of efficiency in some activities. |
II | More severe symptoms, that are distressing, but prevent few everyday activities. Loss of efficiency is discernible elsewhere. Self-care is unaffected and independence is retained. |
III | Loss of efficiency is discernible in many everyday activities. Some elements of self-care are restricted but, in most respects, independence is retained. Bed-rest is often necessary during an attack. |
IV | Major restrictions in many everyday activities. Capacity for self-care is increasingly restricted, leading to partial dependence on others. |
V | Most everyday activities are prevented. Dependent on others for many kinds of self-care. Able to be maintained at home only with considerable difficulty, or hospital admission is required. |
VI | Total incapacity. Unconscious or delirious. Self-care is impossible. |
| | |
Ratings are based on the activities that the veteran is physically unable to perform. For conditions in which it is common practice to lie down during attacks, it may be inappropriate to rate at level III if symptoms are mild and cause little restriction to activity.
Attacks of some intermittent conditions necessitate hospital admission. Hospital admissions commonly, but not invariably, call for level V or VI rating. It is important to rate self-care capacity. To be rated at Level V severity, a condition must render the veteran incapable of caring for himself or herself.
Hospital admission for surgery is not to be used as a basis for ratings from Table 15.1.
Step 6: Determine the rating for duration of the intermittent attacks using Table 15.2.
Attacks that last for more than 24 hours are to be classified as prolonged for the purposes of Table 15.2. Because they affect the veteran for more than one day per attack, the number of affected days per year will be greater than the number of attacks.
Table 15.2 | 
|
INTERMITTENT ATTACK DURATION |
Description | Duration |
Transient | Lasting up to and including five minutes. |
Short | Lasting more than five minutes but less than 30 minutes. |
Medium | Lasting from 30 minutes to four hours. |
Prolonged | Lasting more than four hours. |
| | |
Step 7: Determine the intermittent grading code for the intermittent attack using Table 15.3.
Table 15.3 | 
|
INTERMITTENT GRADING CODE |
Description | Severity Level |
| | 0 | I | II | III | IV | V | VI |
Transient | | A | A | A | B | C | C | F |
Short | | A | A | C | C | D | E | H |
Medium | | A | B | C | D | E | H | I |
Prolonged | | A | C | D | F | G | I | J |
| | | | | | | | | |
Step 8: Determine the impairment rating for the intermittent attack by reference to the number of affected days per year and by using Table 15.4.
Using the intermittent grading code determined in Step 7, determine the impairment rating appropriate to the intermittent grading code and frequency by applying Table 15.4.
Functional Loss Table 15.4 | 
|
INTERMITTENT IMPAIRMENT |
Frequency (affected days/year) |
| 2+ | 5+ | 10+ | 20+ | 40+ | 70+ | 100+ |
Intermittent Grading Code | Impairment Rating |
A | – | – | – | – | – | 2 | 2 |
B | – | – | – | – | 2 | 5 | 5 |
C | – | – | – | 2 | 5 | 10 | 10 |
D | – | – | 2 | 5 | 10 | 15 | 20 |
E | – | – | 2 | 5 | 10 | 20 | 30 |
F | – | 2 | 5 | 5 | 10 | 20 | 30 |
G | – | 2 | 5 | 10 | 20 | 25 | 30 |
H | – | 2 | 5 | 10 | 30 | 40 | 50 |
I | 2 | 5 | 10 | 30 | 50 | 60 | 70 |
J | 5 | 10 | 20 | 40 | 70 | 80 | 90 |
| | | | | | | | |
If the attacks were separated into groups in Step 4, a separate rating is to be obtained for each group of attacks.
Those ratings are not to be combined at this stage but are to be included in the final combining of all ratings.
Step 9: Compare the impairment ratings obtained in Step 3 and Step 8. Take the higher rating.
If the attacks were separated into groups in Step 4, the ratings for the various groups of attacks are to be combined by applying Chapter 18 (Combined Values Chart) before being compared with the rating obtained in Step 3. The combined rating determined under Chapter 18 is to be used only for the purpose of this comparison.
If the combined rating determined under Chapter 18 is higher than the rating obtained in Step 3, then each of the separate ratings for the various groups of attacks is to be included in the final combining of all ratings.
Step 10: Determine the rating for the impairment resulting from the avoidance and preclusion of otherwise normal activities between attacks by using Table 15.5.
Precluded activities refer to ordinary activities. Ratings are to be given on the basis of having to avoid, or of being precluded from undertaking, activities that are common for the veteran’s age group. Ratings are not to be given on the basis of having to avoid only relatively hazardous activities such as rock-climbing or acrobatics.
Table 15.5 is to be applied only if at least one attack of the condition of severity II or greater has occurred within the last two years.
Functional Loss Table 15.5 | 
|
INTERMITTENT IMPAIRMENT: PRECLUDED AND AVOIDED ACTIVITIES |
Impairment Ratings | Criteria |
NIL | Not prevented by fear of an attack from any significant activities. Can lead a normal life between attacks without the need to take long term medication. |
TWO | Must avoid relatively few activities for fear of precipitating an attack. Or Can lead a fairly normal life between attacks but must take long term medication. |
FIVE | Must avoid some activities such as driving a car, using machinery, using public transport, swimming, travelling, being alone except for short periods of time lest an attack occur. |
TEN | Must avoid a wide range of activities such as driving a car, using machinery, using public transport, swimming, travelling, being alone except for short periods of time lest an attack occur with possible severe consequences. |
Only one rating may be had from this table for any given condition. Intermittent conditions may attract a rating from Table 15.5 as well as a rating or ratings from either Table 15.4 or the system specific tables. |
| | |
The rating obtained in Step 10 is not to be compared with the rating obtained in Step 9, nor are ratings to be combined at this stage. Irrespective of the outcome of Step 9 the rating obtained from Table 15.5 is to be included in the final combining of all ratings.
Intermittent Impairment Worksheets
A set of Intermittent Impairment Worksheets (pages 178 to 179) is designed to facilitate the calculation of intermittent impairment rating.
Intermittent Impairment Worksheet (1) is to be used in those cases where all the attacks are grouped into a single type of attack.
Intermittent Impairment Worksheet (2) is to be used in those cases where the attacks are grouped into two or three types.
No worksheet is provided for those cases where more than three types of attacks are involved.
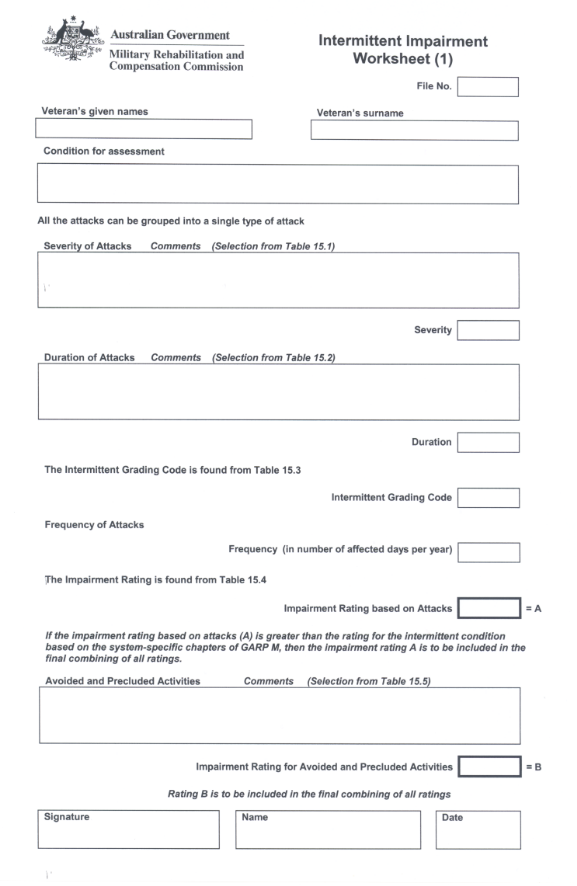
CHAPTER 16
ACTIVITIES OF DAILY LIVING
INTRODUCTION
The Activities of Daily Living (ADLs) are a defined set of activities necessary for normal self-care. The activities are movement in bed, transfers, locomotion, dressing, personal hygiene, and feeding.
These six activities are defined as follows:
- “movement in bed” means sitting in, rising from, and moving around in, bed;
- “transfers” means moving from one seat to another, changing position from sitting to standing, and transferring to and from the toilet and bed;
- “locomotion” means walking on the level, on gentle slopes and down stairs;
- “dressing” means putting on socks, stockings, and shoes, as well as clothing the upper and lower trunk;
- “personal hygiene” means grooming, and washing of face, trunk, extremities and perineum;
- “feeding” means eating and drinking, but not the preparation of food.
“Effects on ADLs” is to be used to assess conditions for which criteria do not exist in the system specific tables of Chapters 1 to 12, or are inadequate, or for which the application of the tables in Chapter 14 (Malignant Conditions) or Chapter 15 (Intermittent Impairment) is inappropriate.
Table 16.3 (Other Impairment) covers such non-specific indicators of disease as pain, lethargy and prognosis.
This chapter is to be applied in the assessment of conditions that result in the veteran being bedfast, chairfast, housebound or nearly housebound. Such conditions include the effects of severe strokes, severe Parkinson’s disease, severe heart failure, severe respiratory disease, severe liver failure, severe kidney failure and some dementias.
ADLs may be used to rate a single condition if its effects are well-differentiated, or may be used to rate all conditions together if their effects are difficult to differentiate.
When ADLs are used to rate a single condition, an impairment rating or ratings from other chapters may be combined with a rating derived from Chapter 16 provided that the ratings relate to different conditions.
When ADLs are used to rate all conditions together, no ratings from other chapters are to be combined with the rating from Chapter 16.
Calculation of the impairment rating for an accepted condition using ADLs
Follow the steps below to calculate the impairment rating due to an accepted condition using the ADLs.
(Each step is elaborated in the following pages.)
STEP 1 | For each of the six ADLs obtain a grading code for that activity. | Page 181 |
STEP 2 | Add up the grading codes for each of the six ADLs. | Page 181 |
STEP 3 | Using the sum obtained in Step 2, determine a functional impairment rating by applying Table 16.2. | Page 182 |
STEP 4 | Determine an Other Impairment rating for the condition by applying Table 16.3. | Page 183 |
STEP 5 | Compare the ratings obtained in Steps 3 and 4. Take the higher rating. | Page 183 |
Step 1: For each of the 6 ADLs, obtain a grading code for that activity using Table 16.1.
From Table 16.1 obtain a separate grading code for:
- movement in bed;
- transfers;
- locomotion;
- dressing;
- personal hygiene; and
- feeding.
Table 16.1 | 
|
ACTIVITIES OF DAILY LIVING GRADING CODES |
Code | Description |
NIL | Independent, and can perform the task as well as peers do, or with minor difficulty only. |
ONE | Can complete the task independently, but with considerably more difficulty than peers have. |
FOUR | Requires some degree of personal assistance in order to perform the task. |
SIX | Requires extensive assistance in order to perform the task. |
EIGHT | Unable to contribute towards performance of the task. Completely dependent. |
No age adjustment permitted for his table
Step 2: Add up the grading codes for each of the 6 ADLs.
Add up the 6 separate grading codes obtained from Table 16.1 for:
- movement in bed;
- transfers;
- locomotion;
- dressing;
- personal hygiene; and
- feeding.
Step 3: Using the sum obtained in Step 2, determine a functional impairment rating by applying Table 16.2.
Use the sum of the grading codes obtained in Step 2 to obtain an impairment rating from Table 16.2.
Functional Loss Table 16.2 | 
|
LOSS OF FUNCTION: ACTIVITIES OF DAILY LIVING |
Impairment Ratings | Sum of Grading Codes |
NIL | 0 |
FIVE | 1–2 |
TEN | 3–4 |
TWENTY | 5–6 |
THIRTY | 7–8 |
FORTY | 9–11 |
FIFTY | 12–14 |
SIXTY | 15–17 |
SEVENTY | 18+ |
| | |
Apply Chapter 19 (Partially Contributing Impairment) to make any necessary adjustment for non-accepted conditions.
Apply Chapter 18 (Apportionment) to make any necessary adjustment for accepted conditions (or groups of conditions) other than the ones that are being assessed by the application of the ADLs tables.
Step 4: Determine an Other Impairment rating for the condition by applying Table 16.3.
Other Impairment Table 16.3 | 
|
ACTIVITIES OF DAILY LIVING: OTHER IMPAIRMENT |
Impairment Ratings | Criteria |
NIL | - No, or negligible, i.e. easily tolerated symptoms.
- Evidence of disease, but minimal interference with daily tasks.
- Feeling of good health most of the time.
- Normal or almost normal life expectancy in spite of disorders.
|
FIVE | - Daily (or almost-daily) symptoms that are irritating and not easily tolerated, but which improve with medication.
- Some daily tasks performed inefficiently because of generalised lethargy.
|
TEN | - Daily (or almost-daily) symptoms that are irritating and not easily tolerated. Treatment is not available, or is of little value, or gives only short remission.
- Noticeable loss of energy, leading to loss of efficiency and avoidance of some tasks previously easily performed.
- Decreased life expectancy. Five year survival less than 75% of normal.
|
| - Intense daily (or almost daily) symptoms which are impossible to ignore, but that prevent few daily tasks. Decreased efficiency in most activities.
- Marked loss of energy leads to avoidance of many daily tasks, most of which can be completed but rapidly cause fatigue.
- Five year survival less than 50% of normal.
|
THIRTY- FIVE | |
| | |
Step 5: Compare the ratings obtained in Steps 3 and 4. Take the higher rating.
The higher of the impairment ratings obtained in Steps 3 and 4 is the final impairment rating for the accepted conditions under assessment, based on ADLs.
CHAPTER 17
DISFIGUREMENT AND SOCIAL IMPAIRMENT
INTRODUCTION
This chapter is to be applied when assessing conditions that cause disfigurement and embarrassment.
Only one rating may be determined by applying this chapter for any condition or combination of conditions. The rating determined by applying this chapter is to be combined with any other ratings for the disfiguring condition or combination of conditions determined under other chapters.
Widespread skin conditions that cause avoidance of ordinary public places should also be assessed under Chapter 11 (Skin Impairment).
“Severe facial disfigurement” and “very severe facial disfigurement” are also mentioned in Chapter 24 (Degree Of Incapacity For Specific Disabilities).
Calculation of the impairment rating for disfigurement.
Follow the steps below to calculate the impairment rating due to disfigurement.
(Each step is elaborated in the following pages.)
STEP 1 | Determine the impairment rating from Table 17.1 for the effect of all accepted conditions that cumulatively lead to disfigurement. | Page 184 |
STEP 2 | If non-accepted conditions have contributed to the disfigurement, apply Chapter 19 (Partially Contributing Impairment) to adjust the rating determined in Step 1. | Page 186 |
Step 1: Determine the impairment rating from Table 17.1 for the effect of all accepted conditions which cumulatively lead to disfigurement.
For the purposes of Table 17.1, the following definitions apply:
“disfiguring condition” means any noticeable condition that causes the sufferer embarrassment in ordinary public places and may include, but is not limited to, the following :
- facial scarring;
- exfoliative skin disorders;
- disorders of gait or posture;
- involuntary facial expressions, or unusual or grotesque involuntary bodily movements;
- disorders of speech;
- vile odours which cannot be overcome by the use of deodorants or the application of normal oral hygiene;
- deficits of the visual field which may cause the veteran to lurch into people through not seeing them;
- painful conditions which may cause the veteran to cry out involuntarily (for example, in response to a sudden pain in a joint); and
- severe pruritic conditions which cause the veteran to scratch even though normal behaviour in a public place would recommend restraint.
“ordinary public places” includes suburban streets, shopping centres, public transport, theatres, clubs and many sporting venues, but does not include places where a great part of the skin is customarily bared such as swimming pools and beaches.
“avoidance” means the veteran feeling obliged as a result of embarrassment to restrict his or her use of public places to hours when few people are about, or to avoid totally use of public places at certain times, for example, when school children are likely to be about.
Functional Loss Table 17.1 | 
|
DISFIGUREMENT | |
Impairment Ratings | Criteria |
NIL | - A visible condition that the veteran does not consider to be disfiguring.
- A noticeable condition that is not significantly disfiguring and which causes negligible or slight embarrassment such as some acne scars on face, or minor limps, or a slight stoop.
|
TWO | - A noticeable condition. For example, severe acne scars, a unilateral squint, an intermittent stutter or stammer.
- A noticeable condition which causes significant embarrassment and may cause avoidance of some normal activities. For example, an ungainly gait, a gross stoop, a persistent stutter or stammer, or an unsightly skin disorder.
|
FIVE | A very noticeable condition which causes marked embarrassment to some people in ordinary social contacts and causes avoidance of some normal activities. For example, a severe skin disorder of the face and/or hands, or a gross and persistent stutter or stammer. |
TEN | - A very noticeable condition which causes marked embarrassment and results in the avoidance of many normal activities. For example, moderate facial disfigurement.
- A severe and marked condition which causes embarrassment and causes much avoidance of many public places and social intercourse. For example, severe facial disfigurement.
|
FIFTEEN | A particularly severe and marked condition which causes extreme embarrassment and results in avoidance of public places and social intercourse to as great a degree as possible. For example, very severe facial disfigurement. |
| Only one rating is to be selected from this table for any condition or group of conditions which contribute to disfigurement. |
| | |
Both the objective and subjective components of a disfiguring condition are to be taken into account when applying Table 17.1. The objective component is the actual physical and/or temporal extent of the disfiguring condition as perceived by others. The subjective component is the veteran’s own emotional and behavioural reactions to the disfigurement.
The two components will generally be aligned with one another. If the veteran has a noticeable condition that is objectively disfiguring but does not embarrass the veteran to the extent to which an average person of the same age, occupational and residential circumstances would be embarrassed, the assessment should be based on the average person’s degree of embarrassment. The veteran’s denial of his or her condition should not be taken into account when applying Table 17.1.
Step 2: If non-accepted conditions have contributed to the disfigurement, apply Chapter 19 (Partially Contributing Impairment) to adjust the rating determined in Step 1.
If non-accepted conditions have contributed to the disfigurement, Table 19.1 in Chapter 19 (Partially Contributing Impairment) is to be applied to adjust the impairment rating for the accepted conditions.
The rating obtained in this step (or in Step 1 if partially contributing impairment is not applicable) is the final rating for disfigurement, and is to be included in the final combining of all impairment ratings.
Part C: Impairment Ratings: Combining, Apportioning, Partially Contributing
CHAPTER 18
COMBINED VALUES CHART
INTRODUCTION
After impairment ratings have been obtained for all accepted conditions they must be combined to a single value known as the combined impairment rating. The combining is not to be done by simple addition but is to be done by applying Table 18.1 (Combined Values Chart). The values in Table 18.1 (Combined Values Chart) are derived from the formula:
Combined value of A and B | = | [A + B (1 - | A | )] rounded to nearest integer |
100 |
where “A” and “B” are the impairment ratings to be combined.
This formula embodies a principle of combining ratings. The principle derives from the concept of whole person impairment (see page X). The following example illustrates the combining principle:
Example
Suppose a veteran has three accepted conditions. If the first assessed condition attracts 60 points the veteran will get a rating of 60. This rating implies that the whole person is 60% impaired. That leaves 40% to be further apportioned among other conditions. If the second condition assessed attracts 30 points, the total impairment rating will not be 60 + 30 = 90, but 60 + 12 = 72. The 12 represents 30% of the 40 that remained of the whole person after the initial 60 was awarded. Now the whole person of the veteran is 72% impaired. If the third condition assessed attracts 10 points, the total impairment rating will be 60 + 12 + 3 = 75. The 3 represents 10% of the 28 that remained of the whole person after 72 was awarded for the first two conditions. Now the whole person of the veteran is 75% impaired.
Combining two or more impairment ratings into a single value.
Follow the steps below to combine two or more impairment ratings into a single value (the combined impairment rating).
STEP 1 | |
STEP 2 | Take the next highest (or equal highest) of the ratings to be combined. Find that rating in the very bottom row of the chart. The column above this number is “The Column” for purposes of Step 3. |
STEP 3 | Find the intersection of The Row and The Column. The number written on the intersection is the combined value of the two ratings. If only two ratings are to be combined, then this figure is the “Combined Impairment Rating”. |
STEP 4 | This step is only to be used if more than two ratings are to be combined. Take the result obtained in Step 3. Find that result in the column on the extreme left hand side of the chart. The row in which this number is written is “The Row” for purposes of Step 6. |
STEP 5 | Take the highest (or equal highest) of the remaining ratings to be combined. Find that rating in the very bottom row of the chart. The column above this number is “The Column” for purposes of Step 6. |
STEP 6 | Find the intersection of The Row and The Column. The number written on the intersection is the combined value of the three ratings. If only three ratings are to be combined, then this figure is the “Combined Impairment Rating”. |
STEP 7 | This step is only to be used if more than three ratings are to be combined. To combine more than three ratings, reapply the instructions in steps 4, 5, and 6 to the remaining ratings. Always take the value obtained by performing Step 6 and combine that with the highest (or equal highest) of the remaining values. Continue until all ratings have been combined into a single value. This figure is the “Combined Impairment Rating”. |
STEP 8 | The individual impairment ratings for the various conditions being assessed are not to be rounded before they are combined using the chart in Table 18.1. If the combined impairment rating is not a multiple of five, it should be rounded to the nearest multiple of five. (For purposes of the preceding sentence, “0” is a multiple of five.) Figures ending on “3” or “4” or “8” or “9” should be rounded up, figures ending on “1” or “2” or “6” or “7” should be rounded down. (This also applies when the only impairment rating a veteran obtains = 2. In that case the combined impairment rating = 0.) |
Example
To combine 35 and 20, read down the extreme left hand side column of the chart in Table 18.1 until you come to the larger value, 35. In the very bottom row of the chart read from left to right until you come to 20. At the intersection of the row on which 35 is written, and the column above 20, is the number 48.
Therefore, 35 combined with 20 is 48. Due to the construction of this chart, the larger impairment value must be identified at the side of the chart.
Applying the formula to this example gives:
35 + 20 × (1 - | 35 | ) = 35 + 20 × (1 - 0.35) = 35 + 20 × 0.65 = 35 + 13 = 48 |
100 |
Table 18.1 | 
|
COMBINED VALUES CHART - Part 1 |
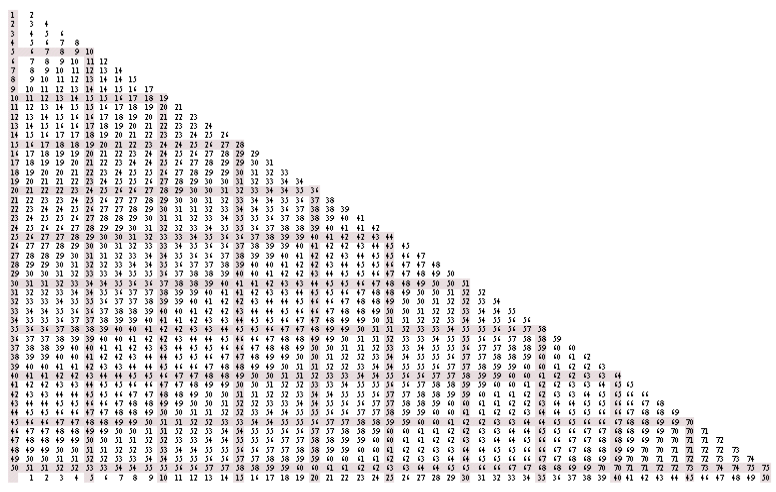
Table 18.1 (continued) | 
|
COMBINED VALUES CHART - Part 2 |
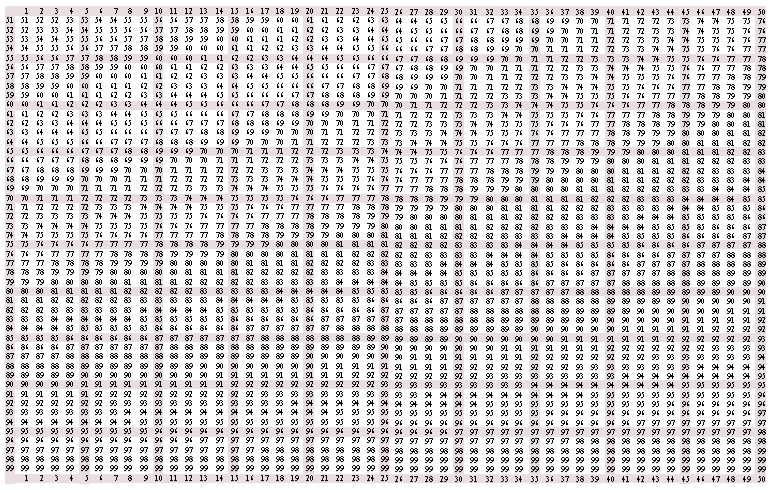
Table 18.1 (continued) | 
|
COMBINED VALUES CHART - Part 3 |
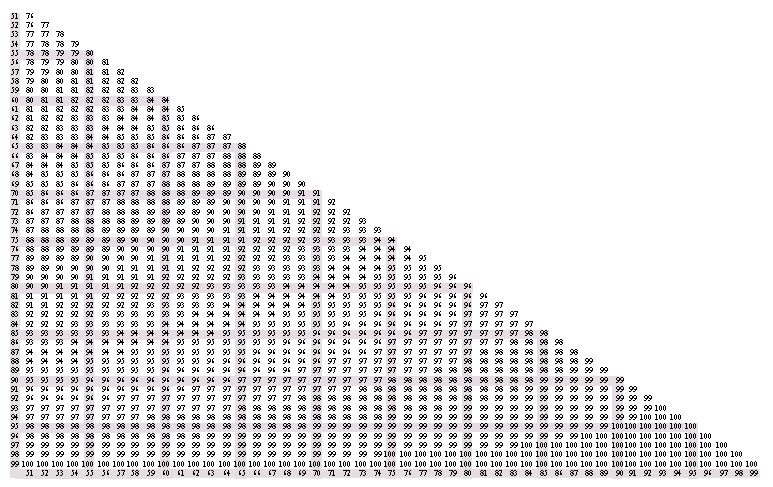
CHAPTER 19
PARTIALLY CONTRIBUTING IMPAIRMENT
INTRODUCTION
Partially contributing impairment is to be applied whenever an impairment is not due solely to the effects of accepted conditions.
How to apply partially contributing impairment
Follow the steps below to apply partially contributing impairment.
(Each step is elaborated in the following pages.)
STEP 1 | Determine whether partially contributing impairment applies. | Page 193 |
STEP 2 | Determine the relative contribution of the accepted and non-accepted conditions. | Page 193 |
STEP 3 | Determine the impairment attributable solely to the accepted condition, by applying Table 19.1. | Page 194 |
Step 1: Determine whether partially contributing impairment applies.
Use relevant medical evidence to determine if any non-accepted conditions contribute to the impairment being assessed.
Step 2: Determine the relative contribution of the accepted and non-accepted conditions.
The judgement of the relative contributions should be based on proper medical advice.
The contribution should be expressed in the form:
‘The accepted condition contributes “not at all”, “about one quarter”, “about one third”, “about half”, etc’.
If more than one accepted condition contributes to the relevant impairment rating, the contribution of the accepted conditions is to be treated as a single entity.
If more than one non-accepted condition contributes to the relevant impairment rating, the contribution of the non-accepted conditions may be treated as a single entity.
Step 3: Determine the impairment rating attributable solely to the accepted condition by applying Table 19.2 or Table 19.1.
Substep 3A | In the columns of Table 19.2 headed “Impairment Rating” find the impairment rating to which partially contributing impairment is being applied. The row extending to the right of the column in which this figure is written is “The Row” for purposes of substep 3C. |
Substep 3B | Take the relative contribution to the impairment by the accepted condition, determined in Step 2. In the top row of Table 19.2 find the description of that contribution. (If the impairment rating used in substep 3A was between 1 and 45 inclusive, the required description of the contribution is to be found in columns 2–8 of Table 19.2. If the impairment rating used in substep 3A was between 46 and 90 inclusive, the required description of the contribution is to be found in columns 10–16 of Table 19.2.) The column in which this description is written is “The Column” for purposes of substep 3C. |
Substep 3C | Find the intersection of The Row and The Column. The number written on the intersection is the impairment rating for the accepted condition. |
Table 19.1 extracts the highlighted information in Table 19.2 and is provided for the convenience of users.
Table 19.1 | 
|
PARTIALLY CONTRIBUTING IMPAIRMENT |
Contribution by accepted condition | 0 | 5 | 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 |
Complete | 0 | 5 | 10 | 15 | 20 | 25 | 30 | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 |
About three quarters | 0 | 4 | 8 | 12 | 16 | 19 | 24 | 28 | 33 | 37 | 42 | 47 | 52 | 57 | 62 | 68 | 73 | 80 | 86 |
About two thirds | 0 | 3 | 7 | 10 | 14 | 18 | 21 | 25 | 29 | 34 | 38 | 43 | 48 | 53 | 58 | 63 | 69 | 76 | 83 |
About half | 0 | 3 | 5 | 8 | 11 | 14 | 17 | 20 | 23 | 26 | 29 | 33 | 37 | 41 | 45 | 50 | 55 | 61 | 68 |
About one third | 0 | 1 | 3 | 5 | 7 | 9 | 11 | 13 | 15 | 17 | 19 | 21 | 24 | 26 | 29 | 32 | 35 | 38 | 42 |
About one quarter | 0 | 1 | 2 | 3 | 5 | 7 | 8 | 10 | 11 | 12 | 14 | 16 | 17 | 19 | 21 | 23 | 25 | 27 | 29 |
Not at all | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| | | | | | | | | | | | | | | | | | | | |
Table 19.2 | 
|
PARTIALLY CONTRIBUTING IMPAIRMENT |
| | | | | | | | | | | | | | | | |
1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | | 46 | 46 | 38 | 35 | 27 | 17 | 13 | 0 |
2 | 2 | 1 | 1 | 1 | 1 | 1 | 0 | | 47 | 47 | 39 | 35 | 27 | 18 | 13 | 0 |
3 | 3 | 2 | 2 | 2 | 1 | 1 | 0 | | 48 | 48 | 40 | 36 | 28 | 18 | 13 | 0 |
4 | 4 | 3 | 3 | 2 | 1 | 1 | 0 | | 49 | 49 | 41 | 37 | 29 | 19 | 14 | 0 |
5 | 5 | 4 | 3 | 3 | 1 | 1 | 0 | | 50 | 50 | 42 | 38 | 29 | 19 | 14 | 0 |
6 | 6 | 4 | 4 | 3 | 2 | 2 | 0 | | 51 | 51 | 43 | 39 | 30 | 20 | 14 | 0 |
7 | 7 | 5 | 5 | 4 | 2 | 2 | 0 | | 52 | 52 | 44 | 40 | 31 | 20 | 15 | 0 |
8 | 8 | 6 | 5 | 4 | 3 | 2 | 0 | | 53 | 53 | 45 | 41 | 32 | 21 | 15 | 0 |
9 | 9 | 7 | 6 | 5 | 3 | 2 | 0 | | 54 | 54 | 46 | 42 | 32 | 21 | 15 | 0 |
10 | 10 | 7 | 7 | 5 | 3 | 3 | 0 | | 55 | 55 | 47 | 43 | 33 | 21 | 16 | 0 |
11 | 11 | 8 | 7 | 6 | 4 | 3 | 0 | | 56 | 56 | 48 | 44 | 34 | 22 | 16 | 0 |
12 | 12 | 9 | 8 | 6 | 4 | 3 | 0 | | 57 | 57 | 49 | 45 | 35 | 22 | 16 | 0 |
13 | 13 | 10 | 9 | 7 | 4 | 3 | 0 | | 58 | 58 | 49 | 46 | 35 | 23 | 17 | 0 |
14 | 14 | 10 | 9 | 7 | 5 | 4 | 0 | | 59 | 59 | 51 | 47 | 36 | 23 | 17 | 0 |
15 | 15 | 11 | 10 | 8 | 5 | 4 | 0 | | 60 | 60 | 52 | 48 | 37 | 24 | 17 | 0 |
16 | 16 | 12 | 11 | 9 | 6 | 4 | 0 | | 61 | 61 | 53 | 49 | 38 | 24 | 18 | 0 |
17 | 17 | 13 | 12 | 9 | 6 | 5 | 0 | | 62 | 62 | 54 | 49 | 38 | 25 | 18 | 0 |
18 | 18 | 14 | 13 | 10 | 6 | 5 | 0 | | 63 | 63 | 55 | 50 | 39 | 25 | 18 | 0 |
19 | 19 | 15 | 13 | 10 | 7 | 5 | 0 | | 64 | 64 | 56 | 52 | 40 | 26 | 19 | 0 |
20 | 20 | 16 | 14 | 11 | 7 | 5 | 0 | | 65 | 65 | 57 | 53 | 41 | 26 | 19 | 0 |
21 | 21 | 16 | 15 | 11 | 7 | 6 | 0 | | 66 | 66 | 58 | 54 | 42 | 27 | 19 | 0 |
22 | 22 | 17 | 15 | 12 | 8 | 6 | 0 | | 67 | 67 | 59 | 55 | 43 | 27 | 20 | 0 |
23 | 23 | 18 | 16 | 12 | 8 | 6 | 0 | | 68 | 68 | 60 | 56 | 43 | 28 | 20 | 0 |
24 | 24 | 19 | 17 | 13 | 9 | 6 | 0 | | 69 | 69 | 61 | 57 | 44 | 29 | 20 | 0 |
25 | 25 | 19 | 18 | 14 | 9 | 7 | 0 | | 70 | 70 | 62 | 58 | 45 | 29 | 21 | 0 |
26 | 26 | 20 | 19 | 14 | 9 | 7 | 0 | | 71 | 71 | 63 | 59 | 46 | 30 | 21 | 0 |
27 | 27 | 21 | 19 | 15 | 10 | 7 | 0 | | 72 | 72 | 64 | 60 | 47 | 30 | 21 | 0 |
28 | 28 | 22 | 20 | 15 | 10 | 8 | 0 | | 73 | 73 | 66 | 61 | 48 | 30 | 22 | 0 |
29 | 29 | 23 | 21 | 16 | 10 | 8 | 0 | | 74 | 74 | 67 | 62 | 49 | 31 | 22 | 0 |
30 | 30 | 24 | 21 | 17 | 11 | 8 | 0 | | 75 | 75 | 68 | 63 | 50 | 32 | 23 | 0 |
31 | 31 | 25 | 22 | 17 | 11 | 8 | 0 | | 76 | 76 | 69 | 64 | 51 | 32 | 23 | 0 |
32 | 32 | 25 | 23 | 18 | 12 | 9 | 0 | | 77 | 77 | 70 | 66 | 52 | 33 | 23 | 0 |
33 | 33 | 26 | 24 | 18 | 12 | 9 | 0 | | 78 | 78 | 71 | 67 | 53 | 34 | 24 | 0 |
34 | 34 | 27 | 25 | 19 | 12 | 9 | 0 | | 79 | 79 | 72 | 68 | 54 | 34 | 24 | 0 |
35 | 35 | 28 | 25 | 20 | 13 | 10 | 0 | | 80 | 80 | 73 | 69 | 55 | 35 | 25 | 0 |
36 | 36 | 29 | 26 | 20 | 13 | 10 | 0 | | 81 | 81 | 75 | 70 | 56 | 35 | 25 | 0 |
37 | 37 | 30 | 27 | 21 | 14 | 10 | 0 | | 82 | 82 | 76 | 72 | 57 | 36 | 25 | 0 |
38 | 38 | 31 | 28 | 21 | 14 | 10 | 0 | | 83 | 83 | 77 | 73 | 59 | 37 | 26 | 0 |
39 | 39 | 32 | 29 | 22 | 14 | 11 | 0 | | 84 | 84 | 78 | 74 | 60 | 37 | 26 | 0 |
40 | 40 | 33 | 29 | 23 | 15 | 11 | 0 | | 85 | 85 | 80 | 76 | 61 | 38 | 27 | 0 |
41 | 41 | 34 | 30 | 23 | 15 | 11 | 0 | | 86 | 86 | 81 | 77 | 62 | 39 | 27 | 0 |
42 | 42 | 34 | 31 | 24 | 16 | 12 | 0 | | 87 | 87 | 82 | 78 | 64 | 39 | 27 | 0 |
43 | 43 | 35 | 32 | 25 | 16 | 12 | 0 | | 88 | 88 | 84 | 80 | 65 | 40 | 28 | 0 |
44 | 44 | 36 | 33 | 25 | 17 | 12 | 0 | | 89 | 89 | 85 | 80 | 65 | 40 | 28 | 0 |
45 | 45 | 37 | 34 | 26 | 17 | 12 | 0 | | 90 | 90 | 86 | 83 | 68 | 42 | 29 | 0 |
| | | | | | | | | | | | | | | | | |
CHAPTER 20
APPORTIONMENT
INTRODUCTION
Throughout this Guide, if a condition can be rated using both a functional loss table and an Other Impairment table, only the higher of the two ratings is to be given to the veteran. This is usually quite a simple thing to do.
However, in some cases, it might not be so straightforward. For example, a veteran has two accepted cardiorespiratory conditions. One is ischaemic heart disease and the other is chronic bronchitis. From METs and spirometry it is found that the veteran’s functional impairment rating is 20 points. It is also found that the veteran’s ischaemic heart disease corresponds to a rating of 10 points from Table 1.6 and the veteran’s chronic bronchitis corresponds to a rating of 5 points from Table 1.10.
Without apportionment the only applicable cardiorespiratory rating would be 20 points and the 10 and 5 point ratings would have to be disregarded because they are both less than 20. This approach would sometimes disadvantage the veteran.
A method of establishing the separate contribution of ischaemic heart disease and the chronic bronchitis to the functional impairment would enable a separation of their contributions thus allowing the comparison of functional and Other Impairments on a condition by condition basis. Such a method is called “apportionment”. Apportionment provides a method for determining whether a rating greater than 20 should be given to the veteran in the example.
Tables 20.1 to 20.13 have been constructed by finding a set of impairment ratings which have the same value as the contribution to the rating to be apportioned, and which, when combined using the Combined Values Chart in Chapter 18, are equal to the original impairment rating.
If the apportionment has to be done in ratios that are not included in Tables 20.1 to 20.13, then the apportionment may be performed by applying Table 18.1 (Combined Values Chart) in reverse. Should more than one solution be possible, that which is the best fit is to be used.
The ratings that result from the application of apportionment can never be less than those which the same conditions would have attracted had apportionment not been applied.
HOW TO USE APPORTIONMENT
INSTRUCTIONS
Follow the steps below in applying apportionment.
STEP 1 | Determine if apportionment is to be used. Apportionment is to be used when it is necessary, for a given accepted condition, to compare an impairment rating derived from one table with an impairment rating derived from another table, and when two or more accepted conditions contribute to the impairment ratings from either table. |
STEP 2 | Find the relative contribution of each contributing condition. The relative contribution of each accepted condition to the impairment rating that is to be apportioned should be expressed as a simple ratio. (The ratio should always be expressed in terms of small integers, e.g. 1:2, 1:3, 1:1:2, etc.) The judgement of the ratio should be based on appropriate medical advice. |
STEP 3 | Apportion the single impairment rating into parts. Once the ratio is known the single rating is to be apportioned to all the contributing conditions. In common cases (2 or 3 contributing conditions) the apportioned ratings are to be read off Tables 20.1 to 20.13. In unusual cases that are not covered in these tables, the method described on page 197 is to be applied. |
STEP 4 | For each condition, compare ratings from two relevant tables. For each condition, the higher of the two relevant ratings is to be selected. |
STEP 5 | Do not combine individual ratings until the end. Individual ratings obtained from applying the apportionment process are not to be combined until the end of the overall assessment process, when ratings for all of the veteran’s assessable conditions are combined to obtain a single value representing the combined impairment rating for accepted conditions. |
Example
The apportionment process can be illustrated by using the example mentioned in the introduction.
STEP 1 | Determine if apportionment is to be used. When ischaemic heart disease and chronic bronchitis are both accepted conditions, apportionment has to be used because each of these conditions can be rated from separate Other Impairment tables in Chapter 1. |
STEP 2 | Find the relative contribution of each contributing condition. Suppose that, on medical advice, it is found that the contributions by chronic bronchitis and ischaemic heart disease are in the ratio of 2:1. |
STEP 3 | Break up the single impairment rating into parts. As the ratio is 2:1, Table 20.1 or Table 20.4 is to be used. From either of these it is found that 20 points apportioned in the ratio of 2:1 gives 14 and 7 as the two contributory impairment ratings. Thus the functional impairment rating for chronic bronchitis is 14 points and for ischaemic heart disease it is 7 points. |
STEP 4 | Compare ratings from two tables for each condition. Compare the ratings for ischaemic heart disease (7 versus 10 from Table 1.6) and for chronic bronchitis (14 versus 5 from Table 1.10). Taking the higher rating in each case, the assessment will be: ischaemic heart disease 10 points, chronic bronchitis 14 points. |
STEP 5 | Do not combine individual ratings until the end. If this veteran had no other accepted conditions, the final combined impairment rating would be 25 points (10 & 14 = 23, rounded to 25) instead of 20 points without apportionment. |
The calculations in the above example can be conveniently set out in a worksheet format, as illustrated below.
Rating to be apportioned: 20
| A | B | C | D |
Accepted Conditions | Relative Contribution | Functional Rating | Other Impairment | Rating for Condition |
Ischaemic Heart Disease | 1 | 7 | 10 | 10 |
Chronic Bronchitis | 2 | 14 | 5 | 14 |
For purposes of the above worksheet
“Accepted Conditions” | means the accepted conditions that con-tribute to a single impairment rating to be apportioned. |
“Relative Contribution” | means the ratio of the relative contributions which the conditions make to the total impairment (in the above example, the ratio is 1:2, written as “1” in the top row of column A, and “2” in the bottom row of column A). |
“Functional Rating” | means the ratings for the conditions obtained after apportionment. |
“Other Impairment” | means the applicable rating for the conditions obtained from an Other Impairment table. |
“Rating for Condition” | means the higher of the ratings in columns B and C of the same row. This is the final impairment rating for the condition named in that row. |
For convenience, Tables 20.1 and 20.2 give the apportionment for impairment ratings that are multiples of 5. Table 20.3 to 20.13 give the apportionment for all relevant integral values of impairment ratings for certain given ratios.
Table 20.1 can be applied to find the two relevant values when any impairment rating has to be apportioned between two conditions in any of the given ratios.
The top row contains the ratios into which the impairment rating needs to be apportioned. The left hand column contains the impairment ratings to be apportioned.
From Table 20.1 it will be seen that:
- if a rating of 55 points is to be divided in the ratio of 3:1, one condition gets 47 points and the other gets 16; and
- if a rating of 35 points is to be divided in the ratio of 3:2, one condition gets 23 points and the other gets 16.
Table 20.1 | 
|
APPORTIONMENT |
Ratios |
| | 1:1 | 2:1 | 3:1 | 4:1 | 5:1 | 3:2 | |
| 5 | 2 & 3 | 4 & 2 | 3 & 1 | 4 & 1 | 5 & 1 | 3 & 2 | |
10 | 5 & 5 | 7 & 3 | 8 & 3 | 8 & 2 | 9 & 2 | 6 & 4 | |
15 | 8 & 8 | 10 & 5 | 11 & 4 | 12 & 3 | 13 & 2 | 10 & 6 | |
20 | 10 & 11 | 14 & 7 | 16 & 5 | 17 & 4 | 18 & 4 | 13 & 8 | |
25 | 13 & 14 | 18 & 9 | 19 & 7 | 21 & 5 | 21 & 5 | 16 & 11 | |
30 | 16 & 17 | 21 & 11 | 24 & 8 | 25 & 6 | 26 & 5 | 19 & 13 | |
35 | 19 & 20 | 25 & 13 | 29 & 9 | 30 & 7 | 31 & 6 | 23 & 16 | |
40 | 23 & 22 | 29 & 15 | 33 & 11 | 34 & 9 | 35 & 7 | 27 & 18 | |
45 | 26 & 26 | 34 & 17 | 37 & 12 | 39 & 10 | 40 & 8 | 31 & 21 | |
50 | 29 & 29 | 38 & 19 | 42 & 14 | 44 & 11 | 45 & 9 | 33 & 25 | |
55 | 33 & 33 | 43 & 21 | 47 & 16 | 49 & 12 | 50 & 10 | 39 & 26 | |
60 | 37 & 37 | 48 & 24 | 52 & 17 | 54 & 13 | 55 & 11 | 44 & 29 | |
65 | 41 & 41 | 53 & 26 | 57 & 19 | 59 & 15 | 60 & 12 | 48 & 32 | |
70 | 45 & 45 | 58 & 29 | 62 & 21 | 64 & 16 | 65 & 13 | 53 & 36 | |
75 | 50 & 50 | 63 & 32 | 68 & 23 | 70 & 18 | 71 & 14 | 59 & 39 | |
80 | 55 & 55 | 69 & 35 | 73 & 25 | 75 & 19 | 76 & 15 | 65 & 43 | |
85 | 61 & 61 | 76 & 38 | 80 & 27 | 81 & 20 | 82 & 16 | 72 & 48 | |
90 | 68 & 68 | 83 & 42 | 86 & 29 | 87 & 22 | 88 & 18 | 79 & 53 | |
| This table shows the relevant values when any impairment rating has to be apportioned between two conditions | |
| | | | | | | | | |
Table 20.2 | 
|
APPORTIONMENT |
Ratios |
| | 1:1:1 | 2:1:1 | 2:2:1 | 3:2:1 |
| 5 | 2 & 2 & 1 | 2 & 2 & 1 | 2 & 2 & 1 | 2 & 2 & 1 |
10 | 4 & 3 & 3 | 5 & 3 & 2 | 4 & 4 & 2 | 5 & 3 & 2 |
15 | 5 & 5 & 5 | 7 & 4 & 4 | 6 & 6 & 3 | 7 & 5 & 3 |
20 | 7 & 7 & 7 | 11 & 6 & 5 | 9 & 9 & 4 | 11 & 7 & 4 |
25 | 10 & 9 & 9 | 13 & 7 & 7 | 11 & 11 & 5 | 13 & 9 & 5 |
30 | 11 & 11 & 11 | 17 & 8 & 8 | 14 & 13 & 7 | 17 & 11 & 6 |
35 | 14 & 13 & 13 | 20 & 10 & 10 | 16 & 16 & 8 | 20 & 13 & 7 |
40 | 16 & 16 & 16 | 23 & 12 & 12 | 19 & 18 & 9 | 23 & 16 & 8 |
45 | 18 & 18 & 18 | 27 & 14 & 13 | 22 & 21 & 11 | 27 & 18 & 9 |
50 | 21 & 21 & 20 | 30 & 15 & 15 | 25 & 24 & 12 | 30 & 20 & 10 |
55 | 23 & 23 & 23 | 35 & 17 & 17 | 28 & 28 & 14 | 34 & 22 & 11 |
60 | 27 & 26 & 26 | 38 & 19 & 19 | 31 & 31 & 16 | 38 & 26 & 13 |
65 | 29 & 29 & 29 | 43 & 22 & 21 | 35 & 35 & 17 | 43 & 28 & 14 |
70 | 33 & 33 & 33 | 48 & 24 & 24 | 40 & 39 & 20 | 47 & 32 & 16 |
75 | 37 & 37 & 37 | 54 & 27 & 27 | 44 & 43 & 22 | 53 & 36 & 18 |
80 | 42 & 42 & 42 | 60 & 30 & 30 | 49 & 49 & 24 | 59 & 40 & 20 |
85 | 47 & 47 & 47 | 66 & 33 & 33 | 54 & 54 & 27 | 60 & 44 & 22 |
90 | 53 & 53 & 53 | 74 & 37 & 37 | 62 & 62 & 31 | 79 & 52 & 26 |
| This table shows the relevant values when any impairment rating has to be apportioned between three conditions. |
| | | | | | |
In the Apportionment tables, those solutions in bold are exact apportionments into the specified ratios. All the other solutions are the best approximations to the specified ratios.
From Table 20.2 it will be seen that:
- if a rating of 55 points is to be divided in the ratio of 2:2:1, one condition gets 28 points, another gets 28, and the third gets 14 points; and
- if a rating of 35 points is to be divided in the ratio of 3:2:1, one condition gets 20 points, another gets 13, and the third gets 7 points.
Table 20.3 | 
|
APPORTIONMENT | | |
Impairment Rating | Apportioned in Ratio 1:1 | Impairment Rating | Apportioned in Ratio 1:1 | |
1 | 1 & 0 | 46 | 27 & 26 | |
2 | 1 & 1 | 47 | 27 & 27 | |
3 | 2 & 1 | 48 | 28 & 28 | |
4 | 2 & 2 | 49 | 29 & 28 | |
5 | 3 & 2 | 50 | 29 & 29 | |
6 | 3 & 3 | 51 | 30 & 30 | |
7 | 4 & 3 | 52 | 31 & 31 | |
8 | 4 & 4 | 53 | 32 & 31 | |
9 | 5 & 4 | 54 | 32 & 32 | |
10 | 5 & 5 | 55 | 33 & 33 | |
11 | 6 & 5 | 56 | 34 & 34 | |
12 | 6 & 6 | 57 | 35 & 34 | |
13 | 7 & 6 | 58 | 35 & 35 | |
14 | 7 & 7 | 59 | 36 & 36 | |
15 | 8 & 8 | 60 | 37 & 37 | |
16 | 9 & 8 | 61 | 38 & 37 | |
17 | 9 & 9 | 62 | 38 & 38 | |
18 | 10 & 9 | 63 | 39 & 39 | |
19 | 10 & 10 | 64 | 40 & 40 | |
20 | 11 & 10 | 65 | 41 & 41 | |
21 | 11 & 11 | 66 | 42 & 42 | |
22 | 12 & 11 | 67 | 43 & 42 | |
23 | 12 & 12 | 68 | 43 & 43 | |
24 | 13 & 13 | 69 | 44 & 44 | |
25 | 14 & 13 | 70 | 45 & 45 | |
26 | 14 & 14 | 71 | 46 & 46 | |
27 | 15 & 14 | 72 | 47 & 47 | |
28 | 15 & 15 | 73 | 48 & 48 | |
29 | 16 & 16 | 74 | 49 & 49 | |
30 | 17 & 16 | 75 | 50 & 50 | |
31 | 17 & 17 | 76 | 51 & 51 | |
32 | 18 & 17 | 77 | 52 & 52 | |
33 | 18 & 18 | 78 | 53 & 53 | |
34 | 19 & 19 | 79 | 54 & 54 | |
35 | 20 & 19 | 80 | 55 & 55 | |
36 | 20 & 20 | 81 | 56 & 56 | |
37 | 21 & 20 | 82 | 57 & 57 | |
38 | 21 & 21 | 83 | 59 & 59 | |
39 | 22 & 22 | 84 | 60 & 60 | |
40 | 23 & 22 | 85 | 61 & 61 | |
41 | 23 & 23 | 86 | 62 & 62 | |
42 | 24 & 24 | 87 | 64 & 64 | |
43 | 25 & 24 | 88 | 65 & 65 | |
44 | 25 & 25 | 89 | 67 & 67 | |
45 | 26 & 26 | 90 | 68 & 68 | |
| | | | | | |
| Table 20.4 | 
|
| APPORTIONMENT |
Impairment Rating | Apportioned in Ratio 2:1 | Impairment Rating | Apportioned in Ratio 2:1 | |
1 | 1 & 0 | 46 | 35 & 17 | |
2 | 1 & 1 | 47 | 35 & 18 | |
3 | 2 & 1 | 48 | 36 & 18 | |
4 | 3 & 1 | 49 | 37 & 19 | |
5 | 3 & 2 | 50 | 38 & 19 | |
6 | 4 & 2 | 51 | 39 & 20 | |
7 | 5 & 2 | 52 | 40 & 20 | |
8 | 5 & 3 | 53 | 41 & 21 | |
9 | 6 & 3 | 54 | 42 & 21 | |
10 | 7 & 3 | 55 | 43 & 21 | |
11 | 7 & 4 | 56 | 44 & 22 | |
12 | 8 & 4 | 57 | 45 & 22 | |
13 | 9 & 4 | 58 | 46 & 23 | |
14 | 9 & 5 | 59 | 47 & 23 | |
15 | 10 & 5 | 60 | 48 & 24 | |
16 | 11 & 6 | 61 | 49 & 24 | |
17 | 12 & 6 | 62 | 49 & 25 | |
18 | 13 & 6 | 63 | 50 & 25 | |
19 | 13 & 7 | 64 | 52 & 26 | |
20 | 14 & 7 | 65 | 53 & 26 | |
21 | 15 & 7 | 66 | 54 & 27 | |
22 | 15 & 8 | 67 | 55 & 27 | |
23 | 16 & 8 | 68 | 56 & 28 | |
24 | 17 & 9 | 69 | 57 & 29 | |
25 | 18 & 9 | 70 | 58 & 29 | |
26 | 19 & 9 | 71 | 59 & 30 | |
27 | 19 & 10 | 72 | 60 & 30 | |
28 | 20 & 10 | 73 | 61 & 31 | |
29 | 21 & 10 | 74 | 62 & 31 | |
30 | 21 & 11 | 75 | 63 & 32 | |
31 | 22 & 11 | 76 | 64 & 32 | |
32 | 23 & 12 | 77 | 66 & 33 | |
33 | 24 & 12 | 78 | 67 & 34 | |
34 | 25 & 12 | 79 | 68 & 34 | |
35 | 25 & 13 | 80 | 69 & 35 | |
36 | 26 & 13 | 81 | 70 & 35 | |
37 | 27 & 14 | 82 | 72 & 36 | |
38 | 28 & 14 | 83 | 73 & 37 | |
39 | 29 & 14 | 84 | 74 & 37 | |
40 | 29 & 15 | 85 | 76 & 38 | |
41 | 30 & 15 | 86 | 77 & 39 | |
42 | 31 & 16 | 87 | 78 & 39 | |
43 | 32 & 16 | 88 | 80 & 40 | |
44 | 33 & 17 | 89 | 82 & 41 | |
45 | 34 & 17 | 90 | 83 & 42 | |
| | | | | | |
Table 20.5 | 
| | |
APPORTIONMENT |
Impairment Rating | Apportioned in Ratio 3:1 | Impairment Rating | Apportioned in Ratio 3:1 | |
1 | 1 & 0 | 46 | 38 & 13 | |
2 | 2 & 0 | 47 | 39 & 13 | |
3 | 2 & 1 | 48 | 40 & 13 | |
4 | 3 & 1 | 49 | 41 & 14 | |
5 | 4 & 1 | 50 | 42 & 14 | |
6 | 4 & 2 | 51 | 43 & 14 | |
7 | 5 & 2 | 52 | 44 & 15 | |
8 | 6 & 2 | 53 | 45 & 15 | |
9 | 7 & 2 | 54 | 46 & 15 | |
10 | 7 & 3 | 55 | 47 & 16 | |
11 | 8 & 3 | 56 | 48 & 16 | |
12 | 9 & 3 | 57 | 49 & 16 | |
13 | 10 & 3 | 58 | 49 & 17 | |
14 | 10 & 4 | 59 | 51 & 17 | |
15 | 11 & 4 | 60 | 52 & 17 | |
16 | 12 & 4 | 61 | 53 & 18 | |
17 | 13 & 5 | 62 | 54 & 18 | |
18 | 14 & 5 | 63 | 55 & 18 | |
19 | 15 & 5 | 64 | 56 & 19 | |
20 | 16 & 5 | 65 | 57 & 19 | |
21 | 16 & 6 | 66 | 58 & 19 | |
22 | 17 & 6 | 67 | 59 & 20 | |
23 | 18 & 6 | 68 | 60 & 20 | |
24 | 19 & 6 | 69 | 61 & 20 | |
25 | 19 & 7 | 70 | 62 & 21 | |
26 | 20 & 7 | 71 | 63 & 21 | |
27 | 21 & 7 | 72 | 64 & 21 | |
28 | 22 & 8 | 73 | 66 & 22 | |
29 | 23 & 8 | 74 | 67 & 22 | |
30 | 24 & 8 | 75 | 68 & 23 | |
31 | 25 & 8 | 76 | 69 & 23 | |
32 | 25 & 9 | 77 | 70 & 23 | |
33 | 26 & 9 | 78 | 71 & 24 | |
34 | 27 & 9 | 79 | 72 & 24 | |
35 | 28 & 10 | 80 | 73 & 25 | |
36 | 29 & 10 | 81 | 75 & 25 | |
37 | 30 & 10 | 82 | 76 & 25 | |
38 | 31 & 10 | 83 | 77 & 26 | |
39 | 32 & 11 | 84 | 78 & 26 | |
40 | 33 & 11 | 85 | 80 & 27 | |
41 | 34 & 11 | 86 | 81 & 27 | |
42 | 34 & 12 | 87 | 82 & 27 | |
43 | 35 & 12 | 88 | 84 & 28 | |
44 | 36 & 12 | 89 | 85 & 28 | |
45 | 37 & 12 | 90 | 86 & 29 | |
| | | | | | |
Table 20.6 | 
|
APPORTIONMENT |
Impairment Rating | Apportioned in Ratio 4:1 | Impairment Rating | Apportioned in Ratio 4:1 |
1 | 1 & 0 | 46 | 40 & 10 |
2 | 2 & 0 | 47 | 41 & 10 |
3 | 2 & 1 | 48 | 42 & 11 |
4 | 3 & 1 | 49 | 43 & 11 |
5 | 4 & 1 | 50 | 44 & 11 |
6 | 5 & 1 | 51 | 45 & 11 |
7 | 6 & 1 | 52 | 46 & 12 |
8 | 6 & 2 | 53 | 47 & 12 |
9 | 7 & 2 | 54 | 48 & 12 |
10 | 8 & 2 | 55 | 49 & 12 |
11 | 9 & 2 | 56 | 50 & 12 |
12 | 10 & 2 | 57 | 51 & 13 |
13 | 10 & 3 | 58 | 52 & 13 |
14 | 11 & 3 | 59 | 53 & 13 |
15 | 12 & 3 | 60 | 54 & 14 |
16 | 13 & 3 | 61 | 55 & 14 |
17 | 14 & 4 | 62 | 56 & 14 |
18 | 15 & 4 | 63 | 57 & 14 |
19 | 16 & 4 | 64 | 58 & 15 |
20 | 17 & 4 | 65 | 59 & 15 |
21 | 18 & 4 | 66 | 60 & 15 |
22 | 18 & 5 | 67 | 61 & 15 |
23 | 19 & 5 | 68 | 62 & 16 |
24 | 20 & 5 | 69 | 63 & 16 |
25 | 21 & 5 | 70 | 64 & 16 |
26 | 22 & 5 | 71 | 65 & 16 |
27 | 22 & 6 | 72 | 66 & 17 |
28 | 23 & 6 | 73 | 68 & 17 |
29 | 24 & 6 | 74 | 69 & 17 |
30 | 25 & 6 | 75 | 70 & 18 |
31 | 26 & 7 | 76 | 71 & 18 |
32 | 27 & 7 | 77 | 72 & 18 |
33 | 28 & 7 | 78 | 73 & 18 |
34 | 29 & 7 | 79 | 74 & 19 |
35 | 30 & 7 | 80 | 75 & 19 |
36 | 30 & 8 | 81 | 76 & 19 |
37 | 32 & 8 | 82 | 78 & 20 |
38 | 33 & 8 | 83 | 79 & 20 |
39 | 34 & 8 | 84 | 80 & 20 |
40 | 34 & 9 | 85 | 81 & 20 |
41 | 35 & 9 | 86 | 82 & 21 |
42 | 36 & 9 | 87 | 84 & 21 |
43 | 37 & 9 | 88 | 85 & 21 |
44 | 38 & 10 | 89 | 86 & 22 |
45 | 39 & 10 | 90 | 87 & 22 |
| | | | |
Table 20.7 | 
|
APPORTIONMENT |
Impairment Rating | Apportioned in Ratio 5:1 | Impairment Rating | Apportioned in Ratio 5:1 | |
1 | 1 & 0 | 46 | 41 & 8 | |
2 | 1 & 1 | 47 | 42 & 8 | |
3 | 2 & 1 | 48 | 43 & 9 | |
4 | 3 & 1 | 49 | 44 & 9 | |
5 | 4 & 1 | 50 | 45 & 9 | |
6 | 5 & 1 | 51 | 46 & 9 | |
7 | 6 & 1 | 52 | 47 & 9 | |
8 | 7 & 1 | 53 | 48 & 10 | |
9 | 7 & 2 | 54 | 49 & 10 | |
10 | 8 & 2 | 55 | 50 & 10 | |
11 | 9 & 2 | 56 | 51 & 10 | |
12 | 10 & 2 | 57 | 52 & 10 | |
13 | 11 & 2 | 58 | 53 & 11 | |
14 | 12 & 2 | 59 | 54 & 11 | |
15 | 12 & 3 | 60 | 55 & 11 | |
16 | 13 & 3 | 61 | 56 & 11 | |
17 | 14 & 3 | 62 | 57 & 11 | |
18 | 15 & 3 | 63 | 58 & 12 | |
19 | 16 & 3 | 64 | 59 & 12 | |
20 | 17 & 4 | 65 | 60 & 12 | |
21 | 18 & 4 | 66 | 61 & 12 | |
22 | 19 & 4 | 67 | 62 & 12 | |
23 | 20 & 4 | 68 | 63 & 13 | |
24 | 21 & 4 | 69 | 64 & 13 | |
25 | 22 & 4 | 70 | 65 & 13 | |
26 | 22 & 5 | 71 | 67 & 13 | |
27 | 23 & 5 | 72 | 68 & 14 | |
28 | 24 & 5 | 73 | 69 & 14 | |
29 | 25 & 5 | 74 | 70 & 14 | |
30 | 26 & 5 | 75 | 71 & 14 | |
31 | 27 & 5 | 76 | 72 & 14 | |
32 | 28 & 6 | 77 | 73 & 15 | |
33 | 29 & 6 | 78 | 74 & 15 | |
34 | 30 & 6 | 79 | 75 & 15 | |
35 | 31 & 6 | 80 | 76 & 15 | |
36 | 32 & 6 | 81 | 77 & 16 | |
37 | 32 & 7 | 82 | 79 & 16 | |
38 | 33 & 7 | 83 | 80 & 16 | |
39 | 34 & 7 | 84 | 81 & 16 | |
40 | 35 & 7 | 85 | 82 & 16 | |
41 | 37 & 7 | 86 | 83 & 17 | |
42 | 37 & 8 | 87 | 84 & 17 | |
43 | 38 & 8 | 88 | 85 & 17 | |
44 | 39 & 8 | 89 | 87 & 17 | |
45 | 40 & 8 | 90 | 88 & 18 | |
| | | | | | |
Table 20.8 | 
| |
APPORTIONMENT | |
Impairment Rating | Apportioned in Ratio 3:2 | Impairment Rating | Apportioned in Ratio 3:2 |
1 | 1 & 0 | 46 | 32 & 21 |
2 | 1 & 1 | 47 | 32 & 22 |
3 | 2 & 1 | 48 | 33 & 22 |
4 | 2 & 2 | 49 | 34 & 23 |
5 | 3 & 2 | 50 | 35 & 23 |
6 | 3 & 3 | 51 | 36 & 24 |
7 | 4 & 3 | 52 | 37 & 24 |
8 | 5 & 3 | 53 | 37 & 25 |
9 | 5 & 4 | 54 | 38 & 25 |
10 | 6 & 4 | 55 | 39 & 26 |
11 | 7 & 4 | 56 | 40 & 27 |
12 | 7 & 5 | 57 | 41 & 27 |
13 | 8 & 5 | 58 | 42 & 28 |
14 | 9 & 6 | 59 | 43 & 28 |
15 | 10 & 6 | 60 | 43 & 29 |
16 | 10 & 7 | 61 | 44 & 30 |
17 | 11 & 7 | 62 | 45 & 30 |
18 | 11 & 8 | 63 | 46 & 31 |
19 | 12 & 8 | 64 | 47 & 32 |
20 | 13 & 8 | 65 | 48 & 32 |
21 | 13 & 9 | 66 | 49 & 33 |
22 | 14 & 9 | 67 | 50 & 33 |
23 | 14 & 10 | 68 | 51 & 34 |
24 | 15 & 10 | 69 | 53 & 35 |
25 | 16 & 11 | 70 | 53 & 36 |
26 | 17 & 11 | 71 | 54 & 36 |
27 | 17 & 12 | 72 | 56 & 37 |
28 | 18 & 12 | 73 | 57 & 38 |
29 | 19 & 12 | 74 | 58 & 39 |
30 | 20 & 13 | 75 | 59 & 39 |
31 | 20 & 14 | 76 | 60 & 40 |
32 | 21 & 14 | 77 | 61 & 41 |
33 | 22 & 14 | 78 | 62 & 41 |
34 | 22 & 15 | 79 | 63 & 42 |
35 | 23 & 15 | 80 | 65 & 43 |
36 | 24 & 16 | 81 | 66 & 44 |
37 | 25 & 16 | 82 | 68 & 45 |
38 | 25 & 17 | 83 | 69 & 46 |
39 | 26 & 17 | 84 | 70 & 47 |
40 | 27 & 18 | 85 | 72 & 48 |
41 | 28 & 18 | 86 | 73 & 49 |
42 | 28 & 19 | 87 | 74 & 49 |
43 | 29 & 20 | 88 | 75 & 50 |
44 | 30 & 20 | 89 | 75 & 52 |
45 | 31 & 21 | 90 | 79 & 53 |
| | | | | |
Table 20.9 | 
|
APPORTIONMENT |
Impairment Rating | Apportioned in Ratio 1:1:1 | Impairment Rating | Apportioned in Ratio 1:1:1 |
1 | 1 & 0 & 0 | 46 | 19 & 18 & 18 |
2 | 1 & 1 & 0 | 47 | 19 & 19 & 19 |
3 | 1 & 1 & 1 | 48 | 20 & 20 & 19 |
4 | 2 & 1 & 1 | 49 | 20 & 20 & 20 |
5 | 2 & 2 & 1 | 50 | 21 & 20 & 20 |
6 | 2 & 2 & 2 | 51 | 21 & 21 & 21 |
7 | 3 & 2 & 2 | 52 | 22 & 22 & 22 |
8 | 3 & 3 & 2 | 53 | 23 & 22 & 22 |
9 | 3 & 3 & 3 | 54 | 23 & 23 & 22 |
10 | 4 & 3 & 3 | 55 | 23 & 23 & 23 |
11 | 4 & 4 & 3 | 56 | 24 & 24 & 24 |
12 | 4 & 4 & 4 | 57 | 25 & 24 & 24 |
13 | 4 & 4 & 5 | 58 | 25 & 25 & 25 |
14 | 5 & 5 & 4 | 59 | 26 & 26 & 26 |
15 | 5 & 5 & 5 | 60 | 27 & 26 & 26 |
16 | 6 & 6 & 5 | 61 | 27 & 27 & 27 |
17 | 6 & 6 & 6 | 62 | 28 & 28 & 27 |
18 | 7 & 6 & 6 | 63 | 28 & 28 & 28 |
19 | 7 & 7 & 6 | 64 | 29 & 29 & 28 |
20 | 7 & 7 & 7 | 65 | 29 & 29 & 29 |
21 | 8 & 8 & 7 | 66 | 30 & 30 & 30 |
22 | 8 & 8 & 8 | 67 | 31 & 31 & 31 |
23 | 9 & 8 & 8 | 68 | 32 & 31 & 31 |
24 | 9 & 9 & 9 | 69 | 32 & 32 & 32 |
25 | 10 & 9 & 9 | 70 | 33 & 33 & 33 |
26 | 10 & 10 & 9 | 71 | 34 & 34 & 34 |
27 | 10 & 10 & 10 | 72 | 35 & 35 & 34 |
28 | 11 & 10 & 10 | 73 | 35 & 35 & 35 |
29 | 11 & 11 & 10 | 74 | 36 & 36 & 36 |
30 | 11 & 11 & 11 | 75 | 37 & 37 & 37 |
31 | 12 & 11 & 11 | 76 | 38 & 38 & 38 |
32 | 12 & 12 & 12 | 77 | 39 & 39 & 39 |
33 | 13 & 13 & 12 | 78 | 40 & 40 & 40 |
34 | 13 & 13 & 13 | 79 | 41 & 41 & 41 |
35 | 14 & 13 & 13 | 80 | 42 & 42 & 42 |
36 | 14 & 14 & 14 | 81 | 43 & 42 & 42 |
37 | 15 & 14 & 14 | 82 | 43 & 43 & 43 |
38 | 15 & 15 & 14 | 83 | 44 & 44 & 44 |
39 | 15 & 15 & 15 | 84 | 45 & 45 & 45 |
40 | 16 & 16 & 16 | 85 | 47 & 47 & 47 |
41 | 17 & 16 & 16 | 86 | 48 & 48 & 48 |
42 | 17 & 17 & 16 | 87 | 49 & 49 & 49 |
43 | 17 & 17 & 17 | 88 | 50 & 50 & 50 |
44 | 18 & 17 & 17 | 89 | 52 & 52 & 52 |
45 | 18 & 18 & 18 | 90 | 53 & 53 & 53 |
| | | | |
Table 20.10 | 
|
APPORTIONMENT |
Impairment Rating | Apportioned in Ratio 2:1:1 | Impairment Rating | Apportioned in Ratio 2:1:1 |
1 | 1 & 0 & 0 | 46 | 28 & 14 & 14 |
2 | 1 & 1 & 0 | 47 | 28 & 14 & 14 |
3 | 1 & 1 & 1 | 48 | 29 & 14 & 14 |
4 | 2 & 1 & 1 | 49 | 29 & 15 & 15 |
5 | 3 & 1 & 1 | 50 | 30 & 15 & 15 |
6 | 3 & 2 & 1 | 51 | 31 & 16 & 16 |
7 | 3 & 2 & 2 | 52 | 32 & 16 & 16 |
8 | 4 & 2 & 2 | 53 | 33 & 16 & 16 |
9 | 5 & 2 & 2 | 54 | 34 & 17 & 17 |
10 | 5 & 3 & 2 | 55 | 35 & 17 & 17 |
11 | 5 & 3 & 3 | 56 | 35 & 18 & 17 |
12 | 6 & 3 & 3 | 57 | 36 & 18 & 18 |
13 | 7 & 3 & 3 | 58 | 37 & 19 & 18 |
14 | 7 & 4 & 3 | 59 | 37 & 19 & 19 |
15 | 7 & 4 & 4 | 60 | 38 & 19 & 19 |
16 | 8 & 4 & 4 | 61 | 39 & 20 & 20 |
17 | 9 & 5 & 4 | 62 | 40 & 20 & 20 |
18 | 9 & 5 & 5 | 63 | 41 & 21 & 21 |
19 | 10 & 5 & 5 | 64 | 42 & 21 & 21 |
20 | 11 & 6 & 5 | 65 | 43 & 22 & 21 |
21 | 11 & 6 & 6 | 66 | 44 & 22 & 22 |
22 | 12 & 6 & 6 | 67 | 45 & 23 & 22 |
23 | 13 & 6 & 6 | 68 | 46 & 23 & 23 |
24 | 13 & 7 & 6 | 69 | 47 & 24 & 23 |
25 | 13 & 7 & 7 | 70 | 48 & 24 & 24 |
26 | 14 & 7 & 7 | 71 | 49 & 25 & 24 |
27 | 15 & 7 & 7 | 72 | 50 & 25 & 25 |
28 | 15 & 8 & 8 | 73 | 52 & 26 & 26 |
29 | 16 & 8 & 8 | 74 | 53 & 26 & 26 |
30 | 17 & 8 & 8 | 75 | 54 & 27 & 27 |
31 | 17 & 9 & 9 | 76 | 55 & 27 & 27 |
32 | 18 & 9 & 9 | 77 | 56 & 28 & 28 |
33 | 19 & 9 & 9 | 78 | 57 & 29 & 29 |
34 | 19 & 10 & 10 | 79 | 58 & 29 & 29 |
35 | 20 & 10 & 10 | 80 | 60 & 30 & 30 |
36 | 21 & 10 & 10 | 81 | 61 & 31 & 31 |
37 | 21 & 11 & 10 | 82 | 62 & 31 & 31 |
38 | 21 & 11 & 11 | 83 | 63 & 32 & 32 |
39 | 22 & 11 & 11 | 84 | 64 & 32 & 32 |
40 | 23 & 12 & 12 | 85 | 66 & 33 & 33 |
41 | 24 & 12 & 12 | 86 | 68 & 34 & 34 |
42 | 25 & 12 & 12 | 87 | 69 & 35 & 35 |
43 | 25 & 13 & 13 | 88 | 70 & 35 & 35 |
44 | 26 & 13 & 13 | 89 | 73 & 37 & 37 |
45 | 27 & 14 & 13 | 90 | 74 & 37 & 37 |
| | | | |
| Table 20.11 | 
|
| APPORTIONMENT |
Impairment Rating | Apportioned in Ratio 2:2:1 | Impairment Rating | Apportioned in Ratio 2:2:1 | |
1 | 1 & 0 & 0 | 46 | 22 & 22 & 11 | |
2 | 1 & 1 & 0 | 47 | 23 & 22 & 11 | |
3 | 1 & 1 & 1 | 48 | 24 & 23 & 12 | |
4 | 2 & 1 & 1 | 49 | 24 & 24 & 12 | |
5 | 2 & 2 & 1 | 50 | 25 & 24 & 12 | |
6 | 3 & 2 & 1 | 51 | 25 & 25 & 13 | |
7 | 3 & 3 & 1 | 52 | 26 & 26 & 13 | |
8 | 3 & 3 & 2 | 53 | 27 & 26 & 13 | |
9 | 4 & 3 & 2 | 54 | 28 & 27 & 14 | |
10 | 4 & 4 & 2 | 55 | 28 & 28 & 14 | |
11 | 5 & 4 & 2 | 56 | 29 & 28 & 14 | |
12 | 5 & 5 & 2 | 57 | 29 & 29 & 14 | |
13 | 5 & 5 & 3 | 58 | 30 & 30 & 15 | |
14 | 6 & 5 & 3 | 59 | 31 & 30 & 15 | |
15 | 6 & 6 & 3 | 60 | 31 & 31 & 16 | |
16 | 7 & 6 & 3 | 61 | 32 & 32 & 16 | |
17 | 7 & 7 & 4 | 62 | 33 & 33 & 16 | |
18 | 8 & 8 & 4 | 63 | 34 & 34 & 17 | |
19 | 9 & 8 & 4 | 64 | 35 & 34 & 17 | |
20 | 9 & 9 & 4 | 65 | 35 & 35 & 17 | |
21 | 9 & 9 & 5 | 66 | 36 & 36 & 18 | |
22 | 10 & 9 & 5 | 67 | 37 & 36 & 18 | |
23 | 10 & 10 & 5 | 68 | 38 & 37 & 19 | |
24 | 11 & 10 & 5 | 69 | 38 & 38 & 19 | |
25 | 11 & 11 & 5 | 70 | 39 & 39 & 20 | |
26 | 11 & 11 & 6 | 71 | 40 & 40 & 20 | |
27 | 12 & 11 & 6 | 72 | 41 & 41 & 21 | |
28 | 12 & 12 & 6 | 73 | 42 & 42 & 21 | |
29 | 13 & 13 & 7 | 74 | 43 & 42 & 21 | |
30 | 14 & 13 & 7 | 75 | 43 & 43 & 22 | |
31 | 14 & 14 & 7 | 76 | 44 & 44 & 22 | |
32 | 15 & 14 & 7 | 77 | 46 & 45 & 23 | |
33 | 15 & 15 & 7 | 78 | 46 & 46 & 23 | |
34 | 15 & 15 & 8 | 79 | 48 & 48 & 24 | |
35 | 16 & 16 & 8 | 80 | 49 & 49 & 24 | |
36 | 17 & 16 & 8 | 81 | 50 & 50 & 25 | |
37 | 17 & 17 & 9 | 82 | 51 & 51 & 26 | |
38 | 18 & 17 & 9 | 83 | 52 & 52 & 26 | |
39 | 18 & 18 & 9 | 84 | 53 & 53 & 27 | |
40 | 19 & 18 & 9 | 85 | 54 & 54 & 27 | |
41 | 19 & 19 & 10 | 86 | 56 & 56 & 28 | |
42 | 20 & 20 & 10 | 87 | 58 & 58 & 29 | |
43 | 21 & 20 & 10 | 88 | 59 & 59 & 30 | |
44 | 21 & 21 & 10 | 89 | 60 & 60 & 30 | |
45 | 22 & 21 & 11 | 90 | 62 & 62 & 31 | |
| | | | | | |
Table 20.12 | 
|
APPORTIONMENT |
Impairment Rating | Apportioned in Ratio 3:2:1 | Impairment Rating | Apportioned in Ratio 3:2:1 | |
1 | 1 & 0 & 0 | 46 | 28 & 18 & 9 | |
2 | 1 & 1 & 0 | 47 | 28 & 19 & 9 | |
3 | 2 & 1 & 0 | 48 | 29 & 19 & 10 | |
4 | 2 & 1 & 1 | 49 | 29 & 20 & 10 | |
5 | 2 & 2 & 1 | 50 | 30 & 20 & 10 | |
6 | 3 & 2 & 1 | 51 | 31 & 20 & 10 | |
7 | 4 & 2 & 1 | 52 | 32 & 21 & 11 | |
8 | 4 & 3 & 1 | 53 | 32 & 22 & 11 | |
9 | 5 & 3 & 1 | 54 | 33 & 22 & 11 | |
10 | 5 & 3 & 2 | 55 | 34 & 22 & 11 | |
11 | 5 & 4 & 2 | 56 | 35 & 23 & 12 | |
12 | 6 & 4 & 2 | 57 | 36 & 24 & 12 | |
13 | 7 & 4 & 2 | 58 | 37 & 24 & 12 | |
14 | 7 & 5 & 2 | 59 | 37 & 25 & 12 | |
15 | 7 & 5 & 3 | 60 | 38 & 26 & 13 | |
16 | 8 & 5 & 3 | 61 | 39 & 26 & 13 | |
17 | 9 & 6 & 3 | 62 | 40 & 26 & 13 | |
18 | 10 & 6 & 3 | 63 | 41 & 27 & 14 | |
19 | 10 & 7 & 3 | 64 | 42 & 28 & 14 | |
20 | 11 & 7 & 4 | 65 | 43 & 28 & 14 | |
21 | 11 & 8 & 4 | 66 | 44 & 29 & 15 | |
22 | 12 & 8 & 4 | 67 | 44 & 30 & 15 | |
23 | 13 & 8 & 4 | 68 | 45 & 30 & 15 | |
24 | 13 & 9 & 4 | 69 | 47 & 31 & 16 | |
25 | 13 & 9 & 5 | 70 | 47 & 31 & 16 | |
26 | 14 & 9 & 5 | 71 | 48 & 32 & 16 | |
27 | 14 & 10 & 5 | 72 | 49 & 33 & 17 | |
28 | 15 & 10 & 5 | 73 | 51 & 34 & 17 | |
29 | 16 & 11 & 5 | 74 | 52 & 35 & 17 | |
30 | 17 & 11 & 6 | 75 | 53 & 36 & 18 | |
31 | 17 & 12 & 6 | 76 | 54 & 36 & 18 | |
32 | 18 & 12 & 6 | 77 | 56 & 37 & 19 | |
33 | 19 & 12 & 6 | 78 | 57 & 38 & 19 | |
34 | 19 & 13 & 6 | 79 | 58 & 38 & 19 | |
35 | 20 & 13 & 7 | 80 | 59 & 40 & 20 | |
36 | 20 & 14 & 7 | 81 | 60 & 40 & 20 | |
37 | 21 & 14 & 7 | 82 | 61 & 40 & 20 | |
38 | 22 & 14 & 7 | 83 | 63 & 42 & 21 | |
39 | 22 & 15 & 7 | 84 | 65 & 44 & 22 | |
40 | 23 & 16 & 8 | 85 | 66 & 44 & 22 | |
41 | 24 & 16 & 8 | 86 | 67 & 44 & 22 | |
42 | 25 & 16 & 8 | 87 | 69 & 46 & 23 | |
43 | 25 & 17 & 8 | 88 | 70 & 46 & 23 | |
44 | 26 & 18 & 9 | 89 | 72 & 48 & 24 | |
45 | 27 & 18 & 9 | 90 | 74 & 50 & 25 | |
| | | | | |
Table 20.13 | 
|
APPORTIONMENT |
Impairment Rating | Apportioned in Ratio 1:1:1:1 | Impairment Rating | Apportioned in Ratio 1:1:1:1 | |
1 | 1 & 0 & 0 & 0 | 46 | 15 & 14 & 14 & 14 | |
2 | 1 & 1 & 0 & 0 | 47 | 15 & 15 & 14 & 14 | |
3 | 1 & 1 & 1 & 0 | 48 | 15 & 15 & 15 & 15 | |
4 | 1 & 1 & 1 & 1 | 49 | 16 & 15 & 15 & 15 | |
5 | 2 & 1 & 1 & 1 | 50 | 16 & 16 & 16 & 16 | |
6 | 2 & 2 & 1 & 1 | 51 | 17 & 17 & 16 & 16 | |
7 | 2 & 2 & 2 & 1 | 52 | 17 & 17 & 17 & 16 | |
8 | 2 & 2 & 2 & 2 | 53 | 17 & 17 & 17 & 17 | |
9 | 3 & 2 & 2& 2 | 54 | 18 & 17 & 17 & 17 | |
10 | 3 & 3 & 2 & 2 | 55 | 18 & 18 & 18 & 18 | |
11 | 3 & 3 & 3 & 2 | 56 | 19 & 18 & 18 & 18 | |
12 | 3 & 3 & 3 & 3 | 57 | 19 & 19 & 19 & 19 | |
13 | 4 & 3 & 3 & 3 | 58 | 20 & 20 & 19 & 19 | |
14 | 4 & 4 & 3 & 3 | 59 | 20 & 20 & 20 & 20 | |
15 | 4 & 4 & 4 & 3 | 60 | 21 & 20 & 20 & 20 | |
16 | 4 & 4 & 4 & 4 | 61 | 21 & 21 & 21 & 21 | |
17 | 5 & 5 & 4 & 4 | 62 | 22 & 22 & 22 & 21 | |
18 | 5 & 5 & 5 & 4 | 63 | 22 & 22 & 22 & 22 | |
19 | 5 & 5 & 5 & 5 | 64 | 23 & 23 & 22 & 22 | |
20 | 6 & 6 & 5 & 5 | 65 | 23 & 23 & 23 & 23 | |
21 | 6 & 6 & 6 & 5 | 66 | 24 & 24 & 24 & 23 | |
22 | 6 & 6 & 6 & 6 | 67 | 24 & 24 & 24 & 24 | |
23 | 7 & 6 & 6 & 6 | 68 | 25 & 25 & 25 & 24 | |
24 | 7 & 7 & 6 & 6 | 69 | 25 & 25 & 25 & 25 | |
25 | 7 & 7 & 7 & 6 | 70 | 26 & 26 & 26 & 26 | |
26 | 7 & 7 & 7 & 7 | 71 | 27 & 27 & 26 & 26 | |
27 | 8 & 8 & 8 & 7 | 72 | 27 & 27 & 27 & 27 | |
28 | 8 & 8 & 8 & 8 | 73 | 28 & 28 & 28 & 28 | |
29 | 9 & 8 & 8 & 8 | 74 | 29 & 29 & 28 & 28 | |
30 | 9 & 9 & 9 & 8 | 75 | 29 & 29 & 29 & 29 | |
31 | 9 & 9 & 9 & 9 | 76 | 30 & 30 & 30 & 30 | |
32 | 10 & 9 & 9 & 9 | 77 | 31 & 31 & 31 & 31 | |
33 | 10 & 10 & 9 & 9 | 78 | 32 & 31 & 31 & 31 | |
34 | 10 & 10 & 10 & 10 | 79 | 32 & 32 & 32 & 32 | |
35 | 11 & 10 & 10 & 10 | 80 | 33 & 33 & 33 & 33 | |
36 | 11 & 11 & 10 & 10 | 81 | 34 & 34 & 34 & 34 | |
37 | 11 & 11 & 11 & 10 | 82 | 35 & 35 & 35 & 35 | |
38 | 11 & 11 & 11 & 11 | 83 | 36 & 36 & 36 & 36 | |
39 | 12 & 11 & 11 & 11 | 84 | 37 & 37 & 37 & 37 | |
40 | 12 & 12 & 12 & 12 | 85 | 38 & 38 & 38 & 38 | |
41 | 13 & 13 & 12 & 12 | 86 | 39 & 39 & 39 & 39 | |
42 | 13 & 13 & 13 & 12 | 87 | 40 & 40 & 40 & 40 | |
43 | 13 & 13 & 13 & 13 | 88 | 41 & 41 & 41 & 41 | |
44 | 14 & 14 & 14 & 13 | 89 | 43 & 42 & 42 & 42 | |
45 | 14 & 14 & 14 & 14 | 90 | 43 & 43 & 43 & 43 | |
| | | | | |
CHAPTER 21
PAIRED ORGANS POLICY
INTRODUCTION
The paired organs policy recognises that impairment of the function of only one of a pair of organs can place greater importance on the proper function of the other organ, impairment of which is therefore more disabling than it would otherwise have been.
The policy is to be applied only if the maximum possible impairment from the loss of both organs is more than double the maximum possible impairment from the loss of one organ; and the accepted conditions impair the function of only one organ of a pair. Thus it is applied to hearing, vision, renal function, and the function of testes, ovaries, and adrenals. It is not to be applied to limbs, since the loss of functional unity of the limbs has been allowed for in the impairment ratings of Chapter 3. Chapter 21 is not to be used for hearing loss, as the steps for applying the paired organs policy to hearing loss are contained in Chapter 7 (Ear, Nose, and Throat Impairment).
Applying the paired organs policy
Follow the steps below to calculate the degree of impairment under the paired organs policy.
STEP 1 | Multiply by 2 the impairment rating for the impairment due to the accepted condition to which the paired organs policy applies. |
STEP 2 | Find the total impairment rating for the relevant paired organs. |
STEP 3 | Compare the ratings obtained in Steps 1 and 2. Take the lesser rating. This is the final impairment rating for the paired organ. |
Example
A veteran has a combined monocular assessment of 20 points for an accepted condition of the left eye, and a binocular impairment rating of 35. In Step 1 the 20 points are multiplied by two to get 40 points. This is compared with the binocular impairment rating, and the lesser taken. The veteran therefore gets 35 points after application of the paired organs policy, instead of the 20 points which would have been given if the policy had not applied.
Lifestyle Effects
CHAPTER 22
LIFESTYLE EFFECTS
INTRODUCTION
This chapter is to be used to assess lifestyle effects of accepted conditions.
What is a lifestyle effect?
A lifestyle effect is a disadvantage, resulting from an accepted condition, that limits or prevents the fulfilment of a role that is normal for a veteran of the same age without the accepted condition.
Method of assessment of lifestyle effect for calculating interim impairment payments
When calculating an interim impairment payment amount under subsection 75(2) of the Act, the Commission must allocate a lifestyle rating using the following methodology:
Step (1) Obtain the lifestyle rating for all conditions previously determined;
Step (2) Work out the lifestyle rating for all conditions (including the current condition in respect of which a determination has not been made) using:
(a) the top of the shaded area for impairment points between 0 and 15; or
(b) in any other case — the bottom of the shaded area.
Step (3) Use the higher of the lifestyle ratings from steps 1 and 2 to work out the interim permanent impairment payment.
This method of assessment of lifestyle effect is not to be used when subsection 75(4) of the Act applies.
Optional methods of assessment when all conditions stabilised
There are three optional methods of assessing lifestyle effects. The veteran may choose which of these methods is to be used for his or her assessment. Except where otherwise indicated, the determining authority is to make its assessment on the basis of the last choice made by the veteran and notified to the determining authority. Where no option has been or can be chosen, the determining authority is to determine a lifestyle rating by following the procedure described under “Option 2” below.
Option 1 allows a veteran to self-assess the effects of the accepted conditions on his or her lifestyle. The veteran must complete a Lifestyle Rating Self Assessment Form. The form covers the four key components of lifestyle (personal relationships, mobility, recreational and community activities, and employment and domestic activities) and is in accord with Tables 22.1 to 22.5.
The self-assessed rating should not usually be queried although further information may be requested if necessary. It is expected that the self-assessed lifestyle rating would be broadly consistent with the level of impairment. A determining authority may reject a self-assessment of lifestyle rating because it overestimates, or underestimates, the level of rating that is broadly consistent with the level of impairment from accepted conditions.
If a determining authority rejects a veteran’s self assessment on the ground that it is an underassessment, the determining authority is to substitute its own lifestyle rating for the one chosen by the veteran, provided that the new rating is higher than the original self-assessed rating.
If a determining authority rejects a veteran’s self assessment on the ground that it is an overassessment, the veteran is to be given a second opportunity to complete a Lifestyle Questionnaire. If after having been given the opportunity the veteran completes a Lifestyle Questionnaire, the determining authority is to determine a new lifestyle rating by following the procedure described under “Option 3” below. If after having been given the opportunity the veteran does not complete a Lifestyle Questionnaire, the determining authority is to determine a new lifestyle rating by following the procedure described under “Option 2” below.
Option 2 is to be used if the veteran chooses not to self-assess or to complete a Lifestyle Questionnaire. Under this option the determining authority should generally allocate a lifestyle rating based on the level of medical impairment. This rating is not to be less than the higher of the ratings contained in the “shaded area” of Tables 23.1 and 23.2 in Chapter 23 (Calculating Permanent Impairment Compensation).
In unusual cases the determining authority may, in the light of information available to it, decide to allocate a rating in excess of the higher of the ratings contained in the “shaded area” of Tables 23.1 and 23.2 in Chapter 23 (Calculating Permanent Impairment Compensation).
Option 3 is to be used if the veteran completes a Lifestyle Questionnaire. The determining authority is to use the information in the completed Lifestyle Questionnaire, together with all other relevant information available to it, to allocate ratings in accordance with Tables 22.1 to 22.5. The ratings are to reflect the impact of the impairment from accepted conditions on the four key components of a person’s lifestyle (personal relationships, mobility, recreational and community activities, and employment and domestic activities).
How are lifestyle effects assessed?
The effects of impairment on lifestyle are specific to a veteran. and are determined by reference to four components of that veteran’s life:
- personal relationships,
- mobility,
- recreational and community activities, and
- employment and domestic activities.
All are of equal weight.
Pain, suffering, impaired memory or concentration, or interference with sleep or sleeping arrangements, that result from the accepted conditions must be taken into account. The rating that best accommodates the veteran’s circumstances is to be selected from the descriptions in Tables 22.1 to 22.5.
The criteria in the Lifestyle Rating Self Assessment Form are the same as the criteria in Tables 22.1 to 22.5. Ratings are based on a progressive scale of 0–7 (with the exception of Table 22.5 in which the scale ranges from 0–5). A zero rating indicates that a veteran’s lifestyle is only negligibly affected by the accepted conditions. A rating of 7 indicates that the effect of the accepted conditions on a veteran’s lifestyle is of the utmost severity.
Calculation of lifestyle rating
Follow the steps below to calculate the lifestyle rating, except in those cases where the veteran has made a self-assessment that has been accepted.
STEP 1 | Determine the lifestyle rating from each of Tables 22.1, 22.2, 22.3, 22.4 and 22.5. |
STEP 2 | Compare the lifestyle ratings obtained from Tables 22.4 and 22.5. Take the higher rating. |
STEP 3 | Add together the lifestyle ratings from Tables 22.1, 22.2, 22.3 and the lifestyle rating obtained in Step 2. |
STEP 4 | Divide the number obtained in Step 3 by four. The result of the division is to be rounded to the nearest integer. The fraction of 0.5 is to be rounded up. This is the final lifestyle rating to be used in the assessment. |
PERSONAL RELATIONSHIPS
“Personal relationships” refers to the veteran’s ability to take part in and maintain customary social, sexual and interpersonal relationships.
To determine the effect on personal relationships, it is necessary to establish how the physical and psychological effects of accepted conditions affect the veteran’s ability to interact socially with others.
Lifestyle Effects Table 22.1 | | 
|
PERSONAL RELATIONSHIPS |
Ratings | Criteria |
NIL | No or negligible effect on personal and social relationships. Relationships are satisfying, with full participation in accustomed social and personal activities. |
ONE | Personal and social relationships are fairly satisfying. Intermittent disadvantages may inhibit, but not prevent participation in accustomed range of social and personal activities. |
TWO | Mildly affected personal and social relationships. Social contacts and activities are reduced, veteran’s participation in the accustomed range of activities is restricted. |
THREE | Moderately affected personal and social relationships. Relationships usually confined to family, close friends, colleagues and neighbours. Unable to relate to casual acquaintances. |
FOUR | Markedly affected relationships. Most relations are unsatisfying, maintenance of usual relations with relatives, friends, neighbours and colleagues is difficult. Much less time is spent socialising than was the case formerly. |
FIVE | Severely affected relationships. Able to relate only to particular, or few people, eg spouse or children. These remaining relationships are strained and of low quality. |
SIX | Extreme difficulty in relating to anyone, for example: - difficulties in relating because of psychosis; or
- social interaction limited to carer(s) due to confinement; or
ability to communicate is restricted due to stroke or other effect of accepted conditions. |
SEVEN | Unable to relate to anyone. All relationships are prevented. |
| One rating from this table is to be selected. |
| | | |
MOBILITY
The mobility rating measures the effects of the accepted conditions on the veteran’s mobility. “Mobility” refers to the veteran’s ability to move about effectively in carrying out the ordinary activities of life. It allows for the veteran’s ability to use available forms of transport. Lack of public transport is not to be taken into account.
Both physical and psychological impediments to mobility are to be taken into account when applying Table 22.2. Restrictions on mobility due to mental health factors (e.g. agoraphobia, claustrophobia, dementia, anxiety, confusion, etc), or sensory deficit (e.g. hearing loss, or reduced vision) should be rated in the same way as the more obvious restrictions due to physical impairment.
| | |
MOBILITY |
Allowance for accepted mental conditions is possible in the rating of effects on mobility and hence on lifestyle. |
Ratings | Criteria |
NIL | |
ONE | Intermittent or periodic effects on mobility: - mobility affected only when impairment eg migraine, angina, sciatica, or panic attack, is present. Between attacks there are no restrictions;
- if there is permanent impairment, eg night blindness, the effect is only sporadically limiting.
|
TWO | Mild effects on mobility, eg slowing of pace in some circumstances, or need for a walking stick. |
| Moderately reduced mobility: - mobility curtained or diminished because of frailty, lack of confidence; or moderate agoraphobia;
- travel as a passenger, in private and public transport, possible in most circumstances without undue difficulty (‘undue difficulty’ not being the need for a break in travel or for special seating arrangements);
- dependent on a walking stick or similar device. Independent in leaving home and reaching destination, but has some difficulty.
|
FOUR | Markedly reduced mobility: - assistance is needed to cope with public or private transport;
- there is considerable difficulty in travelling from home to destination;
- restricted in the use of at least two forms of public transport..
|
FIVE | Major impediments to mobility: - dependent upon others, or mechanical devices such as wheelchairs;
- unable to use most forms of public transport;
- able to drive a car only in a situation of emergency and then only for a short distance.
|
SIX | Severe impediments to mobility: - restricted to home and immediate vicinity, unless door to door transport and assistance from others are provided;
- unable to drive a car in any circumstances whatever.
|
SEVEN | Restricted to room or chair: - severe agoraphobia permanently confines veteran to home;
- dependent upon others, or hoists or similar appliances, for getting in and out of bed.
|
| One rating from this table is to be selected. |
| | | |
RECREATIONAL AND COMMUNITY ACTIVITIES
This refers to the ability to take part in any activities of the veteran’s choosing.
A recreational rating is based on the veteran’s normal recreational and community activities and measures the limitation placed by the accepted conditions on the ability to continue those activities. The table takes into account the veteran’s need to modify recreational pursuits or to seek alternatives. Community activities include welfare work in a voluntary capacity.
Lifestyle EffectsTable 22.3 | | 
|
RECREATIONAL AND COMMUNITY ACTIVITIES |
Ratings | Criteria |
NIL | Able to undertake the full range of usual recreational pursuits and community activities. |
ONE | Intermittent interference with recreational pursuits and community activities. Between episodes is able to continue with the range of accustomed recreational pursuits and community activities. |
TWO | Mild but constant interference with accustomed recreational pursuits and community activities, but is able to continue with them — even if less frequently — or to enjoy alternatives. |
THREE | Unable to continue some accustomed recreational pursuits and community activities, for example: - competition sporting activities (golf, tennis, bowls, etc) but is still able to enjoy most other activities (camping out, hobbies, going visiting, watching sport, etc);
- unable to perform some community or voluntary activities involving physical activity (eg working bees) but is still able to participate in most other activities including welfare work, fund raising work etc.
|
FOUR | Unable to take part in formerly favoured recreational pursuits, leisure and community activities, but less physical activities are possible, for example: - restricted to generally non-active interests (eg music, art, stamp or coin collecting, attending clubs, etc); and
- unable to participate in accustomed activities (eg camping, going for long walks, fishing, voluntary activities such as meals on wheels).
|
FIVE | Greater reduction in the number and kind of recreational activities which can be undertaken; some assistance is needed to undertake those which are still possible, for example: - can only visit or go out if taken to and from destination;
- finds doing a hobby or relaxing (for example, stamp collecting, art & crafts, playing or listening to music, playing cards, etc.) difficult to enjoy due to pain, suffering, or loss of dexterity.
|
SIX | Able to engage in only a very few satisfying recreational activities. Restricted to a few passive activities such as watching TV, listening to radio, reading or receiving visitors. |
SEVEN | Unable to take part in any recreational activities. |
| One rating from this table is to be selected. |
| | | |
No age adjustment permitted for this table
DOMESTIC AND EMPLOYMENT ACTIVITIES
There are two tables for this lifestyle component. A lifestyle rating is to be selected from each table, where applicable, and the higher of the two lifestyle ratings is to be chosen as the lifestyle rating for domestic and employment activities.
Domestic Activities
“Domestic activity” refers to the veteran’s ability to sustain effective routines in a domestic environment. Only the impact of accepted conditions on the ability to engage in domestic activity is to be taken into account: the veteran’s inability to do domestic work for some other reason (for example, choice, habit, inexperience, lack of skill) is not to be taken into account.
Lifestyle EffectsTable 22.4 | | 
|
DOMESTIC ACTIVITIES |
Ratings | Criteria |
NIL | Able to sustain any usual activities. |
ONE | Intermittent effects of accepted disablement on usual activity. |
TWO | Able to carry out accustomed tasks, but has difficulty with some heavier tasks, for example: - has difficulty with heavy gardening activities such as digging, pruning trees etc.
|
THREE | Unable to perform heavy activities, but able to carry out lighter household tasks, taking breaks during sustained activity, for example: - mowing the lawn;
- washing the car;
- performing light maintenance or gardening activities if working at own pace, taking breaks as necessary.
|
FOUR | Unable to carry out a full range of normal household activities, particularly some moderate tasks which require exertion. Needs assistance with some activities, for example: - vacuuming carpets, cleaning floors, or mowing lawns;
- home repairs and maintenance, etc.
|
FIVE | Limitation of household activity to a small range of light tasks, for example: - watering the garden but has difficulty in weeding or pruning;
- able to do some light household activities but has difficulty bending to make beds, or in putting out the rubbish bin;
- requires assistance with grocery shopping.
|
SIX | Able to carry out only very limited domestic activities, usually a restricted range of indoor activities. May require supervision in carrying out such activities, for example: - able to do very light tidying, dusting but unable to cook or prepare meals;
- has difficulty standing to set table or wash dishes.
|
SEVEN | Total dependency upon others for domestic tasks. |
| One rating from this table is to be selected. |
Employment Activities
“Employment activities” refers to the veteran’s ability to work. An employment rating is based on the effects of the accepted conditions on the ability to work for remuneration. It should take into account any necessary changes or modifications to employment or the workplace.
Ratings from Table 22.5 do not confer on the veteran an earnings related benefit, but are intended to compensate for the adverse effects (other than loss of income) of unemployment, reduced employment, or diminished quality of working life.
There are only six criteria on Table 22.5.
Lifestyle EffectsTable 22.5 | | |
EMPLOYMENT ACTIVITIES |
Ratings | Criteria |
NIL | Able to engage in usual employment. |
ONE | Able to carry out usual employment that is affected intermittently. |
TWO | Able to follow accustomed employment but difficulty is experienced in carrying out full range of occupational activities. |
THREE | Unable to follow accustomed employment without modification to workplace, provision of aids or restructuring of tasks. |
FOUR | Either unable to work full time in normal occupation, or has had to change occupation or number of hours worked, or both, because of the accepted conditions. |
FIVE | Unable to work. |
| One rating from this table is to be selected. |
| | | |
CALCULATING PERMANENT IMPAIRMENT COMPENSATION
Chapter 23
CALCULATING PERMANENT IMPAIRMENT COMPENSATION
Section 67 of the Military Rehabilitation and Compensation Act 2004 provides that this Guide can specify how the Military Rehabilitation and Compensation Commission is to determine the compensation payable to a person under Part 2 of that Act.
Different factors apply for any combination of impairment (no rounding up or down) and lifestyle effect (where rounding to nearest integer is allowed). Once a rating of 80 impairment points is achieved no lifestyle needs to be calculated as this rating pays the maximum weekly payment under the Act. The maximum payment is payable at 80 impairment points for all types of service.
Warlike, non-warlike and peacetime service
Table 1 is for warlike and non-warlike service. Table 2 is for peacetime service. The factors for warlike and non-warlike service reflect a premium where impairment has resulted from that service rather than peacetime service.
The differential lessens as impairment rates over 50 points are reached. Impairment of 80 or more points attracts the same level of compensation regardless of the nature of the service that gave rise to the injury or disease.
How to calculate a weekly compensation payment
Petty Officer Andrews is 28 when she applies for compensation. It is determined that she has incapacity caused by an injury suffered on non-warlike service. She is assessed as having an impairment rating of 15 and 1 lifestyle point.
From the table for non-warlike service the factor for her injury is .155.
The maximum payment is $245.82 per week. When this amount is factored she is entitled to $38.10 per week (note that the maximum payment amount is indexed annually on 1 July).
Combining impairment ratings
If all accepted conditions have been given impairment ratings, the ratings are to be combined by applying Table 18.1 (Combined Values Chart) in this Guide.
Details on how to apply Table 18.1 are given in Chapter 18.
However, the combined impairment rating obtained by applying Table 18.1 (Combined Values Chart) is not to be rounded. Rounding is unnecessary since impairment periodic payments are based on whatever impairment rating is determined and are not in multiples of 5 or 10 as in the VEA.
Determining the factor for compensation payment
The combined impairment rating which is obtained by applying Chapter 18 (Combined Values Chart) is to be combined with the lifestyle rating on either the Warlike and Non-warlike Factors Table (Table 23.1) or the Peacetime Factors Table (Table 23.2). This is to determine the factor to be multiplied by the maximum lump sum payment available under the Act.
A veteran’s lifestyle rating is expected to be broadly consistent with the degree of medical impairment from accepted conditions as measured by the Combined Impairment Rating. In most cases a lifestyle rating that falls within the shaded area of Tables 23.1 and 23.2 will satisfy the requirement of broad consistency. There may be exceptional cases and, in accordance with Chapter 22 of this Guide, a lifestyle rating outside the shaded area may be allocated.
Where a member or former member has two or more types of service and different conditions under each then the instructions on “Combined Ratings” apply.
Table 23.1: COMPENSATION FACTORS FOR CALCULATING PERMANENT IMPAIRMENT COMPENSATION - WARLIKE AND NON-WARLIKE SERVICE
| Lifestyle | | | | | | |
Impairment | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
0 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
5 | 0.044 | 0.067 | 0.089 | 0.111 | 0.133 | 0.156 | 0.178 | 0.200 |
6 | 0.053 | 0.075 | 0.098 | 0.120 | 0.142 | 0.165 | 0.187 | 0.209 |
7 | 0.062 | 0.084 | 0.107 | 0.129 | 0.151 | 0.173 | 0.196 | 0.218 |
8 | 0.071 | 0.093 | 0.115 | 0.138 | 0.160 | 0.182 | 0.205 | 0.227 |
9 | 0.080 | 0.102 | 0.124 | 0.147 | 0.169 | 0.191 | 0.213 | 0.236 |
10 | 0.088 | 0.111 | 0.133 | 0.155 | 0.178 | 0.200 | 0.222 | 0.245 |
11 | 0.097 | 0.120 | 0.142 | 0.164 | 0.187 | 0.209 | 0.231 | 0.253 |
12 | 0.106 | 0.128 | 0.151 | 0.173 | 0.195 | 0.218 | 0.240 | 0.262 |
13 | 0.115 | 0.137 | 0.160 | 0.182 | 0.204 | 0.227 | 0.249 | 0.271 |
14 | 0.124 | 0.146 | 0.168 | 0.191 | 0.213 | 0.235 | 0.258 | 0.280 |
15 | 0.133 | 0.155 | 0.177 | 0.200 | 0.222 | 0.244 | 0.267 | 0.289 |
16 | 0.142 | 0.164 | 0.186 | 0.208 | 0.231 | 0.253 | 0.275 | 0.298 |
17 | 0.150 | 0.173 | 0.195 | 0.217 | 0.240 | 0.262 | 0.284 | 0.307 |
18 | 0.159 | 0.182 | 0.204 | 0.226 | 0.248 | 0.271 | 0.293 | 0.315 |
19 | 0.168 | 0.190 | 0.213 | 0.235 | 0.257 | 0.280 | 0.302 | 0.324 |
20 | 0.177 | 0.199 | 0.222 | 0.244 | 0.266 | 0.288 | 0.311 | 0.333 |
21 | 0.186 | 0.208 | 0.230 | 0.253 | 0.275 | 0.297 | 0.320 | 0.342 |
22 | 0.195 | 0.217 | 0.239 | 0.262 | 0.284 | 0.306 | 0.328 | 0.351 |
23 | 0.203 | 0.226 | 0.248 | 0.270 | 0.293 | 0.315 | 0.337 | 0.360 |
24 | 0.212 | 0.235 | 0.257 | 0.279 | 0.302 | 0.324 | 0.346 | 0.368 |
25 | 0.221 | 0.243 | 0.266 | 0.288 | 0.310 | 0.333 | 0.355 | 0.377 |
26 | 0.230 | 0.252 | 0.275 | 0.297 | 0.319 | 0.342 | 0.364 | 0.386 |
27 | 0.239 | 0.261 | 0.283 | 0.306 | 0.328 | 0.350 | 0.373 | 0.395 |
28 | 0.248 | 0.270 | 0.292 | 0.315 | 0.337 | 0.359 | 0.382 | 0.404 |
29 | 0.257 | 0.279 | 0.301 | 0.323 | 0.346 | 0.368 | 0.390 | 0.413 |
30 | 0.265 | 0.288 | 0.310 | 0.332 | 0.355 | 0.377 | 0.399 | 0.422 |
31 | 0.274 | 0.297 | 0.319 | 0.341 | 0.363 | 0.386 | 0.408 | 0.430 |
32 | 0.283 | 0.305 | 0.328 | 0.350 | 0.372 | 0.395 | 0.417 | 0.439 |
33 | 0.292 | 0.314 | 0.337 | 0.359 | 0.381 | 0.403 | 0.426 | 0.448 |
34 | 0.301 | 0.323 | 0.345 | 0.368 | 0.390 | 0.412 | 0.435 | 0.457 |
35 | 0.310 | 0.332 | 0.354 | 0.377 | 0.399 | 0.421 | 0.443 | 0.466 |
36 | 0.318 | 0.341 | 0.363 | 0.385 | 0.408 | 0.430 | 0.452 | 0.475 |
37 | 0.327 | 0.350 | 0.372 | 0.394 | 0.417 | 0.439 | 0.461 | 0.483 |
38 | 0.336 | 0.358 | 0.381 | 0.403 | 0.425 | 0.448 | 0.470 | 0.492 |
39 | 0.345 | 0.367 | 0.390 | 0.412 | 0.434 | 0.457 | 0.479 | 0.501 |
40 | 0.354 | 0.376 | 0.398 | 0.421 | 0.443 | 0.465 | 0.488 | 0.510 |
41 | 0.363 | 0.385 | 0.407 | 0.430 | 0.452 | 0.474 | 0.497 | 0.519 |
42 | 0.372 | 0.394 | 0.416 | 0.438 | 0.461 | 0.483 | 0.505 | 0.528 |
43 | 0.380 | 0.403 | 0.425 | 0.447 | 0.470 | 0.492 | 0.514 | 0.537 |
44 | 0.389 | 0.412 | 0.434 | 0.456 | 0.478 | 0.501 | 0.523 | 0.545 |
45 | 0.398 | 0.420 | 0.443 | 0.465 | 0.487 | 0.510 | 0.532 | 0.554 |
46 | 0.407 | 0.429 | 0.452 | 0.474 | 0.496 | 0.518 | 0.541 | 0.563 |
47 | 0.416 | 0.438 | 0.460 | 0.483 | 0.505 | 0.527 | 0.550 | 0.572 |
48 | 0.425 | 0.447 | 0.469 | 0.492 | 0.514 | 0.536 | 0.558 | 0.581 |
49 | 0.434 | 0.456 | 0.478 | 0.500 | 0.523 | 0.545 | 0.567 | 0.590 |
50 | 0.442 | 0.465 | 0.487 | 0.509 | 0.532 | 0.554 | 0.576 | 0.598 |
51 | 0.461 | 0.483 | 0.504 | 0.526 | 0.547 | 0.569 | 0.590 | 0.612 |
52 | 0.480 | 0.500 | 0.521 | 0.542 | 0.563 | 0.584 | 0.604 | 0.625 |
53 | 0.498 | 0.518 | 0.538 | 0.558 | 0.578 | 0.598 | 0.619 | 0.639 |
54 | 0.517 | 0.536 | 0.555 | 0.575 | 0.594 | 0.613 | 0.633 | 0.652 |
55 | 0.535 | 0.554 | 0.572 | 0.591 | 0.610 | 0.628 | 0.647 | 0.665 |
56 | 0.554 | 0.572 | 0.590 | 0.607 | 0.625 | 0.643 | 0.661 | 0.679 |
57 | 0.572 | 0.590 | 0.607 | 0.624 | 0.641 | 0.658 | 0.675 | 0.692 |
58 | 0.591 | 0.607 | 0.624 | 0.640 | 0.656 | 0.673 | 0.689 | 0.706 |
59 | 0.610 | 0.625 | 0.641 | 0.656 | 0.672 | 0.688 | 0.703 | 0.719 |
60 | 0.628 | 0.643 | 0.658 | 0.673 | 0.688 | 0.703 | 0.717 | 0.732 |
61 | 0.647 | 0.661 | 0.675 | 0.689 | 0.703 | 0.717 | 0.732 | 0.746 |
62 | 0.665 | 0.679 | 0.692 | 0.706 | 0.719 | 0.732 | 0.746 | 0.759 |
63 | 0.684 | 0.697 | 0.709 | 0.722 | 0.735 | 0.747 | 0.760 | 0.772 |
64 | 0.703 | 0.714 | 0.726 | 0.738 | 0.750 | 0.762 | 0.774 | 0.786 |
65 | 0.721 | 0.732 | 0.743 | 0.755 | 0.766 | 0.777 | 0.788 | 0.799 |
66 | 0.740 | 0.750 | 0.761 | 0.771 | 0.781 | 0.792 | 0.802 | 0.813 |
67 | 0.758 | 0.768 | 0.778 | 0.787 | 0.797 | 0.807 | 0.816 | 0.826 |
68 | 0.777 | 0.786 | 0.795 | 0.804 | 0.813 | 0.822 | 0.830 | 0.839 |
69 | 0.796 | 0.804 | 0.812 | 0.820 | 0.828 | 0.836 | 0.845 | 0.853 |
70 | 0.814 | 0.822 | 0.829 | 0.836 | 0.844 | 0.851 | 0.859 | 0.866 |
71 | 0.833 | 0.839 | 0.846 | 0.853 | 0.859 | 0.866 | 0.873 | 0.880 |
72 | 0.851 | 0.857 | 0.863 | 0.869 | 0.875 | 0.881 | 0.887 | 0.893 |
73 | 0.870 | 0.875 | 0.880 | 0.885 | 0.891 | 0.896 | 0.901 | 0.906 |
74 | 0.888 | 0.893 | 0.897 | 0.902 | 0.906 | 0.911 | 0.915 | 0.920 |
75 | 0.907 | 0.911 | 0.914 | 0.918 | 0.922 | 0.926 | 0.929 | 0.933 |
76 | 0.926 | 0.929 | 0.932 | 0.935 | 0.938 | 0.941 | 0.943 | 0.946 |
77 | 0.944 | 0.946 | 0.949 | 0.951 | 0.953 | 0.955 | 0.958 | 0.960 |
78 | 0.963 | 0.964 | 0.966 | 0.967 | 0.969 | 0.970 | 0.972 | 0.973 |
79 | 0.981 | 0.982 | 0.983 | 0.984 | 0.984 | 0.985 | 0.986 | 0.987 |
80 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
For impairment greater than 80 points, the value is always 1.00.
Table 23.2: COMPENSATION FACTORS FOR CALCULATING PERMANENT IMPAIRMENT COMPENSATION - PEACETIME SERVICE
| Lifestyle | | | | | | |
Impairment | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
0 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
5 | 0.025 | 0.037 | 0.050 | 0.062 | 0.075 | 0.087 | 0.100 | 0.112 |
6 | 0.030 | 0.042 | 0.055 | 0.067 | 0.080 | 0.092 | 0.105 | 0.117 |
7 | 0.035 | 0.047 | 0.060 | 0.072 | 0.085 | 0.097 | 0.110 | 0.122 |
8 | 0.040 | 0.052 | 0.065 | 0.077 | 0.090 | 0.102 | 0.114 | 0.127 |
9 | 0.045 | 0.057 | 0.070 | 0.082 | 0.094 | 0.107 | 0.119 | 0.132 |
10 | 0.050 | 0.062 | 0.074 | 0.087 | 0.099 | 0.112 | 0.124 | 0.137 |
11 | 0.054 | 0.067 | 0.079 | 0.092 | 0.104 | 0.117 | 0.129 | 0.142 |
12 | 0.059 | 0.072 | 0.084 | 0.097 | 0.109 | 0.122 | 0.134 | 0.147 |
13 | 0.064 | 0.077 | 0.089 | 0.102 | 0.114 | 0.127 | 0.139 | 0.152 |
14 | 0.069 | 0.082 | 0.094 | 0.107 | 0.119 | 0.132 | 0.144 | 0.157 |
15 | 0.074 | 0.087 | 0.099 | 0.112 | 0.124 | 0.137 | 0.149 | 0.162 |
16 | 0.079 | 0.092 | 0.104 | 0.117 | 0.129 | 0.142 | 0.154 | 0.167 |
17 | 0.084 | 0.097 | 0.109 | 0.122 | 0.134 | 0.147 | 0.159 | 0.172 |
18 | 0.089 | 0.102 | 0.114 | 0.127 | 0.139 | 0.152 | 0.164 | 0.176 |
19 | 0.094 | 0.107 | 0.119 | 0.131 | 0.144 | 0.156 | 0.169 | 0.181 |
20 | 0.099 | 0.111 | 0.124 | 0.136 | 0.149 | 0.161 | 0.174 | 0.186 |
21 | 0.104 | 0.116 | 0.129 | 0.141 | 0.154 | 0.166 | 0.179 | 0.191 |
22 | 0.109 | 0.121 | 0.134 | 0.146 | 0.159 | 0.171 | 0.184 | 0.196 |
23 | 0.114 | 0.126 | 0.139 | 0.151 | 0.164 | 0.176 | 0.189 | 0.201 |
24 | 0.119 | 0.131 | 0.144 | 0.156 | 0.169 | 0.181 | 0.194 | 0.206 |
25 | 0.124 | 0.136 | 0.149 | 0.161 | 0.174 | 0.186 | 0.199 | 0.211 |
26 | 0.129 | 0.141 | 0.154 | 0.166 | 0.179 | 0.191 | 0.204 | 0.216 |
27 | 0.134 | 0.146 | 0.159 | 0.171 | 0.184 | 0.196 | 0.209 | 0.221 |
28 | 0.139 | 0.151 | 0.164 | 0.176 | 0.189 | 0.201 | 0.213 | 0.226 |
29 | 0.144 | 0.156 | 0.169 | 0.181 | 0.193 | 0.206 | 0.218 | 0.231 |
30 | 0.149 | 0.161 | 0.173 | 0.186 | 0.198 | 0.211 | 0.223 | 0.236 |
31 | 0.153 | 0.166 | 0.178 | 0.191 | 0.203 | 0.216 | 0.228 | 0.241 |
32 | 0.158 | 0.171 | 0.183 | 0.196 | 0.208 | 0.221 | 0.233 | 0.246 |
33 | 0.163 | 0.176 | 0.188 | 0.201 | 0.213 | 0.226 | 0.238 | 0.251 |
34 | 0.168 | 0.181 | 0.193 | 0.206 | 0.218 | 0.231 | 0.243 | 0.256 |
35 | 0.173 | 0.186 | 0.198 | 0.211 | 0.223 | 0.236 | 0.248 | 0.261 |
36 | 0.178 | 0.191 | 0.203 | 0.216 | 0.228 | 0.241 | 0.253 | 0.266 |
37 | 0.183 | 0.196 | 0.208 | 0.221 | 0.233 | 0.246 | 0.258 | 0.271 |
38 | 0.188 | 0.201 | 0.213 | 0.226 | 0.238 | 0.251 | 0.263 | 0.275 |
39 | 0.193 | 0.206 | 0.218 | 0.230 | 0.243 | 0.255 | 0.268 | 0.280 |
40 | 0.198 | 0.210 | 0.223 | 0.235 | 0.248 | 0.260 | 0.273 | 0.285 |
41 | 0.203 | 0.215 | 0.228 | 0.240 | 0.253 | 0.265 | 0.278 | 0.290 |
42 | 0.208 | 0.220 | 0.233 | 0.245 | 0.258 | 0.270 | 0.283 | 0.295 |
43 | 0.213 | 0.225 | 0.238 | 0.250 | 0.263 | 0.275 | 0.288 | 0.300 |
44 | 0.218 | 0.230 | 0.243 | 0.255 | 0.268 | 0.280 | 0.293 | 0.305 |
45 | 0.223 | 0.235 | 0.248 | 0.260 | 0.273 | 0.285 | 0.298 | 0.310 |
46 | 0.228 | 0.240 | 0.253 | 0.265 | 0.278 | 0.290 | 0.303 | 0.315 |
47 | 0.233 | 0.245 | 0.258 | 0.270 | 0.283 | 0.295 | 0.308 | 0.320 |
48 | 0.238 | 0.250 | 0.263 | 0.275 | 0.288 | 0.300 | 0.312 | 0.325 |
49 | 0.243 | 0.255 | 0.268 | 0.280 | 0.292 | 0.305 | 0.317 | 0.330 |
50 | 0.248 | 0.260 | 0.272 | 0.285 | 0.297 | 0.310 | 0.322 | 0.335 |
51 | 0.273 | 0.285 | 0.297 | 0.309 | 0.321 | 0.333 | 0.345 | 0.357 |
52 | 0.298 | 0.309 | 0.321 | 0.333 | 0.344 | 0.356 | 0.368 | 0.379 |
53 | 0.323 | 0.334 | 0.345 | 0.356 | 0.368 | 0.379 | 0.390 | 0.401 |
54 | 0.348 | 0.359 | 0.369 | 0.380 | 0.391 | 0.402 | 0.413 | 0.424 |
55 | 0.373 | 0.383 | 0.394 | 0.404 | 0.415 | 0.425 | 0.435 | 0.446 |
56 | 0.398 | 0.408 | 0.418 | 0.428 | 0.438 | 0.448 | 0.458 | 0.468 |
57 | 0.423 | 0.433 | 0.442 | 0.452 | 0.461 | 0.471 | 0.480 | 0.490 |
58 | 0.448 | 0.457 | 0.466 | 0.476 | 0.485 | 0.494 | 0.503 | 0.512 |
59 | 0.473 | 0.482 | 0.491 | 0.499 | 0.508 | 0.517 | 0.526 | 0.534 |
60 | 0.498 | 0.507 | 0.515 | 0.523 | 0.532 | 0.540 | 0.548 | 0.557 |
61 | 0.523 | 0.531 | 0.539 | 0.547 | 0.555 | 0.563 | 0.571 | 0.579 |
62 | 0.549 | 0.556 | 0.563 | 0.571 | 0.578 | 0.586 | 0.593 | 0.601 |
63 | 0.574 | 0.581 | 0.588 | 0.595 | 0.602 | 0.609 | 0.616 | 0.623 |
64 | 0.599 | 0.605 | 0.612 | 0.619 | 0.625 | 0.632 | 0.639 | 0.645 |
65 | 0.624 | 0.630 | 0.636 | 0.642 | 0.649 | 0.655 | 0.661 | 0.667 |
66 | 0.649 | 0.655 | 0.660 | 0.666 | 0.672 | 0.678 | 0.684 | 0.690 |
67 | 0.674 | 0.679 | 0.685 | 0.690 | 0.696 | 0.701 | 0.706 | 0.712 |
68 | 0.699 | 0.704 | 0.709 | 0.714 | 0.719 | 0.724 | 0.729 | 0.734 |
69 | 0.724 | 0.729 | 0.733 | 0.738 | 0.742 | 0.747 | 0.752 | 0.756 |
70 | 0.749 | 0.753 | 0.757 | 0.762 | 0.766 | 0.770 | 0.774 | 0.778 |
71 | 0.774 | 0.778 | 0.782 | 0.785 | 0.789 | 0.793 | 0.797 | 0.800 |
72 | 0.799 | 0.803 | 0.806 | 0.809 | 0.813 | 0.816 | 0.819 | 0.823 |
73 | 0.824 | 0.827 | 0.830 | 0.833 | 0.836 | 0.839 | 0.842 | 0.845 |
74 | 0.850 | 0.852 | 0.854 | 0.857 | 0.859 | 0.862 | 0.864 | 0.867 |
75 | 0.875 | 0.877 | 0.879 | 0.881 | 0.883 | 0.885 | 0.887 | 0.889 |
76 | 0.900 | 0.901 | 0.903 | 0.905 | 0.906 | 0.908 | 0.910 | 0.911 |
77 | 0.925 | 0.926 | 0.927 | 0.928 | 0.930 | 0.931 | 0.932 | 0.933 |
78 | 0.950 | 0.951 | 0.951 | 0.952 | 0.953 | 0.954 | 0.955 | 0.956 |
79 | 0.975 | 0.975 | 0.976 | 0.976 | 0.977 | 0.977 | 0.977 | 0.978 |
80 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
For impairment greater than 80 points, the value is always 1.00.
Combined ratings
If the two service-caused conditions lead to impairment ratings of A for warlike (or non-warlike) service and B for peacetime service, then the compensation payable will be a weighted average. This is determined on the amount that would be paid if they both were caused by warlike (or non-warlike) and both by peacetime service. The weights used are the impairment ratings A and B. If the combined impairment is C (see Chapter 18) and the lifestyle effect is L, this can be expressed as:
CFfinal(C,L) = | A * CFwl(C,L) + B * CFpt(C,L) (A + B) |
where the CF values for warlike (or non-warlike) and peacetime service are taken from the relevant tables the final value of CF is applied to determine the final level of compensation.
Captain Brown has two conditions, a gastro-intestinal condition (A) resulting from warlike service assessed as 20 impairment points and a spinal injury (B) resulting from peacetime service assessed as 30 impairment points.
The lifestyle rating (L) from these conditions is 4.
The combined impairment rating (C) is 44.
The compensation factor that would be applied if both conditions resulted from warlike service would be 0.478.
If both conditions resulted from peacetime service it would be 0.268.
The weighted average, using the above formula, is (20 * 0.478 + 30 * 0.268)/(20 + 30) or 0.352.
The maximum compensation payable of $245.82 is multiplied by this factor to give a periodic payment of $86.53 per week.
Note: If the gastro-intestinal condition had arisen from peacetime service and the spinal condition from warlike service, with the same impairment and lifestyle ratings, the final compensation factor would be (30 * 0.478 + 20 * 0.268)/(30 + 20) or 0.394, with a periodic payment of $96.85 per week.
Chapter 24
CONVERTING WEEKLY SUMS INTO LUMP SUMS
Once the MRCC determines that compensation is payable under any of sections 68, 71 or 75(2) of the Act it must notify the claimant of the weekly amount of compensation and advise if it may be converted wholly or partly into a lump sum.
A member may accept the weekly payment for life or convert all or part of it to a lump sum using factors approved by the Australian Government Actuary.
The convertible amount
The convertible amount (see section 78) is the weekly amount of compensation that is payable.
If the convertible amount is less than 10% of the maximum weekly amount payable under the Military Rehabilitation and Compensation Act 2004, the person may convert the entire amount to a lump sum.
If the convertible amount is at least 10% but not more than 20% of the maximum weekly amount payable under the Act then the person may convert 50% or 100% to a lump sum.
If the convertible amount is more than 20% of the maximum weekly amount payable under the Act then the person may convert 25%, 50%, 75% or 100% to a lump sum.
Chapter 25
METHOD OF WORKING OUT THE AMOUNT OF
COMPENSATION PAYABLE UNDER THE MRCA FOR A
PERSON WITH A VEA OR SRCA INJURY OR DISEASE
This Chapter deals with situations where an injury or disease (the condition) has been accepted under the VEA and/or the SRCA before a claim is made under the MRCA.
Definitions
In this Chapter:
MRCA determination, in relation to a person, means the determination by the Commission of the degree of impairment suffered by the person as a result of a compensable condition under the Act.
MCRA accepted condition means the injury or disease for which the Commission has accepted liability under section 23 of the Act.
MRCA compensation payment means the payment worked out under this Chapter for a person with a MRCA condition and a SRCA condition and/or a VEA condition.
MRCA PI, means MRCA Permanent Impairment.
MRCA Permanent Impairment, in relation to a person, means the person’s impairment for which compensation is payable under Chapter 4 of Part 2 of the Act.
SRCA accepted condition, in relation to a person, means the person’s injury for which Comcare is liable to pay compensation under the Safety, Rehabilitation and Compensation Act 1988 (SRCA).
Note (1): under s.5A of the SRCA “injury” includes “disease”.
Note (2): under s147 of the SRCA, for defence-related claims Comcare means the Military Rehabilitation and Compensation Commission.
VEA accepted condition, in relation to a person, means the person’s incapacity from an injury or disease that the Repatriation Commission has determined under section 19 of the Veterans’ Entitlements Act 1986 (including as affected by section 71 of that Act) entitles the person to be granted a pension.
VEA percentage means the amount of disability pension payable under the VEA for the conditions referred to in Step 1 as at the date of the MRCA claim expressed as a percentage of the General Rate at that date.
weekly disability pension , means a pension at half the rate at which pension would be payable to a veteran under section 22, 23, 24 or 25 of the Veterans’ Entitlements Act 1986.
The method to assess the total amount of MRCA PI compensation payable under the MRCA is as follows:
Step (1) Use GARP M to assess, as at the date of the MRCA determination the combined effect of :
(a) all MRCA accepted conditions; and
(b) any VEA accepted conditions and any SRCA accepted conditions which were accepted conditions on the date the person claimed MRCA PI;
to work out the resulting compensation that would notionally be payable under MRCA.
Step (2) Assess whether, under this Guide, the MRCA accepted condition contributes at least five impairment points to the overall impairment rating:
(a) if the MRCA accepted condition contributes at least five impairment points to the overall impairment rating, compensation for that condition may be payable and the process continues to Step (3); or
(b) if the MRCA accepted condition does not contribute at least five impairment points then the claim is rejected.
Step (3) If compensation may be payable, work out the amount of compensation that would be payable under the MRCA for the VEA and/or SRCA accepted conditions referred to in Step 1 as at the date of the MRCA determination, using GARP M, as if those conditions were compensable under the MRCA.
Step (4) Reduce the amount worked out under Step (1) by the amount worked out under Step (3).
Step (5) The amount worked out at Step (4) is the amount payable under the MRCA subject to the proviso in Step (6).
Step (6) The amount payable cannot take the total sum of:
(a) the amount worked out under Step (4); and
(b) the amount worked out by using the VEA percentage to calculate the notional equivalent amount of disability pension payable using the General Rate payable at the date of the determination; and
(c) SRCA section 24, 25 and 27 lump sum amounts paid for the SRCA conditions referred to in Step 1 (the SRCA payments being converted as set out below);
above the maximum weekly payment of MRCA Permanent Impairment) at the date of the determination. If the proviso applies go to Step (7).
Step (7) If the proviso in Step (6) applies the MRCA compensation payment is worked out as follows:
(a) excess MRCA PI equals the amount worked out in Step 6(b) plus SRCA section 24, 25 and 27 lump sums converted to periodic payments plus Step (4) amount minus maximum MRCA PI rate.
(b) amount of weekly MRCA PI payable is equal to Step (4) amount minus excess PI under (a).
Conversion of SRCA lump sums
In order to work out the net MRCA periodic payment for Step (7), lump sums paid to the person under SRCA sections 24, 25 and 27 that a person has received must be converted to a periodic payment.
The SRCA amounts are converted to a current lump sum value (by multiplying by the ratio of the current value for maximum SRCA section 24 payment to the value when the lump sum payment was made) and each lump sum converted to a periodic payment by dividing by an age-based number provided by the Australian Government Actuary for this purpose. The age to be used in applying this age-based number is the age that the person would have been on their next birthday at the time the SRCA lump sum was paid. The converted amount is indexed annually (on 1 July) using the indexation factor calculated under section 404 of the MRCA.